Asthma may cause systemic repercussions due to its severity and the effects of treatment. Our objective was to compare posture, balance, functional capacity, and quality of life (QOL) according to the severity of disease, as assessed by pulmonary function levels.
METHOD:This cross-sectional study evaluated fifty individuals with asthma. We compared two groups of adult individuals who were divided according to the median of the forced expiratory volume in one second (FEV1) as follows: group A = FEV1>74% predicted; group B = FEV1<74% predicted. All patients underwent the following tests: spirometry, whole-body plethysmography, diffusing capacity for carbon monoxide (DLco), respiratory muscle strength, posture assessment, stabilometry, six-minute walking distance (6MWD), and QOL.
RESULTS:All pulmonary function variables exhibited statistically significant differences between the two groups, except for the DLco. The maximal inspiratory pressure (MIP), maximal expiratory pressure (MEP), and 6MWD were lower in group B. The maximal mediolateral velocity and the mediolateral displacement were significantly different, while the postural changes and QOL were similar between the groups.
CONCLUSIONS:In adult individuals with asthma, the pulmonary function is associated with balance control in the mediolateral direction but does not influence the postural changes or QOL.
Asthma is a chronic inflammatory disease of the airways that involves many cells and cellular elements (1). Chronic inflammation, which is also present in patients with a recent episode of and mild forms of asthma (including the asymptomatic types), is associated with airway hyper-responsiveness. This condition causes recurrent episodes of wheezing, dyspnea, chest oppression, and coughing, particularly during the night or early in the morning (2). The World Health Organization estimates that 235 million people suffer from asthma (3).
Patients with asthma and other chronic respiratory diseases tend to develop changes in posture and balance (4,5). Asthmatic individuals exhibit an excessive recruitment of inspiratory accessory and expiratory muscles in response to the airflow obstruction that leads to maladaptive hypertrophy (5,6). Under tension, these muscles shorten and lose flexibility, causing a reduction in their length and strength (7). The biomechanics of the thoracic cage do not operate in isolation but are integrated with the body's global mechanics. Therefore, any change in the thoracic cage may cause repercussions in the overall biomechanics of the body (8-10).
Some evidence indicates that patients with several lung disorders exhibit significant deficits in postural balance, for which the physiopathological basis appears to be multifactorial (4). Weakness of the limbs, changes in balance, nutritional depletion, malnutrition, depression, cognitive deficits, and the use of medications might be considered risk factors for falls among patients with respiratory diseases, such as chronic obstructive pulmonary disease (COPD) (5,11,12). Nevertheless, there is not yet sufficient evidence to associate pulmonary function impairment with postural balance and body posture changes in patients with asthma.
Asthma may cause systemic repercussions due to its severity and the effects of treatment. Therefore, we hypothesized that factors such as posture, balance, functional capacity, and quality of life (QOL) are altered in patients with poor pulmonary function. Consequently, the aim of this study was to compare these factors between two groups of asthmatic individuals who were grouped based on their pulmonary function levels.
METHODSThe present investigation was a cross-sectional study conducted with patients recruited at the Newton Bethlem Medical Care Center in Rio de Janeiro, Brazil. Individuals diagnosed with asthma who were 18 to 50 years of age were included. Individuals who were using psychotropic medications; had a diagnosis or history of cardiovascular disease, respiratory comorbidities, or vestibular disorders; were smokers or ex-smokers; had a respiratory infection within the previous three months; or had any type of physical disability impairing locomotion were excluded from this study. Individuals older than 50 years were excluded due to the fall risk inherent to this population (4,5,11,12). The study was approved by the Research Ethics Committee of the Augusto Motta University, Rio de Janeiro (number 0012.0.307.228-11). All the participants signed an informed consent form.
