The aim of this study was to review the literature on cervical spine fractures.
METHODS:The literature on the diagnosis, classification, and treatment of lower and upper cervical fractures and dislocations was reviewed.
RESULTS:Fractures of the cervical spine may be present in polytraumatized patients and should be suspected in patients complaining of neck pain. These fractures are more common in men approximately 30 years of age and are most often caused by automobile accidents. The cervical spine is divided into the upper cervical spine (occiput-C2) and the lower cervical spine (C3-C7), according to anatomical differences. Fractures in the upper cervical spine include fractures of the occipital condyle and the atlas, atlanto-axial dislocations, fractures of the odontoid process, and hangman's fractures in the C2 segment. These fractures are characterized based on specific classifications. In the lower cervical spine, fractures follow the same pattern as in other segments of the spine; currently, the most widely used classification is the SLIC (Subaxial Injury Classification), which predicts the prognosis of an injury based on morphology, the integrity of the disc-ligamentous complex, and the patient's neurological status. It is important to correctly classify the fracture to ensure appropriate treatment. Nerve or spinal cord injuries, pseudarthrosis or malunion, and postoperative infection are the main complications of cervical spine fractures.
CONCLUSIONS:Fractures of the cervical spine are potentially serious and devastating if not properly treated. Achieving the correct diagnosis and classification of a lesion is the first step toward identifying the most appropriate treatment, which can be either surgical or conservative.
The most common causes of cervical spine injury are automobile accidents, followed by diving into shallow water, firearm injuries, and sports activities (1,2). There is a bimodal age distribution among patients with spinal cord injuries: the first peak occurs in patients between 15 and 24 years, and the second in patients over 55 years of age (2-4).
Occipital condyle fracturesExtension of the upper part of the cervical spine is limited mainly by the transverse portion of the alar ligaments. When flexion is added to the head rotation, the alar ligament is maximally dilated and the cervical spine becomes more vulnerable to injury (5).
The first description of occipital condyle fractures in the literature was provided by Bell (6) in 1817, and the second was not published before 1900 (7). Further cases were published from 1962 (8-11) to 1978 (12), with this type of fracture characterized as very rare.
Fractures of the occipital condyle require conservative treatment. Outcomes are favorable if there are no other associated injuries, such as those caused by cranioencephalic trauma or cervical vertebral fractures (13).
In general, this type of fracture is caused by accidents involving high-energy traumas, such as sports-related injuries and, in the vast majority of cases, automobile accidents (12). In addition, these fractures generally affect younger individuals in the second and third decades of life, particularly males (12).
In 1987, Dvorak and Panjabi (5) published their study on the functional anatomy of the alar ligaments, and in 1988, Anderson and Montesano (13) proposed a classification for fractures of the occipital condyle according to the regional anatomy, biomechanics of the structures involved, and fracture morphology. Three types of occipital condyle fractures have been described. Type I is an impact fracture of the occipital condyle for which the trauma mechanism is the axial load of the skull on the atlas. In this fracture, there is communication of the occipital condyle with or without minimum deviation of the fragments toward the foramen magnum. The tectorial membrane remains intact, as does the alar ligament contralateral to the fracture, which ensures the fracture's stability. Type II fractures are part of a cranial base fracture that causes a fracture line extending towards the foramen magnum. This fracture is caused by direct regional trauma and is stable because the alar ligaments and the tectorial membrane remain intact. In type III fractures, there is a fracture-avulsion of the occipital condyle by the alar ligament, which is caused by a rotation of the head, a lateral tilt of the head, or both movements together. In this case, because the contralateral alar ligament and the tectorial membrane do not remain intact, the injury is potentially unstable.
The clinical signs of occipital condyle fractures are highly non-specific, which makes diagnosis difficult. The patient generally only complains of pain on the posterior side of the neck and cervical paravertebral muscle spasms (10). Because specific exams are needed to diagnose these fractures, they often go unnoticed. The patient may present with persistent pain in the posterior cervical region accompanied by muscle spasms over long periods, without ever suspecting that there is an injury (11,12). These fractures are extremely difficult to detect using conventional radiographic techniques, so the use of other methods is necessary. Computed tomography (CT) is the preferred examination method (11,12). The occipitocervical transition should be carefully evaluated, particularly in patients with associated facial and cranial traumas (11,12).
Cranioencephalic trauma occurs in the vast majority of patients with these fractures, which contributes to the clinical symptoms of these patients, making diagnosis difficult and often leading to death. There is a possible association of these injuries with fractures of the cervical vertebrae, and occipital condyle fractures are often mistakenly diagnosed as cervical vertebral fractures (11,12).
