The present study was designed to analyze the serum levels of aspartate and alanine aminotransferases, gamma-glutamyl transferase, and the hematocrit in patients with chronic kidney disease who were undergoing peritoneal dialysis or hemodialysis.
PATIENTS AND METHODS:Twenty patients on peritoneal dialysis and 40 on hemodialysis were assessed, and the patients were matched according to the length of time that they had been on dialysis. Blood samples were collected (both before and after the session for those on hemodialysis) to measure the enzymes and the hematocrit.
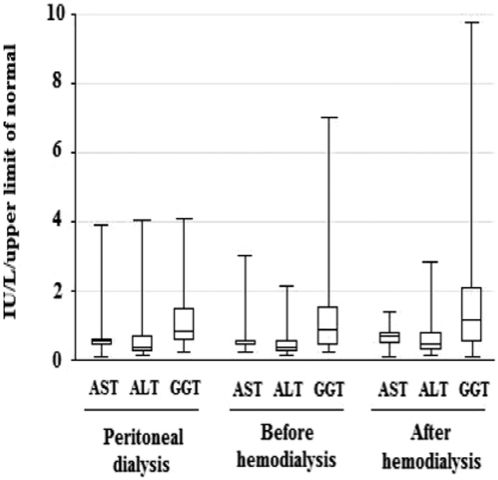
RESULTS:In the samples from the patients who were undergoing peritoneal dialysis, the aspartate and alanine aminotransferase levels were slightly higher compared with the samples collected from the patients before the hemodialysis session and slightly lower compared with the samples collected after the hemodialysis session. The levels of gamma-glutamyl transferase in the hemodialysis patients were slightly higher than the levels in the patients who were undergoing peritoneal dialysis. In addition, the levels of aminotransferases and gamma-glutamyl transferase that were collected before the hemodialysis session were significantly lower than the values collected after the session. The hematocrit levels were significantly lower in the patients who were on peritoneal dialysis compared with the patients on hemodialysis (both before and after the hemodialysis session), and the levels were also significantly lower before hemodialysis compared with after hemodialysis.
CONCLUSION:The aminotransferase levels in the patients who were undergoing peritoneal dialysis were slightly higher compared with the samples collected before the hemodialysis session, whereas the aminotransferase levels were slightly lower compared with the samples collected after the session. The hematocrits and the aminotransferase and gamma-glutamyl transferase levels of the samples collected after the hemodialysis session were significantly higher than the samples collected before the session. Taken together, the present data suggest that hemodilution could alter the serum levels of liver enzymes.
Patients with chronic kidney disease (CKD) who are undergoing hemodialysis (HD) and are infected with hepatitis C virus (HCV) have been shown to present with lower serum levels of alanine aminotransferase (ALT) than HCV-infected patients with normal renal function (1,2). Generally, ALT levels are below the upper limit of the normal (ULN) range but higher than the levels found in noninfected HD patients (3–5).
Even in noninfected HCV patients, ALT serum levels are lower in patients with CKD undergoing HD compared with the population that has normal renal function (6,7). ALT levels may be lower because of a deficiency in vitamin B6, which is a coenzyme of ALT, or hemodilution, which occurs because of water retention in patients with CKD before an HD session (8–10).
In regard to patients who do not have CKD, there has been a proposal to reduce the ULN of ALT to approximately 70% of the “conventional limits” when screening for liver abnormalities. Clinicians have argued that the current limits, which were originally defined approximately 25 years ago, may consider some individuals to be “healthy” when they actually have steatosis or an HCV infection. When the ULN was reduced, there was an increase in the sensitivity of ALT from 55% to 76% for the diagnosis of “discrete” liver diseases; however, the specificity was reduced from 97% to 89% (11). A study of a large Korean population revealed that the risk of mortality from liver disease would be higher in individuals with normal levels of ALT that were close to the ULN compared with individuals with lower ALT levels. A proposal was put forward to reduce the ULN level to approximately 75% of the current ULN level of ALT (12).
