The metabolic test using 18F-fluorodeoxyglucose is a useful tool for the management of patients with Hodgkin lymphoma, either for staging purposes or for the evaluation of suspicious masses that can frequently occur after treatment. The aim of the present study was to investigate the value of the 18F-fluorodeoxyglucose test performed with a dual-head coincident gamma camera (CGC-PET with fluorodeoxyglucose) for the staging and the detection of residual tumor of patients with Hodgkin lymphoma.
METHODS:Thirty-eight consecutive patients were included in this retrospective study; the metabolic test comprising CGC-PET with FDG was done in 18 patients for staging work-up (Group 1), and the results were compared to conventional clinical staging procedures that included computed tomography scans and bone marrow biopsy. The remaining 20 patients were evaluated with CGC-PET with fluorodeoxyglucose due to the presence of residual masses or a new lesion (Group 2).
RESULTS:The 18F-Fluorodeoxyglucose metabolic test, CGC-PET with fluorodeoxyglucose, upstaged 5 (27%) of the Group 1 patients and detected more lesions (45) than conventional methods of staging (33). Of the 20 patients in Group 2, 11 had positive18F-fluorodeoxyglucosetests, and a viable tumor was confirmed in 9 patients. Regarding the 9 patients with negative fluorodeoxyglucose metabolic tests, the 1-year probability of recurrence was 11.8%. The sensitivity, specificity, positive predictive value, negative predictive value, and accuracy of the CGC-PET with fluorodeoxyglucose test were 90%, 80%, 82%, 89%, and 85% respectively.
CONCLUSIONS:The metabolic test comprising CGC-PET with fluorodeoxyglucose had a higher diagnostic accuracy than conventional methods in the staging of Hodgkin lymphoma and thus is a valuable noninvasive tool for the diagnosis of suspicious lesions.
O estudo metabólico com 18F-fluorodeoxi-glicose é uma ferramenta útil para o manejo de portadores de linfoma de Hodgkin, tanto como método auxiliar no estadiamento da doença, quanto na avaliação de massas suspeitas encontradas após tratamento. O objetivo deste estudo foi investigar o valor do estudo com 18F-fluorodeoxiglicose em gama câmara híbrida no estadiamento e na detecção de tumor residual em pacientes com linfoma de Hodgkin.
MÉTODOS:Trinta e oito pacientes foram incluídos neste estudo retrospectivo, 18 foram avaliados com o estudo metabólico durante o estadiamento (Grupo 1), sendo os resultados do estudo comparados com os obtidos com o estadiamento convencional, que incluiu tomografia e biópsia de medula óssea. Os 20 pacientes restantes realizaram o estudo metabólico devido à presença de massa residual ou de nova lesão suspeita (Grupo 2).
RESULTADOS:O estudo metabólico aumentou o estádio de cinco (27%) dos pacientes do Grupo 1 e pôde detectar mais lesões que os métodos convencionais de estadiamento (45 lesões detectadas com 18F-fluorodeoxiglicose versus 33 lesões métodos convencionais). Nos 20 pacientes do Grupo 2, 11 foram 18F-fluorodeoxiglicose positivos e tumor viável foi confirmado em 9 pacientes. Nos 9 pacientes com estudo metabólico negativo, a probabilidade de recidiva em um ano foi de 11.8%. A sensibilidade, especificidade, valor preditivo positivo, valor preditivo negativo e a acurácia do estudo metabólico foram de 90%, 80%, 82%, 89% e 85% respectivamente.
CONCLUSÕES:O estudo com 18F-fluorodeoxiglicose apresentou melhor acurácia que os métodos convencionais de estadiamento do Linfoma de Hodgkin e foi útil para o diagnóstico não-invasivo de lesões suspeitas.