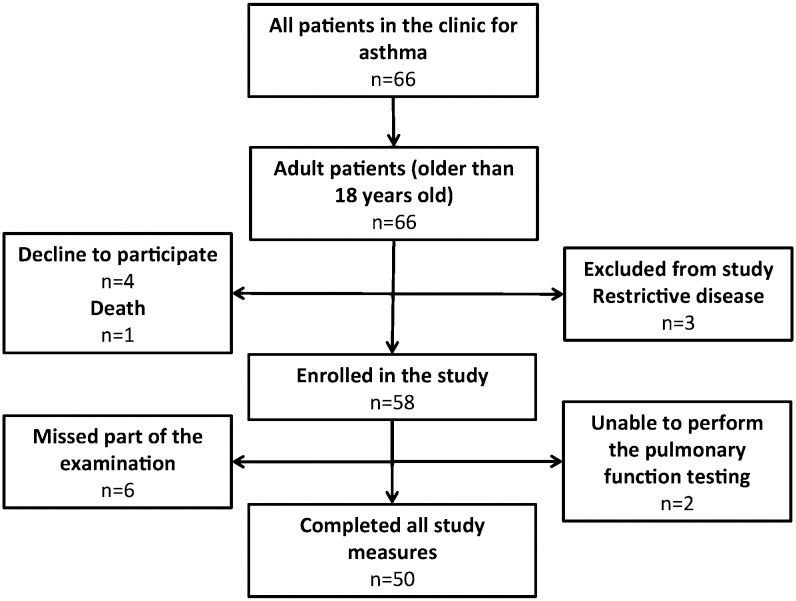
SubjectsBetween September 2011 and August 2012, 66 patients were assessed (Figure 1). From these individuals, 16 were excluded, including six who did not complete the tests, two who were unable to perform pulmonary function testing, three who exhibited an associated restrictive syndrome, four who withdrew from the study, and one who died due to acute myocardial infarction. The sample population was divided into two groups according to the median value of the forced expiratory volume in one second (FEV1) as follows: group A = FEV1 >74% predicted; group B = FEV1 <74% predicted. The FEV1 was chosen because it is the most widely used index, compared with other lung function parameters, for monitoring adults with asthma (1). Its measurement is easily obtainable, highly reproducible, and widely performed across the world (13).
Analysis of pulmonary function and functional capacitySpirometry, whole-body plethysmography, respiratory muscle strength, and the diffusing capacity for carbon monoxide (DLco) were measured using the computerized Collins Plus Pulmonary Function Testing Systems (Warren E. Collins, Inc., Braintree, MA, USA) at the Laboratory of Pulmonary Function of the State University of Rio de Janeiro. All tests followed the standards of the American Thoracic Society (14). Pereira's (15) and Neder's (16-18) equations were used to interpret the functional parameters. The six-minute walking test (6MWT) was performed at the same location along a three-meter corridor, according to the ATS recommendations. The predicted six-minute walking distance (6MWD) was estimated for all the patients, using the equations from Gibbons et al. (19).
