Neovascular glaucoma is a challenging disease in its pathogenesis and treatment.1–3 Ischemic retinopathies can lead to neovascular glaucoma due to newly formed vessels on the iris surface and anterior chamber angle. Eyes with neovascular glaucoma can exhibit high intraocular pressure, usually treated by retinal coagulation, cyclodestructive pro” cedures, or drainage procedures.3,4 Based on experimental studies, clinical observations, and pathogenetic considera” tions, Robert Machemer proposed the intravitreal applica” tion of crystalline cortisone to locally suppress intraocular inflammation, proliferation of cells, and neovascula” rization.5–7 The purpose of the present clinical study is to report on a new potential treatment modality, the intravitreal injection of triamcinolone acetonide as adjunc” tive therapy of secondary neovascular glaucoma.
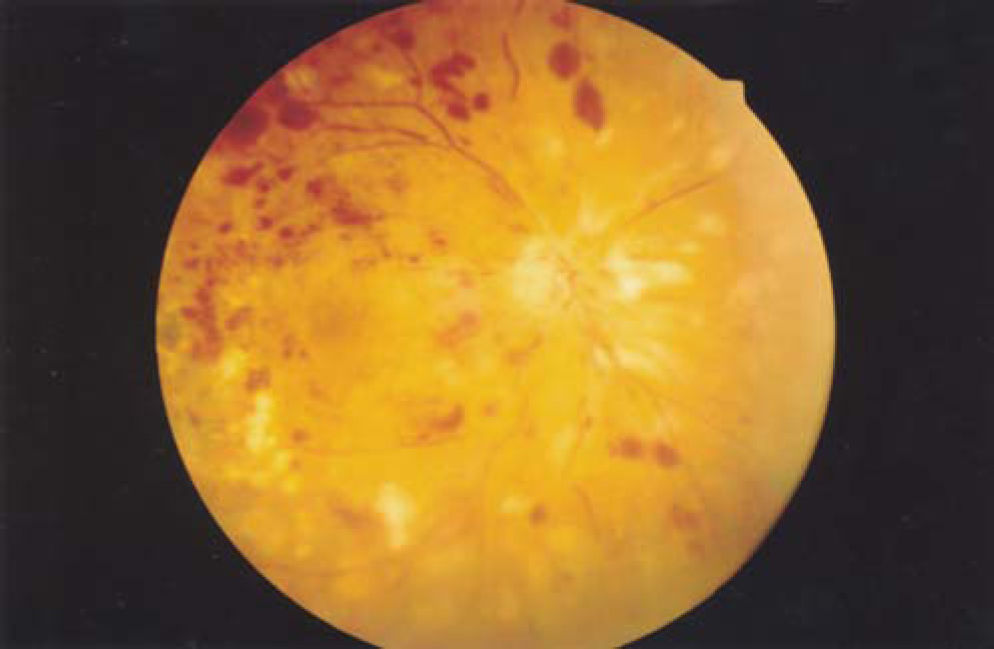
CASE REPORTA 70-year-old caucasian diabetic woman presented with poor vision in both eyes in September, 2003. Her past ocular history comprised cataract surgery and laser photocoagulation in both eyes for diabetic retinopathy and in the right eye for associated venous occlusion. The diabetes and the high blood pressure were poorly controlled, and creatinine clearance and HbA1c were 60 mL/min and 15%, respectively. Her visual acuity was counting fingers in the right eye (RE) and 20/200 in the left eye (LE). The intraocular pressure (IOP) was 13 mm Hg in the RE and 14 mm Hg in the LE. The fundus showed bilateral panretinal photocoagulation (PRP) and clinically significant macular edema but no retinal neovascularization (Fig. 1). An intravitreal triamcinolone injection was proposed initially for the right eye. An intravitreal injection of 4 mg (0.1 mL) triamcinolone acetonide (Kenalog-40, Apothecon, Princeton, NJ) was performed through the pars plana. After the procedure (October 17, 2003), her vision did not improve despite the partial drying of the macula, and the intraocular pressure ranged from 12 to18 mm Hg up to February 25, 2004. The LE was treated only with extra peripheral and macular photocoagulation. On March 10, 2004, the patient returned with a severe pain in the RE associated with nausea. Iris neovascularization, cornea edema with poorly visible fundus, and an IOP of 54 mm Hg was detected. A second intravitreal injection of 4 mg triamcinolone was given on that day, along with transconjunctival cryotherapy in the peripheral retina (5 applications per quadrant). The medical treatment comprised 0.5% timolol maleate and 1% atropine locally and oral acetazolamide. After 2 days, the patient returned with no pain, an IOP of 24 mm Hg, no corneal edema, and barely visible iris neovascularization. In the fundus, a progression of the vascular occlusion was visible, now compromising the retinal arteries (Fig. 2), and PRP was intensified. In the following visits (April 16, 2004 and May 24, 2004), the IOP was 22 mm Hg with 1% brinzolamide, 0.5% timolol maleate, and 1% atropine. The angle was free from goniosynechia in about 120°, and the vision remained the same.
