Physiotherapy using muscle strengthening and stretching exercises is claimed to have beneficial effects in the treatment of Legg-Calvé-Perthes disease; however, no scientific evidence is available concerning effectiveness of treatment.
PURPOSE:The purpose of the present study was to clinically evaluate possible effects of the proposed physiotherapeutic effects compared to observational follow-up in patients with Legg-Calvé-Perthes disease.
METHOD:A prospective follow-up study was conducted in 17 patients with unilateral Legg-Calvé-Perthes disease, divided into 2 groups: Group A (observational follow-up) and Group B (physiotherapeutic follow-up). In order to evaluate the outcome of the adopted treatments, the following parameters were assessed: articular range of motion, level of muscular strength, level of articular dysfunction, and radiographic status, both before and after the treatment.
RESULTS:Group B exhibited significant improvement in articular range of motion concerning hip flexion, extension, abduction, adduction, medial rotation, and lateral rotation, while in Group A an equally significant worsening occurred concerning abduction, adduction, and medial rotation. Muscular strength also improved in Group B, mainly in the set of hip flexor muscles, while Group A showed no changes. Articular dysfunction after therapy compared to pretherapy was significantly reduced in Group B and increased in Group A. Patients undergoing physiotherapy exercises showed no changes in their radiographic features.
CONCLUSION:Physiotherapy produced significant improvement in articular range of motion, muscular strength, and articular dysfunction in patients with Legg-Calvé-Perthes disease, but these improvements were not evident on radiographs.
A fisioterapia por meio de exercícios de fortalecimento e alongamento muscular é citada no tratamento de pacientes com doença de Legg-Calvé-Perthes; entretanto não há evidência científica sobre a efetividade do tratamento.
OBJETIVO:O objetivo do trabalho foi avaliar clinicamente os possíveis efeitos dos exercícios fisioterapêuticos propostos em comparação com o acompanhamento observacional dos pacientes com doença de Legg-Calvé-Perthes.
MÉTODO:Foi realizado um estudo prospectivo com 20 pacientes com doença de Legg-Calvé-Perthes unilateral, divididos em dois grupos: grupo A, acompanhamento observacional e grupo B, acompanhamento fisioterapêutico. Para avaliação dos resultados dos tratamentos adotados, foram avaliados os parâmetros: amplitude de movimento articular, grau de força muscular, grau de disfunção articular e quadro radiográfico, pré e pós-tratamento.
RESULTADOS E DISCUSSÃO:Houve no grupo B uma melhora estatisticamente significativa da amplitude de movimento articular para a flexão, extensão, abdução, adução, rotação medial e rotação lateral do quadril, enquanto no grupo A ocorreu uma piora, também significativa, da abdução, adução e rotação medial. A força muscular também melhorou no grupo B, principalmente no grupo dos flexores quadril, enquanto no grupo A não houve alteração. O grau de disfunção articular apresentou, em média, uma melhora estatisticamente significativa no grupo B e uma piora no grupo A em relação aos períodos pré e pós-tratamento. Os pacientes submetidos aos exercícios fisioterapêuticos não apresentaram modificação do quadro radiográfico.
The management of Legg-Calvé-Perthes disease (LCPD) has advanced since its first description, but it remains controversial.1 The main objective of treatment is to maintain the hip joint morphology in its best possible condition in order to prevent early degeneration, while preserving the joint mobility with pain relief.2,3 So far, however, there is no consensus regarding the best form of conservative treatment and during which stage of the disease should it be applied.
It is not clear what would be the possible benefits from physiotherapy in LCPD or when should it be used. Some studies mention physiotherapy as a pre- and/or postoperative resource,4–7 while others consider it a form of conservative treatment associated with other treatments, such as skeletal traction, orthesis, and plaster cast.3,8–11
According to Herring et al, literature includes 1 randomized study and a few controlled studies, most of them without control groups.12,13
Wild et al14 suggest that a study should be conducted in patients with LCPD scored as I or II in the Catterall radiographic classification and/or as A in the Salter-Thompson radiographic classification; such patients would then undergo 3 to 4 months of physiotherapeutic treatment, with clinical and radiographic control evaluations.