Throughout the past two decades, the prognosis of Hodgkin lymphoma (HL) has greatly improved due to earlier diagnosis and accurate staging of the disease, which has facilitated a better therapeutic approach. At the time of writing, HL has an excellent outcome that varies according to its clinical stage. Long-term survival of about 90% is observed in the earlier stages and up to 75% in the advanced stages of the disease.1
The Ann-Arbor staging system (AAS) modified at the Cotswolds meeting2 is used to define the conventional clinical stage (CS) of HL. The AAS categorizes HL into 4 distinct stages according to the number and location of the involved sites. The CS is obtained by clinical examination, computed tomography (CT) of cervical, thoracic, abdominal and pelvic regions, and bilateral bone marrow biopsy. Although CT is an imaging technique that can evidence anatomic details, featuring important information about the relationship between organs and vascularity, the detection of nodal disease is based only on morphological criteria. Based on AAS criteria, a lymph node that is greater than 1.5 cm in its longest transverse diameter should be considered involved by HL, but studies in which pathological staging was performed have demonstrated that the size of the lymph nodes is not always related to the presence of HL.3 Additionally, CT has a limited sensitivity for the detection of disease in the spleen, liver, and bone marrow. Therefore, the CS can be equivocally under- or overestimated, leading to insufficient or disproportionately aggressive therapy, respectively. Therefore, precise methods for determining the extent of the disease are essential for the best treatment choice.
In recent years, the metabolic test with fluorine-18-fluorodeoxyglucose (FDG) has proved to be a useful tool in the management of many malignancies, including HL. Fluorine-18-fluorodeoxyglucose, a radiopharmaceutical glucose analogue labeled with the positron emitter, 18Fluor, accumulates in tissues with high metabolic activity. Because HL tumor cells use glucose at abnormally high rates, the metabolic test with FDG can demonstrate in a single scan all sites involved by the disease, independent of the size and location.
Positron emission tomography (PET) with FDG, the most used technique in the USA and Europe, has high sensitivity and specificity when compared with CT and bone marrow biopsy.4–8 Also, FDG-PET is used in the investigation of residual masses, which are present in up to 60% of patients at the end of treatment, and in the evaluation of new lesions that appear after treatment.9–11 In these cases, the confirmation of the presence of viable tumor cells is fundamental for therapeutical decisions. The histopathological assessment of suspected sites is the gold-standard method for detection of residual tumor, but tissue biopsy is not a risk-free procedure, especially when mediastinal and abdominal lesions must be evaluated. In cases for which surgical diagnosis is impossible, the presence of lymphoma can be confirmed only by serial physical examination and/or CT. Thus, the diagnosis is confirmed only when a tumor progresses and the suspected lesions increase in size, delaying the beginning of a new therapy and decreasing the chances of cure.
Despite its value, dedicated PET equipment is not available on a large scale in Brazil, which precludes its application in our country. An alternative method of metabolic testing with FDG is the use of a dual-head coincident gamma camera device (CGC-PET) instead of a dedicated PET device. Both systems have almost the same spatial resolution (4-5 mm). The larger size of the gamma camera provides an increase of about 2.5 times in the axial field of view. However, the dedicated systems have an advantage in measured sensitivity by a factor of 8 to 12 over hybrid systems. This difference in sensitivity translates into difficulty in reliably detecting lesions smaller than 15-20 mm in diameter by the CGC-PET equipment.
The aim of this study was to investigate the role of the metabolic test with FDG, CGC-PET with FDG, in staging and in the evaluation of HL patients with residual masses or new suspicious lesions.
MATERIALS AND METHODSPatients. From December 1999 to September 2002, 38 consecutive unselected patients with HL were eligible for this retrospective study. Lymph node biopsies were obtained from all patients, and the diagnosis was completed according to the criteria established by the WHO classification. Eighteen patients were submitted to a baseline metabolic test using CGC-PET as part of the staging procedures, before any therapeutic approach (Group I). The remaining 20 patients were evaluated with FDG scanning due to the presence of residual masses or a new lesion found on CT or physical examination (Group II).