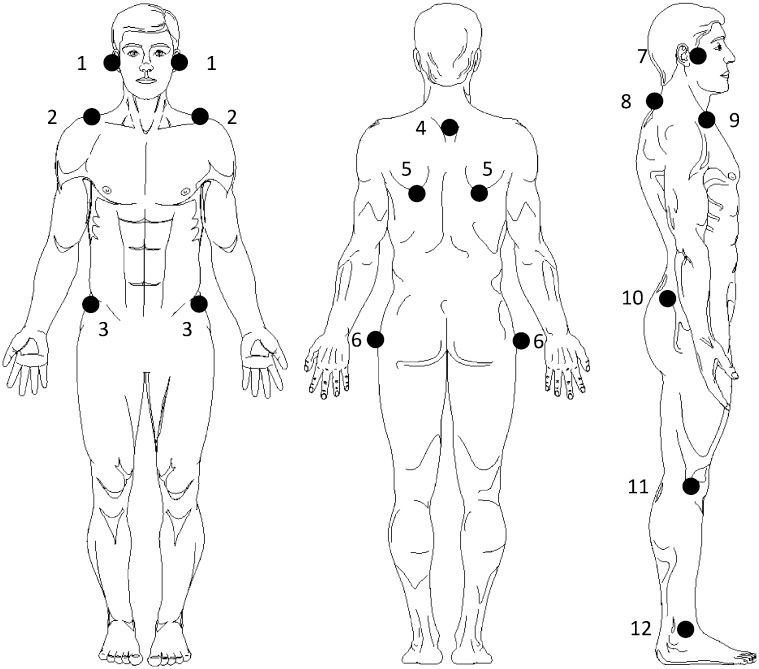
Postural assessmentThe body posture analysis was performed at the Human Movement Analysis Laboratory - Augusto Motta University, via photogrammetry using the postural assessment software (PAS, FAPESP Incubator, SP, Brazil) (20). For the acquisition of photographs, the coordinates of the anatomical points marked with passive markers (specifically, Styrofoam balls held with double-sided tape) were used. For all participants, four photographs were acquired in the anterior, posterior, and lateral (right and left) views after the anatomical points were located (Figure 2). The anatomical points were chosen based on previous studies that, using the same or a similar method, found an association between pulmonary function and posture in patients with chronic pulmonary diseases (21,22). The patients were placed in an orthostatic position on a sheet of paper on which their feet had been previously outlined, and they were instructed to adopt a comfortable position. A plumb line with two Styrofoam balls placed 1.20 meters apart was placed next to the patients and was later used to calibrate the photographs in the software. The camera was placed 163 cm above the floor and 3.0 meters from the patients. After each photograph, the sheet of paper was rotated 90°, and the patients were repositioned. The photographs were transferred to a compatible microcomputer and analyzed.
Anatomical points that were evaluated by the PAS protocol: (1) tragus (anterior view); (2) acromion (anterior view); (3) anterior-superior iliac spine (ASIS); (4) spinal processes of the third thoracic (T3) vertebrae; (5) scapula (inferior angle); (6) greater trochanter; (7) tragus (lateral view); (8) spinal processes of the seventh cervical (C7) vertebrae; (9) acromion (lateral view); (10) posterior-superior iliac spine; (11) knee (articular line); and (12) lateral malleoli.
Before analysis, the photographs were calibrated based on the two plumb line Styrofoam balls. The anatomical points marked on the patients were also marked on the photographs using the mouse, according to the software protocol. A report was generated at the end of each assessment and listed the results of the following parameters: (a) the anterior view: head - horizontal alignment, angle between the acromion and the anterior-superior iliac spine (ASIS), and ASIS - horizontal alignment; (b) the posterior view: scapula - third thoracic (T3) vertebrae horizontal asymmetry; and (c) the right and left side views: head - horizontal and vertical alignment, trunk - vertical alignment, body - vertical alignment, pelvis - horizontal alignment, knee angle, and ankle angle.
Analysis of static postural balanceThe participants performed stabilometry on a force platform (AccuSway Plus, AMTI, Watertown, MA, USA), and the data collected were analyzed using the SuiteEBG software, version 1.0 (PGSM, Paris, France). The tests were performed under an open eye, open base condition. The participants were requested to maintain the static posture while watching a target on a wall for 30 seconds at a sampling frequency of 100 Hz. The position of the feet had been previously outlined on the platform base with chalk, and the participants were requested to keep their feet turned forward and apart from each other up to the margins of the platform. The representative value for each postural balance variable was computed as the average of three trials (23). The following stabilometric variables were calculated: mediolateral standard deviation (X SD), anteroposterior standard deviation (Y SD), mediolateral amplitude (X range), anteroposterior range (Y range), elliptical area (assessed by a principal component analysis), average velocity, maximal mediolateral velocity (Vx), and maximal anteroposterior velocity (Vy) (24-26).