Conservative treatment of occipital condyle fractures results in good outcomes; the patient becomes free of neck pain, and full range of motion of the segment involved can be regained after three months of treatment. The use of a Philadelphia cervical collar is recommended for cases categorized as type I or II in the Anderson and Montesano classification, and a more rigid immobilization, such as a halo brace or Minerva cast for 12 weeks, is recommended in the case of type III fractures. If radiographic images indicate instability after an appropriate period of immobilization with a halo brace, occiput-C2 arthrodesis may be necessary (13,14).
C1 and C2 fractures and dislocationsAtlas fracturesAtlas fractures represent 2% of all vertebral spine fractures (15) and occur when an axial (vertical) compression of the skull on the atlas forces it onto the axis, resulting in a rupture at the weakest points (the anterior and posterior arches) and causing the lateral masses to split; this is known as a Jefferson fracture (15).
Pressure exerted on the atlas may lead not only to fracture of the arches but also to rupture of the transverse ligament, which is the main structure that gives this vertebra its anterior stability and prevents it from slipping on the axis (5). Thus, in Jefferson fractures, the status of the transverse ligament is essential to the prognosis.
The diagnosis of an atlas fracture is made by observation of the C1-C2 joint in frontal radiographs. Normally, there should be continuity of the vertical line traced on the lateral margins of the lateral masses of the atlas and of the joint masses of the axis; however, when there is a fracture of the anterior and posterior arches of the atlas, this continuity disappears due to splitting of the lateral masses.
It has yet to be determined how much of a separation is consistent with the integrity of the transverse ligament. Experimental studies on cadavers (14) have demonstrated that if the separation is greater than 7 mm, rupture of the ligament has occurred with C1-C2 instability, which continues even after consolidation of the arch fractures and results in a greater risk of C1-C2 dislocation; this is also true for small traumas (5).
The treatment indicated for Jefferson fractures is reduction by cranial traction and immobilization for three to four months. However, in cases where there is rupture of the transverse ligament, immediate occipito-cervical arthrodesis is necessary.
Sometimes, routine radiographic study of the Jefferson fracture only reveals a fracture of the posterior arch, while a fracture of the anterior arch only appears on CT scans.
Atlas-axis dislocationPatient survival following dislocations between the occiput and the atlas is rare. We do not have any personal experience with these cases, and there have been very few reports in the literature (14). Pure C1-C2 dislocations, i.e., without fracture of the odontoid process, are also rare because they can only be caused by a violent flexion mechanism with rupture of the transverse ligament, projection of the odontoid dens to the neural canal, and spinal cord trauma that is generally incompatible with life.
Subluxations determined by existing instability are more common, as in dysplasias of the odontoid dens and rheumatoid arthritis (16). We should also differentiate between this and other types of injury, such as Grisel's syndrome, in which a fixed rotatory subluxation of C1-C2 can be observed, which is of an inflammatory origin and with a distinct previous history.
Radiographic diagnosis of a C1-C2 dislocation is typically made in the profile view, in which the distance between the posterior margin of the anterior arch of the atlas and the anterior margin of the odontoid peg is greater than 3 mm in adults or 5 mm in children. If there is uncertainty, the recommendation is to conduct radiographic imaging in the profile view, in both flexion and extension; normally, there should be no significant difference in the distance. In this dynamic study, especially when a dislocation is suspected, precautions should be taken; for example, complaints of pain should be interpreted as a limitation of movement, and the exam should not be performed on unconscious patients (11).
In cases of C1-C2 dislocations, the treatment should always be surgical. C1-C2 arthrodesis can be performed using various methods: wire fixation between the posterior arches of C1-C2; transarticular fusion of C1-C2 (Magerl technique); the Harms technique, in which a screw is placed in the lateral mass of C1 and in the pedicle of C2; or the Wright technique, in which a screw is placed in the lateral mass of C1 and intralaminarly in C2 (17). Recent anatomical studies show that, with more modern techniques, surgical treatment is even a possibility in children (18).
Odontoid dens fracturesOdontoid dens fractures represent 5 to 15% of cervical spine fractures. The mechanism of these fractures is not clear (19), but biochemical studies suggest that they are caused by shear forces (19).
If there is a hyperflexion component to the fracture, then an anterior deviation with anterior dislocation of the atlas can occur. This injury is known as a C1-C2 fracture dislocation. In this case, there is a higher possibility of spinal cord integrity than in pure dislocation; therefore, the probability of survival is greater.