Angiofluoresceinography of both eyes in September 2003. A – The right eye shows dilated veins alongside the background diabetic retinopathy. Laser marks and large areas of capillary nonperfusion are visible throughout the mid-peripheral retina. B – The left eye shows the diabetic background retinopathy and a less coarse laser pattern
Color retinography of the right eye after the cryoablation and the intravitreal injection. Two days before this picture, before the treatment, the cornea was edematous and the fundus barely visible. Vascular changes such as venous sheathing, intravascular stop of the blood column, arteriolar thinning, retinal hemorrhages, and cotton wool spots were also visible throughout the entire fundus
One of the most important still unsolved problems in clinical ophthalmology is the proliferation of vascular cells in eyes with intraocular neovascular diseases. The new vessels on the iris surface and anterior chamber angle are secondary to ischemic and, to a lesser degree, to inflammatory retinal diseases.1 Once established, this entity is difficult to manage surgically.2 The arresting of the neovascular process through retinal destructive techniques is the only known treatment.3 Even though retinal ablation has an efficacy of about 85% using cryosurgery or laser surgery; neovascular glaucoma may still appear in 1.6% of treated eyes.4 A specific pharmacological therapy for intraocular neovasularization control or regression is not still available. For many years, corticosteroids have been known to reduce intraocular inflammation and, depending on the concentration, to suppress cell proliferation. Consequently, corticosteroids, given either locally or systemically, have been used in many ocular conditions. To achieve the highest concentration of a drug at its site of action, however, it is best to give it directly into the area where this action is required. Based on experimental studies that showed steroid inhibition of appearance and growth of neovascular tissue in the eye due to inflammation5–8 and ischemia,9 along with its few described side effects.10,11Jonas et al. proposed the intravitreal injection of crystalline cortisone as an adjunctive therapy to manage neovascular glaucoma.12 They reported using a single injection of approximately 20 mg of triamcinolone acetonide with little vehicle in patients with established neovascular glaucoma. Associated procedures included goniosynechiolysis, phacoemulsification and intraocular lens implantation, and transscleral peripheral retinal cryocoagulation. After a follow-up period of 3.10 ± 2.4 months, they showed a significant decrease of the degree of rubeosis iridis, improvement in intraocular pressure, and no significant changes in visual acuity.
Recently, a smaller amount of triamcinolone (0.1 mL of 40 mg/mL) with no previous filtration has been injected into the vitreous, to control macular edema secondary to diabetes,13 central retinal vein occlusion (CRVO),14 and inflammatory disease.15 Despite the potentially vision-threatening complications such as transient or persistent intraocular high pressure,16 cataract progression,13 and aseptic17 or septic endophthalmitis,18 the gravity of the clinical condition of our patient seemed to justify this procedure. We performed a single injection of 4 mg of the commercially available triamcinolone acetonide through the pars plana along with transconjunctival cryotherapy. Our patient received 2 injections, and it may be speculated that the first injection caused a worsening of the neovascular process. Although it has frequently been a surgical approach, intravitreal corticosteroid injection has not been associated with this complication in the literature.13–20 Ip et al.,20 retrospectively studying 13 patients treated with 4 mg intravitreal triamcinolone injections to control macular edema due to central retinal vein occlusion, reported a second injection in 3 patients and 1 eye that developed iris neovascularization after the treatment. In our patients, in the 2 days after the injection, the iris neovascularization was barely visible, the corneal edema was gone, and we could complete the PRP through clear media. It has to be taken into account that the duration of the anti-angiogenic effect of the intravitreal steroids is limited about 2 weeks experimentally21,22and from 2 to 5 months clinically13,14 if not supported by additional procedures such as panretinal photocoagulation.
In the present case, it is unlikely that the rapid iris neovascularization regression, as well as the reduction in IOP, was caused solely by the retinal cryocoagulation. Though consistently stating the efficacy of this method of treatment for anterior segment neovascularization or early neovascular glaucoma, the literature is not clear about the time span in which neovascularization regression takes place.23–25 Using the panretinal cryotherapy (10 to 14 applications per quadrant), the regression of the rubeotic vessels begins after a few days of treatment, with complete resolution occurring after 4 to 6 weeks. 23,24 Using the transconjuntival anterior retina cryoablation, Sihota et al.25 report a rapid release of pain and iridocyclitis, with the corneal edema regressing over a period of 7 to 10 days. In our patient, after 48 hours of the treatment pain, iris neovascularization and corneal edema were all gone, leaving a perfect environment for further retinal photocoagulation (Fig. 2).
The results of this study support the findings of previous investigations and clinical observations.11 Using the intravitreal cortisone injection associated with the cryotherapy, we gained time and were able to stop the process of angle closure through retinal coagulation.
The outcome of this case, as well as evidence from the literature, suggests that the intravitreal application of triamcinolone acetonide helps to temporarily reduce the neovascularization of the iris. With the normalization of the intraocular pressure and clearing of the corneal edema, laser application to the retina is possible through clear media.
However, randomized prospective investigations are needed to confirm our findings and to determine the usefullness of the intravitreal injection of 4 mg of triamcinolone acetonide as an additional tool in the treatment of neovascular glaucoma secondary to ischemic retinopathies.
We thank Miss Leonor Maria Dias Sampaio for the language revision.