Analysis of the QOLThe QOL was assessed by the Asthma Questionnaire of Life Quality (AQLQ), which comprised 32 questions corresponding to the following four domains: activity limitation, symptoms, emotional function, and environmental stimuli. The score of each response varied from one (minimum score; severely impaired) to seven (maximum score; not impaired) points. The overall score was the mean of all 32 responses, and the individual domain scores were the means of the items in those domains. As the minimal score was one and the maximal score was seven, a higher overall score indicated a higher QOL. An increase of 0.5 point between assessments was considered clinically relevant (27-29).
Statistical analysisTo estimate the sample size, a pilot study was conducted using a protocol identical to that described above in a group of 20 subjects. Based on these preliminary results, the MedCalcH 8.2 software (Medicalc Software Mariakerke, Belgium) was used to calculate the sample size based on the median values of FEV1, assuming type I and type II errors of 1%. The minimal calculated value for this study required 25 individuals for each group.
The data are presented as the median and interquartile intervals (25th and 75th percentiles) or as a frequency (percentage). As the distribution of the variables was non-normal by the Shapiro-Wilk test, the Mann-Whitney test was used to perform the comparisons. A multifactorial variance analysis was performed to investigate the association between the pulmonary function, functional capacity, posture, balance, and possible confounders. This model was designed to analyze the FEV1 as the dependent variable, with covariates of age, duration of symptoms, use of oral corticosteroids (yes/no), use of inhaled corticosteroids (yes/no), maximal inspiratory pressure (MIP), maximal expiratory pressure (MEP), DLco, 6MWD, stabilometric parameters, and PAS measurements. The analysis was performed using the SigmaStat software for Windows, version 3.5 (Systat Software, Inc., Chicago, IL, USA). Statistical significance was established as p<0.05.
RESULTSThe general characteristics, pulmonary function testing, functional capacity, and QOL results for both groups are described in Table 1. Most patients were female (72%), and the median ages were 31 years for group A and 33 years for group B. All the pulmonary function variables (spirometry, whole-body plethysmography, and respiratory muscle strength) exhibited statistically significant differences between the two groups, except for the DLco (p = 0.06). The median of the 6MWD was 625 meters (566.5-687 meters) in group A, which was significantly higher than the median of group B, 577 meters (505-607.2 meters) (p = 0.05). The medians of the percentages predicted by the equations from Gibbons et al. (19) for those distances were 86.6% and 80.5% for groups A and B, respectively (p = 0.03).
General characteristics, pulmonary function, functional capacity, and QOL of the studied sample.
| Variable | Sample (n = 50) | Group A (n = 25) | Group B (n = 25) | p-value |
|---|---|---|---|---|
| Age (years) | 32.5 (24–40) | 31 (23–40.5) | 33 (26–38.5) | 0.67 |
| Gender (M/F) | 14/36 | 7/18 | 7/18 | - |
| Weight (kg) | 66.9 (40–93) | 73.5 (40–93) | 62 (44.6–91.2) | 0.06 |
| Height (m) | 1.60 (1.41–1.82) | 1.60 (1.44–1.75) | 1.60 (1.41–1.82) | 0.97 |
| BMI (kg/m2) | 25.3 (18.9–38) | 28.2 (19.3–37.7) | 23.2 (18.9–38) | 0.04 |
| Duration of symptoms (years) | 19.5 (6–27) | 18 (9–23.7) | 20 (5–31.5) | 0.70 |