If the odontoid dens fracture occurs by hyperextension, there may be posterior deviation (19). In radiographic studies of fractures without deviation, whether in the anteroposterior or profile views, only the fracture line of the odontoid peg fracture will be visible, whereas in fractures with deviation, the fracture will be visible with deviation of the distal fragment and dislocation of the atlas. In fractures without deviation, it is sometimes very difficult to see the fracture line, and diagnosis is only possible with CT imaging.
Special care should be taken with children when performing a radiological diagnosis of fractures without deviation because vertebral ossification is incomplete. In radiographs of children, the odontoid process and the body of the axis are separated by a strip of tissue that is transparent to X-rays. This strip of tissue becomes progressively narrower until it disappears in 10-11-year-olds (19,20).
Anderson and D'Alonzo (19) created a classification linking the height of the line with the fracture prognosis:
Type I: fracture of the upper part of the odontoid dens;
Type II: fracture at the base of the odontoid dens; and
Type III: fracture affecting the body of the axis.
Treatment is guided by the type of odontoid fracture (19-22). Type I fractures that do not involve injury to the ligament structures supporting the atlanto-occipital joint can be treated with cervical arthrodesis for three months. There is some debate as to the best treatment of type II fractures due to the documented poor potential for consolidation of the fracture in elderly patients and the known morbidity associated with prolonged treatment with a halo brace (19-22).
Relative indications for surgery include the following (20-22):
- •
A more than 5-mm fracture dislocation;
- •
A more than 10-degree angulation;
- •
Failed attempts at closed reduction.
In fractures requiring surgical treatment, an alternative is osteosynthesis with the use of a cannulated screw. In this technique, a radioscopy-guided anterior incision is made at C4-C5 with dissection and placement of a guide wire in the inferior cortex of C2. A cannulated screw is then inserted with the assistance of simultaneous images in the anteroposterior and profile views (19-22). Contraindications for this technique include the following: osteoporosis, comminuted fractures, unfavorable fracture line angulation (oblique anterior line), diastasis of the fragments, and pseudoarthrosis.
Hangman's fractureTraumatic spondylolisthesis of the axis, also known as hangman's fracture, is the typical fracture resulting from hyperextension-distraction in which there is a fracture of the pedicle of C2 with dislocation of the body of this vertebra on C3 (23). This fracture, despite the major dislocation of C2 on C3 that often occurs, rarely leads to spinal cord injury because it causes the canal to widen rather than narrow (23).
The Levine and Edwards classification (24) divides traumatic spondylolisthesis of the axis into four types:
Type I: fracture without an angular deviation and translational deviation of less than 3.5 mm that occurs due to hyperextension and axial compression;
Type II: fracture with a significant translational or angular deviation that occurs due to hyperextension and axial compression combined with a mechanism of flexion-compression;
Type IIa: fracture with a small translational deviation and wide angulation, with an increase in posterior disc space between C2-C3 upon application of traction that occurs due to a flexion-distraction; and
Type III: fracture with a large translational and angular deviation, which is associated with unilateral or bilateral dislocation of the C2-C3 joint facets and occurs due to a flexion-compression mechanism.
Type I fractures are stable injuries and can be treated with the use of a neck brace, halo-cast, halo-vest, or Minerva cast for a period of 12 weeks. Type II fractures are unstable injuries, and the mechanism by which the fracture is produced requires a reduction through distraction and slight hyperextension with posterior immobilization and application of a halo-cast for 12 weeks. In type IIa fractures, cranial traction is indicated so that reduction can be achieved by means of slight compression and extension, as flexion-distraction is the probable injury mechanism. These fractures should be treated with a halo-cast for 12 weeks or surgically stabilized by means of C2-C3 anterior arthrodesis or transpedicular fixation of C2. Surgical treatment is indicated in type III fractures and is aimed at reduction of the joint facets and stabilization by arthrodesis (24).
Lower cervical spine fracturesPreviously, the most commonly used classifications of cervical fractures were those of Allen-Ferguson (25) and the AO. More recently, the SLIC classification (26) has added neurological status as another factor to consider.
The Allen-Ferguson classification was one of the first classifications to be used, but its importance today is only historical. It divides injuries into six types (23): compression-flexion, vertical compression, distraction-flexion, compression-extension, distraction-extension, and lateral flexion (25).