Metabolic test technique. All metabolic tests were performed using a dual-head coincident gamma camera (CGC-PET) device (Vertex Plus MCD/AC, ADAC Laboratories, Milpitas, CA). Patients were instructed to fast for 12 hours before CGC-PET scanning. Scans from the skull through the mid thigh were acquired 1 hour after the intravenous injection of 185-370 MBq (5 - 10 mCi) of FDG. Topographic slices of 4 mm in the axial, sagittal, and coronal planes were reconstructed. The results were interpreted by the same team of specialists (at least 2 nuclear physicians). Focal areas with abnormal uptake of FDG were considered to represent lymphoma involvement.
Conventional staging (CS) of patients (Group I). All 18 patients of Group I underwent conventional staging (CS) procedures that included CT (cervical, thoracic, abdomen, and pelvic) and bone marrow biopsy. Conventional staging was performed according to Ann Arbor stage (AAS) criteria.2
Definition of residual mass/relapse in Group II. A residual mass was defined as the persistence of a lesion greater than 1.5 cm in its longest transverse diameter localized in a previously involved site observed after the end of treatment. Possible relapse was defined as the appearance of a new lesion of at least 1.5 cm at its longest transverse diameter observed at any time after complete remission. Suspicious relapse lesions were detected by physical examination and/or CT.
Follow-up after CGC-PET with FDG in Group II. After the CGC-PET with FDG procedure, all patients of Group II were evaluated every 2 months with physical examination and laboratory analysis, every 4 to 6 months with CT. The presence of active HL was confirmed by biopsy of the suspected lesion or evident clinical progression of disease, defined as an increase of more than 25% of longest transverse diameter of the suspicious lesion, according to ASS criteria.2 In all patients, the interval between the CGC-PET with FDG procedure and the confirmation of recurrence or loss to follow-up was obtained. The patients with confirmed active disease were treated with chemotherapy according to institutional protocols.
Data analysis. In Group I patients, CS was compared to the staging obtained by CGC-PET with FDG. Furthermore, the number of involved sites in the cervical, thoracic, abdominal-pelvic, and bone regions observed by the two methods were also compared. A concordance rate of CGC-PET with FDG to CS was calculated using CS as the reference.
In patients of Group II, those with a positive scan and with lesions confirmed by biopsy or clinical progression of disease were considered true positives. Patients with a negative scan and no evidence of clinical progression during follow-up were considered true negatives. Sensitivity, specificity, positive predictive value, negative predictive value, and accuracy were calculated. For patients with a negative CGC-PET scan, the 1-year probability of recurrence was calculated by the Kaplan-Meier method.
RESULTSPatientsThirty-eight patients (18 male and 20 female) were evaluated. The median age was 29 years (range, 17-50 years), and nodular sclerosis was the most frequent histological type observed (Table 1).
Group IOf the 18 patients staged by CS, 3 (17%) were classified as stage I, 4 (23%) as stage II, 3 (17%) as stage III, and 8 (43%) as stage IV. Of the patients staged using CGC-PET with FDG, 1 (6%) was classified as stage I, 4 (22%) as stage II, 2 (11%) as stage III, and 11 (61%) as stage IV (Table 2).