| Use of OCS | 11 (22%) | 4 (16%) | 7 (28%) | 0.35 |
| Use of ICS | 34 (68%) | 13 (52%) | 21 (84%) | 0.04 |
| PEF (% predicted) | 66 (49–82) | 80 (66.5–88) | 49 (36.7–66) | <0.001 |
| FEV1 (% predicted) | 74 (53–87) | 87 (81.7–94.2) | 53 (42.7–68.2) | <0.001 |
| FVC (% predicted) | 94 (79–104) | 104 (97–108.2) | 79 (68–88.7) | <0.001 |
| FEV1/FVC (%) | 70 (56–75) | 73 (70–80.5) | 56 (49–67) | <0.001 |
| MIP (% predicted) | 55.7 (35.6–71.4) | 61.5 (50.5–78.7) | 44.7 (29.8–64.2) | 0.02 |
| MEP (% predicted) | 60.1 (46.3–81.7) | 76.8 (50.8–80.1) | 52.1 (40–77.8) | 0.03 |
| TLC (% predicted) | 103.5 (102–123) | 105 (99.7–115.7) | 121 (105.2–129) | 0.02 |
| RV (% predicted) | 134.5 (110–214) | 115 (104.7–132.2) | 190 (145.5–237.2) | <0.001 |
| Raw (% predicted) | 1.40 (1–2.20) | 1.10 (0.80–1.70) | 1.70 (1–3.90) | 0.01 |
| SGaw (% predicted) | 0.20 (0.10–0.30) | 0.27 (0.21–0.33) | 0.14 (0.10–0.20) | <0.001 |
| DLco (% predicted) | 103 (89–116) | 107 (99–117.2) | 98 (86.7–112) | 0.06 |
| 6MWD (% predicted) | 83.6 (76–92) | 86.6 (79.8–93.2) | 80.5 (72.1–86.8) | 0.03 |
| AQLQ(s) mean | 3.10 (2.50–4.40) | 3.10 (2.40–3.70) | 3.40 (2.60–4.60) | 0.37 |
The results are expressed as the medians (interquartile range) or numbers (%). The p-value between groups A and B was calculated. BMI: body mass index; OCS: oral corticosteroids; ICS: inhaled corticosteroids; PEF: peak expiratory flow; FEV1: forced expiratory volume in one second; FVC: forced vital capacity; MIP: maximal inspiratory pressure; MEP: maximal expiratory pressure; TLC: total lung capacity; RV: residual volume; Raw: airway resistance; SGaw: specific airway conductance; DLco: diffusing capacity for carbon monoxide; 6MWD: six-minute walking distance; AQLQ(s): asthma QOL questionnaire.
The stabilometric data are described in Table 2. The variables related to the amplitude of the mediolateral sway (X SD, X range) and the velocity of displacement of the center of pressure (CoP) along the mediolateral axis (Vx) exhibited statistical significance between the groups (p<0.001, p = 0.04, and p<0.001, respectively). Table 3 describes the postural analysis values of the entire sample and those for groups A and B individually. No variable exhibited a significant difference between the groups (p>0.05 for all variables).
Stabilometric values of the studied sample performed under an open eye, open base condition.
| Variable | Sample (n = 50) | Group A (n = 25) | Group B (n = 25) | p-value |
|---|---|---|---|---|
| X SD (cm) | 0.17 (0.11–0.28) | 0.12 (0.09–0.21) | 0.24 (0.15–0.35) | <0.001 |
| Y SD (cm) | 0.37 (0.23–0.52) | 0.36 (0.20–0.47) | 0.39 (0.26–0.52) | 0.31 |
| X range (cm) | 0.82 (0.52–1.23) | 0.65 (0.46–1.03) | 0.97 (0.70–1.41) | 0.04 |
| Y range (cm) | 1.75 (1.14–2.41) | 1.76 (1.03–2.36) | 1.75 (1.17–2.42) | 0.52 |
| Elliptical area (cm2) | 0.48 (0.25–1.12) | 0.46 (0.16–1.07) | 0.57 (0.30–1.16) | 0.23 |
| V avg (cm/s) | 0.46 (0.36–0.59) | 0.44 (0.33–0.54) | 0.50 (0.38–0.60) | 0.23 |
| Vx (cm/s) | 1.34 (0.93–2.85) | 1.02 (0.80–2.09) | 1.90 (1.09–3.15) | <0.001 |
| Vy (cm/s) | 2.40 (1.47–3.81) | 2.23 (1.80–3.63) | 2.50 (1.40–4.35) | 0.45 |
The results are expressed as medians (interquartile range) or numbers (%). The p-value between groups A and B was calculated. X SD: mediolateral standard derivation; Y SD: anteroposterior standard derivation; X range: mediolateral range; Y range: anteroposterior range; V avg: average velocity; Vx: maximal mediolateral velocity; Vy: maximal anteroposterior velocity.