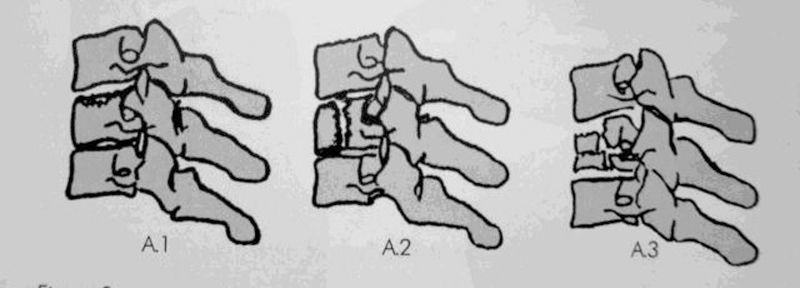
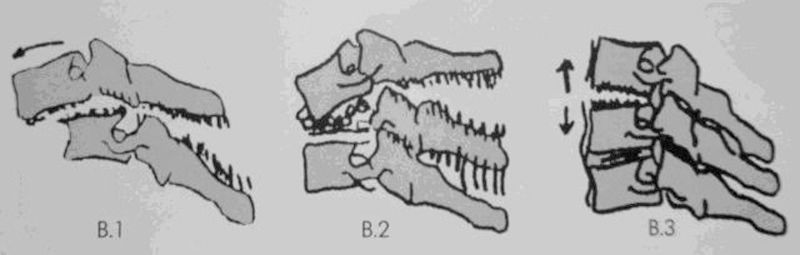
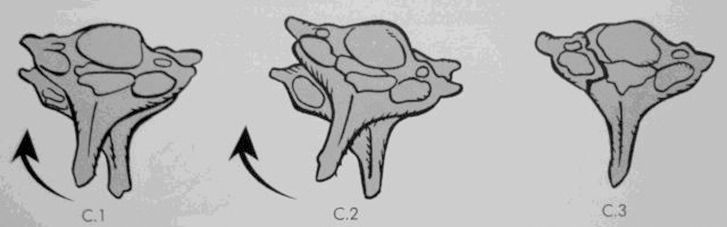
Still widely used by various centers, the classification of lower cervical fractures recommended by the AO group consists of three types (A, B and C), which are extended into groups and subgroups. The types describe the trauma mechanism (A: compression; B: distraction; C: rotation), while the groups and subgroups define the morphological parameters. This classification represents a ranking that follows a prognostic hierarchy, i.e., as one progresses through the classification, the severity becomes theoretically higher and the prognosis worsens. The AO classification of fractures of the lower cervical spine (C3-C7) (27) is shown in Figures 1 to 3.
The Subaxial Injury Classification (SLIC) Scale was created to remedy the lack of consensus among classification groups. To create the scale, a systematic review of the surgical treatment of lower cervical spine trauma was conducted, and a treatment algorithm was created with the evidence-based consensus of a group of specialists (26). This classification of lower cervical spine injuries takes into account the following characteristics:
- 1.
Morphology;
- 2.
Status of the disco-ligamentous complex; and
- 3.
Neurological assessment.
Based on these parameters, a table is used to assign scores to each injury: individuals with a score lower than 4 do not require surgical intervention; a score of 4 means the treatment could be either surgical or conservative (often, the decision is made based on the personal experience of the surgeon); and a score higher than 4 normally means that surgical intervention is required (26) (Table 1).
Subaxial Injury Classification (SLIC) scale.
| Points | |
|---|---|
| Morphology | |
| No abnormality | 0 |
| Compression + burst | 1 + 1 = 2 |
| Distraction (e.g., facet perch or hyperextension) | 3 |
| Rotation or translation (e.g., facet dislocation, unstable teardrop, or advanced-stage flexion-compression injury) | 4 |
| Disc-ligamentous complex | |
| Intact | 0 |
| Indeterminate (e.g., isolated interspinous widening or MRI signal change only) | 1 |
| Disrupted (e.g., widening of the anterior disk space or facet perch or dislocation) | 2 |
| Neurological status | |
| Intact | 0 |
| Root injury | 1 |
| Complete cord injury | 2 |
| Incomplete cord injury | 3 |
| Continuous cord compression (neuromodifier in the setting of a neurological deficit) | + 1 |
The correct way to transport a patient with a suspected cervical fracture is in the dorsal decubitus position on a rigid surface with a person hands or pads placed beside the patient to secure the head and prevent rotation. Ideally, a collar should be fitted immediately (28). The patient should be examined while still in the dorsal decubitus position with an inspection of the ear canals to rule out the possibility of fluid fistula or otorrhagia behind the tympanic membrane, which would indicate a skull fracture. The head and spinous processes should be palpated (1-3,6).