In an attempt to clarify whether lower levels of aminotransferases in patients with CKD are a result of renal failure or the type of dialysis treatment, the present preliminary study analyzed the ALT serum levels in patients who were undergoing peritoneal dialysis (PD) and HD. We also measured the levels of aspartate aminotransferase (AST) and gamma-glutamyl transferase (GGT). In addition, the hematocrit (Ht) was assessed to investigate the possibility of hemodilution.
PATIENTS AND METHODSThe present study, which was conducted as a case series with an internal comparison group, involved 60 patients with CKD who were in renal replacement therapy and attended a dialysis unit in the city of Recife, Brazil. Twenty of the 26 patients who were undergoing PD were included; six were excluded because they either refused to take part in the study or switched their type of dialysis. Concurrently, 40 out of the 211 patients who were undergoing HD in the Nefroclinica Dialysis Unit were randomly selected for the present study, and the HD patients were paired in a 1∶2 ratio according to the period of time that they had been on renal replacement therapy.
To be included in the present study, patients had to be at least 18 years old, have CKD, and have been undergoing dialysis therapy by HD or PD for a minimum of six months. The patients were excluded if they had previously been diagnosed with hepatitis B and/or if they consumed ≥40 g/day of alcohol.
After explaining the aims of the study to the patients, interviews were conducted by a researcher (IROL), and blood samples were collected and sent to the Central Laboratory at the Hospital das Clínicas – Universidade Federal de Pernambuco.
ALT, AST, and GGT serum levels were determined by an automated kinetic method for blood samples, which were taken from each patient immediately before and after a single HD session. In addition, samples were obtained from the patients who were undergoing PD after they completed the questionnaire.
The serum concentration for each patient was divided by the ULN (according to gender) of ALT (31 IU/L for women and 41 IU/L for men), AST (31 IU/L for women and 35 IU/L for men), and GGT (38 IU/L for women and 55 IU/L for men). The Ht was measured using a CELL-DYN 4000 analyzer. Antibodies (anti-HCV) against the HCV and surface antigen (HBsAg) of hepatitis B virus (HBV) were determined by enzyme immunoassays (Abbott®).
We compared the Ht and the median serum levels of AST, ALT, and GGT in the patients on PD with the values from the patients on HD before and after the dialysis session. In addition, we compared the Ht and the median serum levels of the enzymes in the 40 patients who were undergoing HD before and after the dialysis session. Excel software was used, and the Mann-Whitney U test was applied to compare the median (P25; P75) values. The chi-squared test or Fisher's exact test was used to compare frequencies, and statistical significance was set as p<0.05.
The study was approved by the Ethics Committee of the Health Sciences Center at the Universidade Federal de Pernambuco and followed the guidelines established by the Declaration of Helsinki.
RESULTSTable 1 provides a description of the demographic characteristics, the occurrence of anti-HCV and the etiology of CKD in the 60 patients who were included in the present study (the patients were divided into two groups according to the type of dialysis). Among the 20 PD patients, 12 (60%) had received HD before beginning the PD treatment. In these 20 PD patients, the AST and ALT serum levels were each higher than the ULN in three patients (15% for each enzyme). In addition, the GGT levels in eight patients (40%) were higher than the ULN.
Demographic characteristics and etiologies of chronic renal failure for the 60 patients who were undergoing dialysis (20 on PD and 40 on HD).
| Peritoneal dialysis | Hemodialysis | p-value | |
|---|---|---|---|
| N | 20 | 40 | |
| Age±SD (years)Range (years) | 48±17(24 - 78) | 54±15(21 - 86) | 0.168 |
| Female (%) | 11 (55%) | 20 (50%) | 0.927 |
| Anti-HCV+ | 3 (15%) | 3 (7.5%) | |
| Etiology of chronic renal failure | |||
| Systemic arterial hypertension | 3 (15%) | 12 (30%) | 0.343 |
| Diabetes mellitus | 3 (15%) | 4 (10%) | 0.676 |
| SAH + DM | 0 (0%) | 2 (5%) | 0.548 |
| Systemic lupus erythematosus | 3 (15%) | 2 (5%) | 0.322 |
| Others | 1 (5%) | 10 (25%) | 0.081 |
| Undetermined | 10 (50%) | 10 (25%) | 0.100 |
anti-HCV – hepatitis C virus antibody; SAH – systemic arterial hypertension;
DM – diabetes mellitus.