PAS values of the studied sample.
| Variable | Sample (n = 50) | Group A (n = 25) | Group B (n = 25) | p-value |
|---|---|---|---|---|
| HHA (AV) | 1.45 (-2.00–3.80) | 0 (-2.30–3.25) | 2.5 (-1.67–6.2) | 0.16 |
| AcASISA | 0.20 (-2.77–2.57) | 1.20 (-1.75–3.40) | -0.40 (-3.72–1.50) | 0.06 |
| ASISHA | 0 (-1.40–2.07) | 1.30 (-1.60–2.60) | 0 (-1.07–1.02) | 0.18 |
| ST3Has | 0 (-16–19.4) | 0 (-13–17.4) | 0 (-22.6–26.9) | 0.94 |
| HHA (RV) | 42.1 (36.3–46.2) | 40.1 (35.6–45) | 43.5 (38.7–50) | 0.14 |
| HHA (LV) | 40.8 (36.9–47.2) | 42 (38.5–50.7) | 38.9 (35.8–45) | 0.07 |
| HVA (RV) | 18.8 (12.3–29.9) | 17.1 (12.4–26.8) | 25.2 (9.20–30.4) | 0.58 |
| HVA (LV) | 0 (-2.30–3.25) | 20.6 (11.5–29.3) | 24.9 (14.5–34.3) | 0.41 |
| BVA (RV) | 1.60 (0.10–2.60) | 1.70 (0.35–2.50) | 1 (-0.75–2.62) | 0.70 |
| BVA (LV) | 0.50 (-0.30–1.80) | 0.70 (-0.05–1.82) | 0.20 (-0.82–1.80) | 0.47 |
| TVA (RV) | -4.20 (-6.70–-2.40) | -3.50 (-5.90–-1.57) | -4.30 (-8.60–-3.70) | 0.10 |
| TVA (LV) | -3.25 (-7.50–-1.10) | -3.20 (-4.65–-0.57) | -3.50 (-7.67–-1.52) | 0.43 |
| PHA (RV) | -14.0 (-19.7–-9.30) | -13.4 (-19.2–-9.15) | -16.7 (-20.4–-9.7) | 0.45 |
| PHA (LV) | -14.5 (-19.9–-10.5) | -12.2 (-18.8–-8.25) | -15.2 (-23.8–-11.2) | 0.18 |
| RKA | 0.95 (-5.10–5.50) | -0.60 (-5.03–6.45) | 1.2 (-5.37–5.42) | 0.85 |
| LKA | -0.80 (-6.80–4.00) | -0.40 (-6.17–2.27) | -2.40 (-8.82–4.32) | 0.50 |
| RAA | 84.35 (81.50–87.00) | 84.7 (81.1–87.7) | 83.9 (82.2–86.5) | 0.70 |
| LAA | 87.4 (82.8–90.0) | 87.3 (82.1–88.2) | 87.5 (81.8–90.0) | 0.97 |
The results are expressed as the medians (interquartile range) referred to angulations, except ST3HAs (cm). The p-value between groups A and B was calculated. HHA (AV): head - horizontal alignment (anterior view); AcASISA: angle between the acromion and the anterior-superior iliac spine alignment; ASISHA: anterior-superior iliac spine horizontal alignment; ST3Has: scapula - third thoracic vertebrae horizontal asymmetry; HHA (RV): head - horizontal alignment (right view); HHA (LV): head - horizontal alignment (left view); HVA (RV): head - vertical alignment (right view); HVA (LV): head - vertical alignment (right view); BVA (RV): body - vertical alignment (right view); BVA (LV): body - vertical alignment (left view); TVA (RV): trunk - vertical alignment (right view); TVA (LV): trunk - vertical alignment (left view); PHA (RV): pelvis - horizontal alignment (right view); PHA (LV): pelvis - horizontal alignment (left view); RKA: right knee angle; LKA: left knee angle; RAA: right ankle angle; LAA: left ankle angle.