The hypothesis to be tested in this study was that physiotherapy exercises as a modality of conservative treatment for LCPD provide significant functional improvement compared to observation alone. The design of the study was to clinically evaluate the possible effects of the proposed physiotherapy exercises in comparison with observational follow-up in patients with LCPD.
CASES AND METHODSThis was a prospective, parallel-group controlled study of 20 patients of both genders with unilateral LCPD conducted between November 2003 and September 2005 at the Institute of Orthopedics and Traumatology and approved by the Institutional Ethics Committee. Patients presenting with an indication for conservative treatment were divided into 2 groups: A (control group) and B (physiotherapy group). The division of the groups was made according to the patients’ availability: the patients available to attend the Institute twice a week were included in Group B and those who did not have this availability were included in Group A.
The patients were included in this study according to the following criteria: diagnosis as LCPD, no other associated lesion in the hip, no surgery undergone in the hips, unilateral involvement by the disease, indication for conservative treatment, and no neurological disturbance with cognitive alterations. The patients in Group B must have been available to attend the Institute twice a week to participate in physiotherapy sessions.
Patients excluded from the study were those who ceased treatment, who were not available for revaluation, who needed to undergo a surgical procedure, or who failed to attend treatment for more than 2 consecutive times. Two patients were excluded from Group B—one was absent more than 2 consecutive times and the other underwent a surgical procedure—and 1 patient who was not available for revaluation was excluded from Group A. Therefore, 17 patients completed the study out of the 20 initially included patients.
Group AGroup A consisted of 9 patients (8 boys and 1 girl, aged 3.3 to 7.5 years, (mean, 5.6 years) (Table 1). Seven patients presented with affected left hips and 2 with affected right hips, with dominant left sides in 5 patients and dominant right sides in 4. Only 1 patient was Black, while the others were Caucasians. Concerning radiographic classifications, 7 were Catterall Type II patients, and 2 were Catterall Type III patients; 2 were Herring Type A patients, and 7 were Herring Type B patients; 4 were Salter-Thompson Type A patients, but this classification could not be used for the other patients (see Table 1).
Distribution of the patients in groups A and B, according to sample size, gender, affected hip, dominant side, race, and radiographic classification (Catterall, Herring, and Salter-Thompson)
| Group | n | Gender | Affected hip | Dominant side | Race | Catterall | Herring | Salter-Thompson |
|---|---|---|---|---|---|---|---|---|
| A | 9 | Boys 8 | Left 7 | Left 5 | Black 1 | Type II 7 | Type A 2 | |
| Girls 1 | Right 2 | Right 4 | Caucasian 8 | Type III 2 | Type B 7 | Type A 4 | ||
| B | 8 | Boys 7 | Left 6 | Left 2 | Black 1 | Type I 2 | Type A 3 | |
| Type II 4 | Type A 3 | |||||||
| Girls 1 | Right 2 | Right 6 | Caucasian 7 | Type III 2 | Type B 5 |
n: sample size
Group A was subjected to a 12-week observational follow-up with no therapeutic intervention.
Group BGroup B consisted of 8 patients (7 boys and 1 girl), aged 3.5 to 7.4 years (mean, 5.7 years) (see Table 2). Six patients presented with affected left hips, and 2 presented affected right hips, with dominant right sides in 6 patients and dominant left sides in 2. Only 1 patient was Black, while the others were Caucasians. Concerning radiographic classifications, 2 were Catterall Type I patients, 4 were Catterall Type II, and 3 were Catterall Type III; 3 were Herring Type A patients, and 5 were Herring Type B patients; 3 were Salter-Thompson Type A patients, but this classification could not be used for the other patients.