Conventional staging (CS) versus staging using CGC-PET with FDG*
| CS | |||||
|---|---|---|---|---|---|
| I | II | III | IV | ||
| CGC-PET | I | 1 | 0 | 0 | 0 |
| with FDG | II | 1 | 3 | 0 | 0 |
| III | 0 | 1 | 1 | 0 | |
| IV | 1 | 0 | 2 | 8 | |
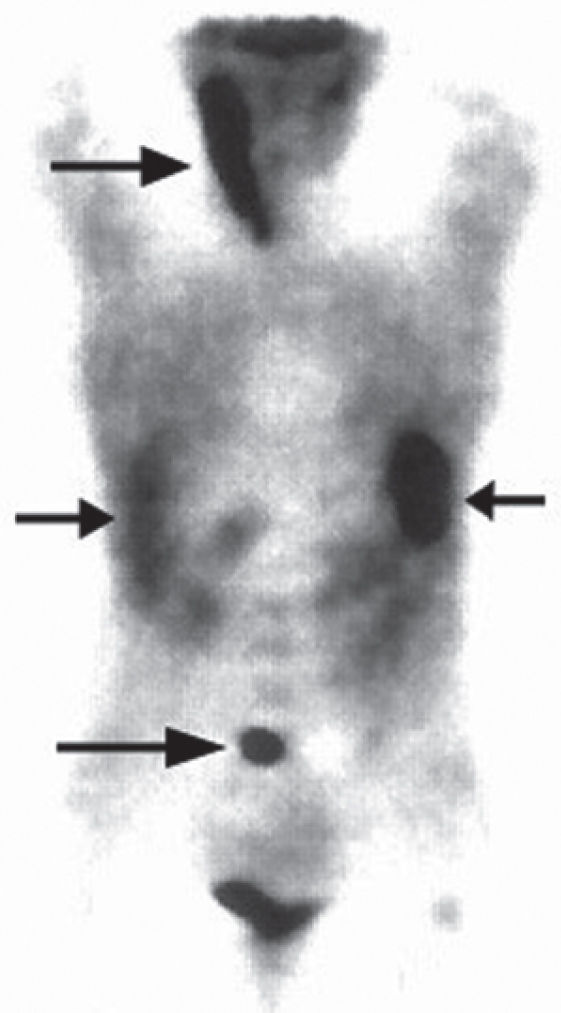
Agreement between both methods was observed in 13 (73%) of the 18 patients and discordant results were obtained in 5 (27%) patients. In all discordant cases CGC-PET with FDG resulted in upstaging (Figure 1).
Staging with CGC-PET with FDG. A 23 year-old female, who after physical examination, CT and bone marrow biopsy was regarded as having stage I disease (only right cervical lymph nodes enlargement). CGC-PET (coronal plan) demonstrated abnormal glucose metabolism (black arrows) in right cervical region, spleen, liver and lumbar spine (stage IV disease). Staging laparotomy confirmed the presence of disease in the abdominal sites (spleen and liver).
When the involved sites were evaluated, CGC-PET with FDG detected more lesions than CS performed with CT and bone marrow biopsy (Table 3). Only 1 patient had enlarged lymph nodes in the abdominal region detected by CT that were not avid to FDG.
Group IIOf the 20 Group II patients, 5 (25%) had a suspicious lesion on the cervical region, 13 (65%) in the thoracic region, and 2 (10%) in the abdominal region.
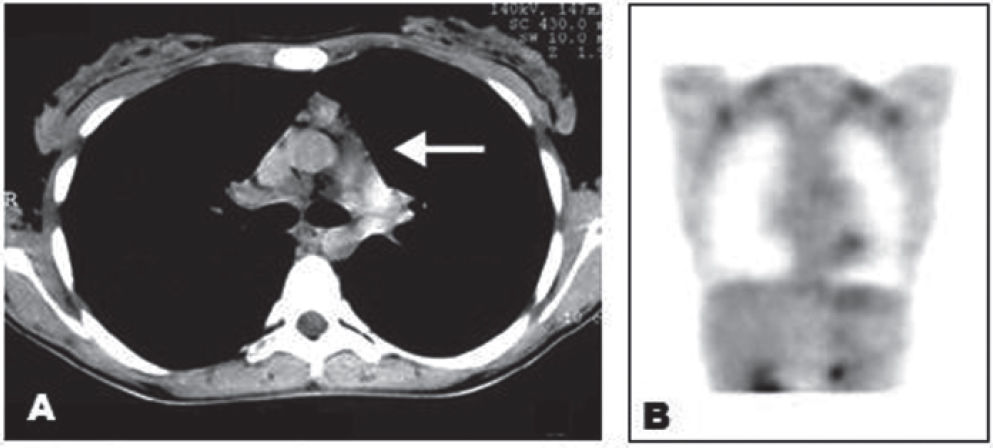
Eleven (55%) patients had positive CGC-PET scans. During a median follow-up of 26 months (range, 4-38 months), 7 (64%) of the 11 patients had disease confirmed by biopsy and 2 (18%) by clinical progression. Two other patients with positive scans underwent surgical excision of the suspected lesion. Pathologic evaluation showed only thymic hyperplasia without tumor involvement. These patients did not have any new evidence of disease through the last follow-up and were considered as false-positive cases.