If there are signs of spinal cord injuries or factors potentially leading to such injuries, treatment measures should be commenced immediately. Recent studies support the idea that the sooner the spine is stabilized with decompression of the injured spinal cord, the greater the chances of recovery (29). Radiographic exams should be performed that include profile, anteroposterior, oblique, and transoral views of the cervical spine. CT may be used to clarify any unclear findings in the simple radiographs, reveal an occult injury, and assess an identified fracture or fracture-dislocation in greater depth (1,30).
Orthopedic treatment to reduce the fracture or dislocation will re-conduct the vertebral canal to its normal form and dimension and lead to spinal cord decompression (31). Reduction through traction with a cranial halo is a method commonly used in some emergency services and is efficient and well tolerated by the patient. Reduction by manipulation under general anesthesia is contraindicated because it is an extremely dangerous method; even with gradual traction, care must be taken and small weights should be utilized first (32).
Because of the instability associated with dislocations, most recent guidelines indicate that surgery is required to achieve adequate reduction and stabilization, ensure spinal cord decompression, and prevent uncomfortable immobilization. Surgery may be performed via the anterior, posterior, or double routes (33). More recent anatomical and biomechanical studies support the use of instrumentation with the most modern synthesis materials, such as cages and anterior plates, or posterior lateral mass screws (34).
Posterior fixation of the cervical spine by means of implants anchored in the lateral vertebral masses has been extensively used due to its mechanical advantage over fixations that use the interspinous cerclage technique. In addition, this procedure has other technical advantages, such as the possibility to be used in cases where the posterior elements are absent or fractured.
The most recent guidelines (26) for surgical treatment are described in Table 2.
Guidelines for the surgical treatment (32) of cervical fractures.
| Situation | Findings | Approach and comments | |
|---|---|---|---|
| Central spinal cord injuries | Sagittal lordotic alignment/compression at multiple levels | Laminoplasty or laminectomy and arthrodesis | |
| Sagittal cyphotic alignment/compression at one or two levels | Previous vertebrectomy(ies) or multiple discectomies frequently requiring posterior arthrodesis with or without associated laminectomies | ||
| Vertical burst fracture (compression trauma) | Anterior cervical vertebrectomy, cage or structured graft (allogeneic or autologous) with anterior cervical plate | ||
| The isolated anterior route is usually capable of creating satisfactory decompression | |||
| It is safe only when the disco-ligamentous elements are intact | |||
| Injuries resulting from hyperextension or avulsion (distraction trauma) | Generally occur in elderly individuals | Anterior discectomy and arthrodesisVery stiff spines (ankylosing spondylitis, severe spondylitis) require surgery using the posterior approach (long lever arms) | |
| Single or bifaceted subluxation (distraction trauma) | Magnetic resonance imaging shows disc herniation | Anterior route, with discectomy, sagittal realignment, and fixation with a plate (risk of inadequate reduction and need for posterior route) | |
| Magnetic resonance imaging shows disc-ligament rupture without herniation | Posterior route, with resection of the ligamentum flavum and fixation of the lateral masses with arthrodesis (risk of progressive disc collapse and development of segmental kyphosis) 45 | ||
| The anterior route is indicated only where there is perfect facet congruence; even so, there is a risk of failure | |||
| Bifaceted dislocation requires the posterior route due to the risk of kyphosis after the use of the isolated anterior route | |||
| Isolated posterior ligamentary injury can be treated by the posterior approach with complementary decompression when necessary | |||
| There is still no absolute consensus, and the possible complications should be considered | |||
| Single or bifaceted dislocation/fracture (distraction trauma) | Associated compression fracture of the vertebral body | Plateau compressionExplosion fracture | Posterior routeAnterior and posterior routes |
| Without associated fracture of the vertebral body | Intracanal disc | Isolated anterior route if there is adequate reduction; if there is inadequate reduction, anterior and posterior routes combined | |
| Without intracanal disc | Posterior route with fixation of lateral masses and arthrodesis | ||
In addition to the commonly known complications involved in the treatment of fractures of the cervical spine with spinal cord or nerve injury (for example, pseudarthrosis, or defective consolidation, and postoperative infection), less common complications should also be considered, such as lead poisoning in cases of fractures caused by firearm injuries (35,36).
In conclusion, fractures of the cervical spine are potentially serious and can lead to devastating consequences if not properly treated. Correct diagnosis and classification of the injury is the first step toward determination of the most appropriate treatment, which can be either surgical or conservative.
Teixeira WJ, Narazaki DK and Oliveira RP performed the literature review. Marcon RM and Cristante AF wrote the manuscript. Barros Filho TEP supervised the literature review and writing and revised the final version of the manuscript.
No potential conflict of interest was reported.