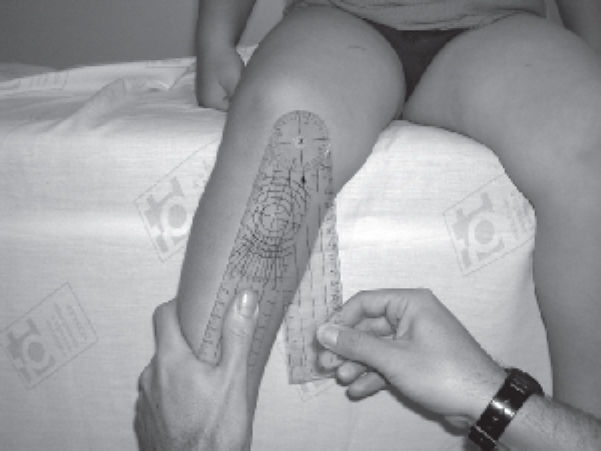
Group B received physiotherapeutic treatment twice a week for 12 weeks. The treatment proposed included passive exercises for musculature stretching of the involved hip (Figure 1). Stretching was repeated 3 times for each exercise modality and maintained for 20 seconds. Straight leg raise exercises were undertaken to strengthen the musculature of the hip involved for the flexion, extension, abduction, and adduction of muscles of the hip. They started with three 20-second sets of isometric exercises, and after the eighth session, concentric exercises were introduced, with 3 sets of 10 repetitions each. The balance training started during the fifth session, initially on stable terrain and later on unstable terrain.
An analysis of probability of occurrence of categories was performed in the population. They were compared using the verisimilitude ratio test, and similar groups were determined in terms of age (P = 0.956), gender (P > 0.999), race (P = 0.596), affected hip (P = 0.081), dominant side (P > 0.999), and Catterall (P = 0.170) and Herring (P = 0.490) classifications.
Evaluation criteriaPatients were clinically evaluated in affected and nonaffected lower limbs before and 12 weeks after the treatment. The same physician performed all clinical evaluations, which consisted of 3 parts: articular range of motion, muscular strength, and articular dysfunction.
The evaluation of the hip range of motion was measured in passive flexion, extension, abduction, adduction, medial rotation (Figure 2), and lateral rotation movements of the hip, using a manual goniometer.
Muscular strength was evaluated using a 0 to 5 scale, where a 0 point score corresponds to no muscular contraction experienced; 1 point meant that the muscular contraction was noticed and did not produce articular movement; 2 points meant that motion was produced only if the force of gravity was suppressed; 3 points, when the muscle contracted and moved the segment against the force of gravity; 4 points, when the muscle moved against the force of gravity, but supported little counterresistance only; and 5 points, when the muscle moved against the force of gravity and against an additional resistance.15 The findings were compared to those of the nonaffected contralateral hip. In order to evaluate the level of muscular strength, a muscular function test for movements of the hip joints was applied.
Spósito et al16 created a scale to evaluate the level of articular dysfunction that was used in this study, where 1 point was assigned to every 5 degrees of discrepancy from the normal pattern of the nonaffected hip, and 1 point to each level of muscular strength discrepancy for the tested groups, always comparing the result with the nonaffected side. The sum of scores obtained, before and after treatment, was performed to compare the groups.
The first and last radiographs were studied for changes that occurred in the radiographic status.
Statistical analysisThe descriptive analysis of parameters number of cases (n), mean, standard deviation (SD), minimum, median, and maximum was performed. For range of motion, which are quantitative ordinal parameters, an inferential analysis was performed using ANOVA with repeated measurements. The differences between the 2 limbs were considered and the Bonferroni method was applied. The inferential analysis of hip muscular strength level was performed using McNemar’s test. The level of articular dysfunction was analyzed using ANOVA with repeated measurements, and the paired mean values were compared using the Bonferroni method. A significance level of P < 0.05 was used throughout the analysis. The analysis was performed using the Minitab® Statistical Software Release 14 software (Copyright ©2005 Minitab Inc, State College, PA, USA).