All variables were assessed in a multifactorial variance model (Table 4). The covariates X SD, Vx, and MIP were significantly associated with the FEV1.
Multifactorial variance analysis of the relationship between the pulmonary function, functional capacity, posture, balance, and clinical data of the studied subjects. Only statistically significant associations are presented.
| Outcome variable | Independent variables | Unstandardized coefficient | p-value | ||
|---|---|---|---|---|---|
| B | SE | Wald F-test | |||
| FEV1 | Mediolateral standard derivation | 4.32 | 1.73 | 8.89 | 0.001 |
| Maximal mediolateral velocity | 3.07 | 1.57 | 5.63 | 0.027 | |
| Maximal inspiratory pressure | 2.81 | 1.44 | 4.95 | 0.032 | |
B: regression coefficient. SE: standard error. FEV1: forced expiratory volume in one second.
The main findings of the present study were as follows: (a) there were significant differences in the variables related to balance and functional capacity between the two groups of asthmatic individuals who were divided according to the FEV1, and (b) the posture and QOL parameters did not exhibit a significant difference between the groups. Until the present, no study appears to have focused on these topics in an integrated manner.
Most of the participants were women, which is in agreement with the literature reports of a higher prevalence of asthma among adult females (30,31). The median FEV1 value [74% (53-87%)] indicates that the present study assessed a homogeneous sample population corresponding to the moderate persistent stage based on the older Global Initiative for Asthma (GINA) classification (1). Because the FEV1 was used to divide the groups, a difference was observed for all pulmonary function parameters, except for the DLco (p = 0.06). Notably, the mechanisms underlying the FEV1 and DLco are different, as the former assesses lung mechanics, and the latter assesses the transfer of gases from the alveoli to the red blood cells (32,33).
The patients in group B presented with lower respiratory muscle strength. This result is in agreement with the premise that the inspiratory muscles of chronic asthmatic patients are shortened due to hyperinflation, reducing their efficacy (34,35). A Brazilian study assessed the effects of muscle stretching on the MIP and MEP values and found an improvement in respiratory muscle strength following sessions of global posture re-education among healthy individuals (36). As there is no evidence indicating whether the same results might be achieved in asthmatic patients with different degrees of airflow obstruction, this topic is an area for future research.
Several QOL questionnaires have revealed that the results might help to establish the severity of asthma and that modification of the results might correlate with the clinical status of patients (37,38). A study has demonstrated that, in adults with asthma, the QOL is closely related to the frequency of symptoms and the level of pulmonary function (38). In our investigation, the two groups did not exhibit a significant difference in the median values of the AQLQ. The socioeconomic conditions of the investigated sample might have influenced this result. Several patients reported an inability to discontinue their activities (particularly paid work) despite exhibiting symptoms and thus did not rate their activity as limited by the disease.
The assessment of patients' functional capacity is important for evaluating the response to interventions and for prescribing physical training protocols (39). In our study, the 6MWT proved to be a reliable method of assessing the functional capacity of asthmatic individuals. The test was easily understood, tolerated, and accepted by the participants. Group A exhibited a greater predicted 6MWD than group B did (86.6% vs. 80.5%, respectively; p<0.05), which denotes a greater functional capacity defined by the patients' ability to perform everyday activities. In a study conducted with adult women who were classified with mild to moderate asthma (FEV1 = 72.9±19.3%), the average 6MWD was lower than in group B of our study (524 meters vs. 575 meters, respectively) and was even lower when compared to group A (524 meters vs. 625 meters, respectively) (40). The same result was obtained in a comparison of another study of sedentary individuals and in groups A and B of our investigation (544 meters vs. 575 meters and 544 meters vs. 625 meters, respectively) (41); however, the sample from the former study consisted of young adults (20-30 years of age) and used a different reference equation than the one used in our investigation.