Among the 40 HD patients, the AST serum level was higher than the ULN in two (5%) patients before the dialysis session and three patients (7.5%) after the dialysis session, and similar findings were observed for the levels of ALT (i.e., the ALT serum level was higher in three (7.5%) patients before dialysis and five (12.5%) patients postdialysis). The GGT serum level was higher than the ULN in 17 (42.5%) patients before dialysis and 21 (52.5%) patients postdialysis.
Table 2 provides a description of the median Ht in the 60 patients with CKD and the median values and ranges of the AST, ALT, and GGT serum levels divided by the ULN. It should be emphasized that the median values of the serum levels of the aminotransferases were below the ULN in the patients who were undergoing PD and HD (both before and after the session). The median values of GGT were near the ULN in patients on PD and in samples collected before the HD session; however, they were higher than the ULN in the samples collected after the HD session (Figure 1).
The median (P25; P75) Ht and the median serum levels of AST, ALT, and GGT divided by the ULN for the 20 patients on PD compared with the 40 patients on HD (before and after the HD session).
| Liverenzymes | PeritonealdialysisMedian (P25; P75) | BeforehemodialysisMedian (P25; P75) | p-value | AfterhemodialysisMedian (P25; P75) | p-value |
|---|---|---|---|---|---|
| AST/ULN(range IU/L) | 0.53 (0.41; 0.61)(4 – 121) | 0.47 (0.41; 0.55) a(8 – 93) | 0.54 | 0.68 (0.46; 0.77) a(3 – 48) | 0.13 |
| ALT/ULN(range IU/L) | 0.39 (0.22; 0.71)(6 – 125) | 0.37 (0.21; 0.56) b(6 – 66) | 0.87 | 0.44 (0.27; 0.77) b(6 – 87) | 0.42 |
| GGT/ULN(range IU/L) | 0.83 (0.55; 1.48)(13 – 155) | 0.88 (0.43; 1.55) c(9 – 318) | 0.74 | 1.14 (0.51; 2.10) c(4 – 372) | 0.68 |
| Ht (%) | 32.9 (29.8; 35.5) | 36.7 (32.1; 41.3) d | 0.03 | 41.3 (33.1; 47.1) d | 0.001 |
a) p<0.001 b) p<0.001 c) p<0.001 d) p<0.001.
AST – aspartate aminotransferase; ALT – alanine aminotransferase;
GGT – gamma-glutamyl transferase; Ht – hematocrit;
ULN – upper limit of normal.
In the patients who were undergoing PD, the median AST (0.53 IU/L) and ALT (0.39 IU/L) serum levels were slightly higher compared with the samples collected from the HD patients before their HD session (0.47 and 0.37 IU/L, respectively) and slightly lower than samples collected after the session (0.68 and 0.44 IU/L, respectively). The GGT serum levels were slightly lower in the patients who were undergoing PD compared with the samples collected from the patients who were undergoing HD (both before and after the session).
We also analyzed the median Ht and the median AST, ALT, and GGT serum levels divided by the ULN before and after dialysis for the 40 patients with CKD who were undergoing HD. The AST, ALT, and GGT serum levels that were collected before the dialysis session were significantly lower than the values that were observed after dialysis (Table 2).
The Ht rates were significantly lower in the patients on PD compared with the patients on HD (both before and after the session), and the Ht rates were also significantly lower before dialysis compared with after the HD session (Table 2).
DISCUSSIONStudies have revealed that ALT serum levels are lower in patients with CKD compared with patients with normal renal function, which raises the question of whether the lower levels are related to CKD factors or to the HD treatment (1,2,10,13–15).
Researchers have assumed that there is a correlation between the ALT serum levels and the severity of renal failure caused by glomerular lesions. Indeed, Fabrizi et al. (8) reported lower ALT levels in patients who were undergoing HD compared with patients with CKD who were undergoing conservative treatment (predialysis), which demonstrated that the ALT serum levels were reduced concomitantly with the progression of renal dysfunction.