RESULTSArticular range of motionThe means of differences between the affected and nonaffected hips were compared between Groups A and B and between the pre- and post-treatment periods.
In Group B, the analysis of flexion, extension, medial rotation, and lateral rotation of the hip showed that the mean values of the differences between the affected and nonaffected hips were higher before than after the treatment period (P < 0.001, P = 0.020, P < 0.001), and P = 0.028, respectively). In Group A, the analysis of flexion, extension, medial rotation, and lateral rotation showed no difference, the mean values of the differences were equal before and after the treatment period.
In Group A, the analysis of hip adduction showed that the mean value of the difference between the affected and the nonaffected hip was higher after follow-up than before the follow-up (P = 0.002). However, in Group B this ratio was reversed and, according to the hip adduction analysis, the mean of the difference between the affected hip and nonaffected hip was higher before the treatment than after the treatment (P = 0.002). The differences detected in abduction and adduction were similar. Group A showed a higher postfollow-up mean difference (P = 0.005) and Group B showed a higher pretreatment mean difference (P < 0.001), that is, the mean differences between the 2 limbs decreased with treatment.
In Group A, the posttreatment analysis of flexion, adduction, abduction, and medial rotation show that the mean differences between the affected and nonaffected hips were higher as compared with those in Group B (P = 0.007, P = 0.044, P < 0.001, and P < 0.001, respectively). In the pretreatment period, however, this ratio had been the opposite, in the analysis of flexion, adduction, abduction, and medial rotation: the mean differences in Group B were higher than in Group A (P = 0.010, P = 0.002, P < 0.001, and P = 0.008, respectively). Only for the lateral rotation, the mean range of motion of the groups did not show a statistical difference (P = 0.167).
Based on these results, we reevaluated, whenever necessary, the means of the differences and generated the 95% confidence intervals (Table 3).
Mean values and 95% confidence intervals for differences between affected and nonaffected members, per group and per period
| Variable | Group | Period | Mean | 95% Confidence Interval | |
|---|---|---|---|---|---|
| Flexion | A | Pre and Post | 6.11 | 1.01 | 11.21 |
| B | Pre | 10.63 | 2.75 | 18.50 | |
| Post | 1.25 | -0.69 | 3.19 | ||
| Extension | A | Pre and Post | 1.02 | -0.18 | 2.24 |
| B | Post | ||||
| B | Pre | 2.50 | 0.06 | 4.94 (*) | |
| Adduction | A | Pre | 3.89 | -0.31 | 8.09 |
| Post | 7.78 | 1.97 | 13.57 | ||
| B | Pre | 7.50 | 3.03 | 11.97 | |
| Post | 1.88 | -1.23 | 4.99 | ||
| Abduction | A | Pre | 7.78 | 3.43 | 12.12 |
| Post | 12.22 | 8.83 | 15.61 | ||
| B | Pre | 13.75 | 7.52 | 19.97 | |
| Post | 4.37 | -1.23 | 4.98 | ||
| Medial Rotation | A | Pre and Post | 2.5 | 0.10 | 4.90 |
| B | Post | ||||
| B | Pre | 11.87 | 6.43 | 17.32 | |
| Lateral Rotation | A | Pre and Post | 4.70 | 2.10 | 7.31 |
| B | Pre | ||||
| B | Post | 2.50 | -0.66 | 5.66 | |
Pre: pretreatment; Post: posttreatment; (*) 90% confidence interval
In the pre-treatment period, 7 patients of Group B rated 4 points at the evaluation of muscular strength of the affected hip and one patient rated 5 points. However, in the post-treatment period all patients (8) had improved to 5 points.
Group B showed an improvement in the strength of abduction muscles in relation to periods (P = 0.016). The contralateral hip muscular set showed no statistical differences between groups and periods.
Articular dysfunctionThe descriptive statistical values for the level of articular dysfunction are described in Table 4. Using the Bonferroni method, it was found that in Group A, the pretreatment mean value was lower than after the postfollow-up mean (P < 0.001), and in Group B the pretreatment mean value was higher than the posttreatment mean (P < 0.001). In the pretreatment period, the mean value was higher in Group B than in Group A (P = 0.024). This relation was reversed in the posttreatment period; the mean value was higher in Group A than in Group B (P = 0.020).