The alignment of the static posture is considered adequate when the overload on the joints, ligaments, and bones that are required to support the body weight is minimal (8,11). Photogrammetry has been increasingly used in several Brazilian studies, and the PAS is one of the most widely used postural analysis systems because it exhibits satisfactory intra- and inter-examiner reliabilities (24,42). In the present study, we did not find significant differences between the groups with respect to body posture variables. We did not find any literature reports of the normal values of these variables for comparison. Robles-Ribeiro et al. (43) reported that adult patients with mild to severe asthma exhibited several postural changes, including protracted shoulders. However, the quantitative measures related to this change, specifically scapula and T3 asymmetry, do not allow for confirming that observation. Danis et al. (44) found a weak correlation between posture and stability (r<0.30; p≤0.05) in patients with vestibular dysfunction and in healthy individuals. The authors suggested that major postural changes may correlate with stability, which was not observed for either group in our study.
The understanding of posture includes the idea of postural control. The alignment of the body segments and postural alterations might affect the location of the gravity center, thus affecting the control of body stability (44). Neither group in our study exhibited postural changes (p>0.05), which might be explained by the ability of the human body to adapt to various conditions.
Stability is achieved through the generation of moments of force on the body joints to neutralize the effect of gravity and any other perturbation. This continuous and dynamic process maintains a given posture over time. Therefore, the integration of somatosensory and vestibular input is necessary to ensure adequate postural control (24). While the anteroposterior balance is maintained by the ankle torque, the mediolateral balance is maintained by the hip and trunk torque. As observed in patients with COPD, in the present study, the degree of hyperinflation in the group with more severe asthma might also contribute to the increased activity of the trunk muscles, with a consequent increase in their rigidity. These phenomena might reduce the contribution of the trunk movements and the force moments for balance control (4,5). Interestingly, Cunha et al. (23) also demonstrated a higher area of CoP displacement in adults with asthma using a force platform.
We also investigated whether the clinical data, functional capacity, posture, and balance could independently predict the pulmonary function. In this investigation, the X SD, Vx, and MIP were covariates for the FEV1. Mientjes and Frank (45) demonstrated that the modified control of trunk muscles and the reduction in trunk movement were associated with increased COP displacement, particularly in the mediolateral direction. Thus, it is reasonable to imagine that these changes may be more marked in adults with severe asthma. The relationship between the FEV1 and the MIP is also noteworthy. In adults with asthma, hyperinflation leads to flattening of the diaphragm, causing a mechanical disadvantage and impaired function of the inspiratory muscles (46).
The lack of a control group, the cross-sectional design, and the small sample size are the main limitations of the present study. Due to the lack of a control group, we cannot definitively conclude that the changes found are exclusively or mainly caused by the disease severity. In addition, the present study is a cross-sectional analysis, which makes the establishment of cause-effect relationships difficult. Thus, longitudinal studies may better clarify these findings. Furthermore, additional investigations using the ‘classification of asthma by level of control’ (1) may provide new insights regarding balance and its relationship to the QOL.
We conclude that, in adult individuals with asthma, pulmonary function is associated with balance control in the mediolateral direction but does not influence the postural changes or QOL in these patients.
Almeida VP and Lopes AJ contributed to the study conception and design, the revision of the article, and the approval of the manuscript's final version. Guimarães FS contributed to the study conception and design and to the approval of the manuscript's final version. Moço VJR contributed to the analysis and interpretation of the data and to the approval of the manuscript's final version. Ferreira AS conducted the statistical analysis and approved the manuscript's final version. Menezes SLS contributed to revising the article and to the approval of the manuscript's final version.
No potential conflict of interest was reported.