Nevertheless, given the possibility that hypoaminotransferasemia could be related to hemodilution, the present preliminary study assessed patients who were undergoing HD and patients who were undergoing PD. We observed that the ALT serum levels were slightly higher in the 20 patients with CKD who were undergoing PD compared with the 40 patients who were undergoing HD when the samples were collected before the dialysis session. A comparison of the mean ALT serum levels for the patients on PD and the postdialysis measurements for the HD patients showed that the ALT levels after therapy were slightly higher. These findings suggest that hemodilution could be involved in reducing ALT levels. Interestingly, the patients on HD presented with fluid retention before the dialysis session; however, the fluid retention regressed after the session ended. If the present study included a larger number of patients, the differences in the median values of aminotransferases may have been even greater.
Indeed, a recent study has confirmed that the Ht and the ALT level are lower before HD and higher after dialysis, which is inversely proportional to the loss of water weight (10). The patients on PD, however, did not present with fluid accumulation or rapid fluid loss, which normally occurs after HD sessions. In addition, the patients on PD evolved with stable and higher serum levels of aminotransferases.
The possibility of hemodilution is corroborated when the mean values of AST and ALT in the same 40 patients are compared in the samples collected before and after the HD session. There was a significant increase in both the AST and the ALT serum levels after the dialysis session. Moreover, a significant increase in the Ht after the HD session was also observed, which provided support for the hypothesis that patients with CKD retain water before HD.
Few authors have discussed AST and GGT levels in patients with CKD who were undergoing dialysis treatment (4). The data from the present study illustrated that AST and GGT levels behave in a similar manner as ALT, which excludes the possibility of an alteration in aminotransferase production, such as a reduction of synthesis because of vitamin B6 deficiency (9).
Importantly, the GGT levels exceeded the ULN in the two groups of patients with a greater frequency than the aminotransferases. Furthermore, the median values of the GGT serum levels were near the ULN and were higher than those for AST and ALT in the three measurements. Similarly, Souza et al. evaluated 87 patients with CKD and observed that the GGT serum levels were higher than the aminotransferase levels (16).
The high GGT levels in patients who were undergoing dialysis may have been induced by the use of medication or been related to the origins of CKD, such as diabetes mellitus, which can cause steatohepatitis (17). In addition, high GGT serum levels could be related to malnutrition-inflammation-atherosclerosis (MIA syndrome), which has been observed in patients with CKD who were undergoing dialysis because of systemic arterial hypertension or diabetes mellitus (18).
There are only a few articles, however, that describe the GGT levels in patients with CKD (16,19,20), and further studies are needed to assess the possibility of other mechanisms that may be involved in the changes of this liver enzyme.
Unlike the aminotransferases, the Ht was lower in the patients on PD compared with the patients on HD (both before and after the HD session). This finding could be related to the improved control of anemia in patients on HD and to the more appropriate replacement of iron supplementation and erythropoietin because the patients on HD have more frequent contact with the dialysis unit than the patients on PD.
In conclusion, the aminotransferase serum levels were slightly higher in the patients with CKD who were undergoing PD compared with the patients on HD when the samples were collected before the HD session. In addition, the median values of the samples collected after the HD session were significantly higher than the values collected before dialysis. Because this was the first study to analyze these three enzymes in patients on HD and patients on PD, further research is needed to confirm whether hemodilution is the cause of these differences or whether other factors are involved in the alteration of the AST, ALT and GGT serum levels.
AUTHOR CONTRIBUTIONSLiberato IRO was responsible for the project design, material collection, data analysis, and manuscript writing. Lopes EPA was responsible for supervising the project and correcting the manuscript. Cavalcante MAGM was responsible for the patients and participated in meetings to discuss the strategies for data collection and study methodology. Pinto TC helped with the questionnaires and the data collection. Moura IF was responsible for the biochemical assays and analyses of all the results. Loureiro Jr L was responsible for the dose strategies and provided suggestions regarding the manuscript.
No potential conflict of interest was reported.