Descriptive statistics for the degree of hip joint dysfunction in pre- and posttreatment periods and for the difference between periods, in groups A and B
| Group | n | Mean | SD | Minimum | Median | Maximum | |
|---|---|---|---|---|---|---|---|
| Pre | A | 9 | 6.3 | 4.5 | 1 | 6 | 16 |
| B | 8 | 13.3 | 4.3 | 6 | 14 | 18 | |
| Post | A | 9 | 9.8 | 4.9 | 4 | 9 | 21 |
| B | 8 | 3.5 | 2.1 | 0 | 3 | 7 | |
| Pre and Post | A | 9 | -3.4 | 1.8 | -7 | -3 | -1 |
| B | 8 | 9.8 | 2.7 | 6 | 11 | 13 |
Pre: pretreatment; Post: posttreatment; n: sample size; SD: standard deviation
The ages of the study groups were statistically equal, with a mean age of 5.6 years in Group A and 5.7 years in Group B. Martinez et al17 present in their study a mean age of 6 years, while Tsao et al18 present a mean age of 4.4 years.
The ratio between males and females has been frequently reported as 4:1.19–22 The groups in this study were equal concerning the proportion of female patients: 11.1% for Group A and 12.5% for Group B. However, these data do not agree with generally reported findings, although 1 study performed at our institution reported 9.8% female patients;23 however, other studies also conducted in our environment, although in different institutions, reported higher proportions of female patients (20% and 33.3%).23,24 Thus, it is possible that in this study center, the incidence of the disease among females is lower.
Caucasians prevailed as follows: 77.8% in Group A and 87.5% in Group B. In 2 studies conducted in our environment, Caucasians prevailed among 9 patients, numbering 8 (88.9%)25 and in another study with 43 patients, this number was 41 (95.35%).26 It was seen in this sample that, although it was considered statistically equal, the incidence of Blacks was higher than in other studies conducted in our environment. This may be related to the small number of cases.
According to Wenger et al,27 the involvement of the left and right hips in LCPD is approximately the same. In this study, Group A had 66.7% affected right hips, while Group B had 75% affected left hips.
In both groups there was a higher, but not statistically significant, proportion of patients with dominant right sides (55.6% in Group A and 75% in Group B.) We could not find data in literature relating the affected hip with the dominant side in patients with LCPD.
One of the early symptoms of LCPD is pain and/or claudication. Pain may be located in the hip, although it is normally reported in the medial region of the thigh or knee.28 During clinical examination, patients with LCPD may also present positive signs in the Trendelemburg test29; reduction in the hip range of motion, mainly in abduction, flexion, and medial rotation, which may lead to hypothrophy or atrophy of the thigh for lack of use of the limb28; failure of abductor muscles due to increased growth of the greater trochanter9; and muscular flexion and abduction contracture of the hip.18 Therefore, it is important to measure the range of motion and the level of muscular strength of the hip,22,28–30 because the results of treatment are directly related to the hip range of motion; a good outcome is when the patient has no symptoms and total hip range of motion.19 Thus, the reduction of hip range of motion may be one of the first signs of subluxation.31
To classify the disease stages and prognosis, the main radiographic classifications used are Catterall,19 which classifies the stages of LCPD according to radiographic findings into 4 types, depending on the extent of the injury of the femoral epiphysis; Salter and Thompson,32 who created a classification based on a radiographic sign of subchondral lysis (fracture) divided into 2 types, A and B; Herring et al,2 based on the height of the lateral pillar of the epiphysis in the fragmentation phase, subdividing the hips into 3 groups: A, B, and C. Later, Herring et al2 modified the original classification of the lateral pillar and subdivided it into 4 groups: A, B, B/C, and C. We used the classification of Herring et al described in 1992,12 because the new classification was described after the beginning of this study. In the present study, patients of groups A and B presented radiographic indications for conservative treatment.
There are many forms of conservative treatment, and the earlier the treatment is started, the better the prognosis.33 However, few studies have the purpose of evaluating the benefits of physiotherapy in LCPD. Most use physiotherapy as a resource in association with other treatments, although they do not directly evaluate its benefits.13
The analysis of the articular range of motion of Group B showed that, on average, all movements studied had significant improvement when pre- and posttreatment periods were compared. No improvement was shown in Group A in terms of pre- and posttreatment periods; all movements remained the same or worsened. In general, in Group B, the mean pretreatment difference between the affected and nonaffected hip was higher than in Group A. However, in the posttreatment period, this ratio was reversed: in Group A the mean posttreatment difference between affected and nonaffected hips was higher than in Group B. This clearly shows that Group B had improved and Group A had worsened. Only a few published studies report values of articular range of motion, and usually the reported values correspond to patients who underwent reevaluations many years after treatment, mostly on the occasion of surgical treatment. Some reports stress the importance of physiotherapy in LCPD, with exercises to maintain or acquire hip range of motion and reduce muscular spasms.12 These reports describe physiotherapy exercises and resources to be used by patients with LCPD, such as active-assisted exercises, active exercises and active-resistive exercises, proprioceptive neuromuscular facilitation (PNF), cryotherapy, and hydrotherapy, although they do not evaluate them.28 Some case reports show how physiotherapy works in LCPD and evaluate it, but only in patients who used physiotherapy as a resource associated with surgical or other conservative treatment.34
Since the level of muscular strength of the nonaffected limb for all individuals of both groups and in both periods was considered equal to 5, we did not perform a statistical analysis of the variables of the nonaffected limb. It was observed that the levels of muscular strength assumed by the variables corresponded to responses equal to 4 or 5. Data on the level of hip muscular strength showed improvement in the values concerning the level of muscular strength in Group B, with a significantly higher incidence of a score equal to 5 in the posttreatment than in the pretreatment evaluations for abductor hip muscles. Probably these were the most weakened muscles before the treatment. Medial and lateral rotation muscles were also shown to be weakened before the treatment; however, Group B was not subjected to strengthening exercises concerning these sets of muscles, and even though patients of this group underwent stretching exercises, they had a small, nonsignificant improvement. The distribution of other responses was the same pre- and posttreatment. Thus, in Group A, the score distribution was the same pre- and posttreatment. Only a few studies mention having evaluated the level of muscular strength,16 but it was not possible to compare them with the levels of muscular strength found in the present study.
On the average, the level of articular dysfunction improved in Group B and worsened in Group A in terms of treatment periods. In Group A the pretreatment mean value was significantly lower than after the treatment, and in Group B the pretreatment mean value was significantly higher than after the treatment.
Spósito et al16 found the following mean pretreatment values of articular dysfunction level: in Group I, Catterall Type II patients scored 8.8 points and Type III patients scored 22.5 points, while in Group II, Type II patients scored 18.8 points and Type III patients scored 16 points. In the present study, the pretreatment mean value was 6.3 in Group A and 13.3 in Group B. This shows that the radiographic condition did not always correspond to the level of articular dysfunction, since in Group B of this study, whose patients were less affected as shown radiographically (Catterall Type I), the mean level of articular dysfunction was higher than in Group A. As in Group II of Spósito et al,16 Catterall Type III patients scored 16 points, versus the 18.8 points scored by Catterall Type II patients. However, posttreatment results cannot be compared because treatment procedures and times were quite different.
Patients of the 2 study groups did not present changes in their radiographic conditions and will be followed-up for future analyses.
The most important finding in this study was that the exercises proposed for Group B were effective for improving both the articular range of motion and the level of muscular strength of the affected hip when compared with Group A. The physiotherapeutic treatment employed in Group B was effective for patients with LCPD who presented with an indication for conservative treatment.