Of the 9 patients with a negative CGC-PET scan, 8 (89%) did not relapse during follow-up (Figure 2). Only 1 patient had a recurrence confirmed by biopsy 3 months after the exam and was considered a CGC-PET with FDG false-negative. The 1-year probability of recurrence for CGC-PET with FDG-negative patients was 11.8%. The results of CGC-PET with FDG scanning and disease status during follow-up for all patients are summarized in Table 4.
Residual mass evaluated by CGC-PET with FDG. Panel A – Thoracic CT with evidence of residual mass on mediastinal area (white arrow) observed after the treatment in a 32-year-old female. Panel B – CGC-PET (coronal plane) of the same patient without any foci of abnormal glucose metabolism in the mediastinal area.
The sensitivity, specificity, positive predictive value, negative predictive value, and accuracy of CGC-PET with FDG were 90%, 80%, 82%, 89%, and 85% respectively.
DISCUSSIONImaging with FDG has been increasingly used in the management of oncology patients and relies on the detection of metabolic alterations observed in cancer cells instead of detection of anatomical abnormalities. Fluorine-18-fluorodeoxyglucose, a glucose analog, is taken up by metabolically active cells using a facilitated transport mechanism similar to that for glucose by means of the glucose transporters proteins. Subsequently, FDG undergoes phosphorylation to FDG-6-phosphate by hexokinases, and unlike glucose, it is not efficiently dephosphorylated by glucose-6-phosphatase (G6P); as a consequence, FDG-6-phosphate accumulates within the cell.
Malignant cells have an augmented glycolytic activity due to an increase in the membrane glucose transporters and in some of the glycolytic enzymes, such as hexokinase, as well as markedly low levels of G6P. These features lead to a higher accumulation of FDG in tumor cells. Particularly in HL, the glycolic activity and the avidity for FDG are substantially higher than in normal tissue.12
The advantage of FDG-associated imaging relative to CT is the ability to detect disease in sites without structural anatomical changes. Even in small-volume tumors, in which the number of neoplastic cells is insufficient to disrupt the normal anatomic architecture, the malignant cell metabolic activity can be demonstrated. Therefore, the presence of viable tumor cells can be detected before any increase in the volume of the affected organ.
Several studies have investigated the role of FDG for the staging of lymphoma patients. Most of these studies, using dedicated PET devices,4–8 compared the performance of FDG-PET with CS obtained by conventional methods, showing concordant results in 60% to 80% of cases, with upstaging rates ranging from 18% to 40%. The use of FDG with dual-head hybrid gamma cameras modified to recognize coincidence photons (CGC-PET) has been used as an alternative of dedicated PET devices. In the present study using CGC-PET technology, the results were similar to the ones observed with PET equipment. It is important to emphasize that biopsy confirmation of all FDG-avid lesions is unfeasible from the ethical and practical view; therefore, the true sensitivity and specificity of FDG-associated imaging for the staging of HL, performed with either PET or CGC-PET devices, is impossible to evaluate.
In our study using CGC-PET with FDG, 27.8% of the patients were up-staged when compared to conventional CS methods. Even in the cases in which the CGC-PET scan did not change the stage of the disease, CGC-PET with FDG was able to detect more involved sites per region, resulting in a better evaluation of the disease extent.
Two other groups have evaluated CGC-PET with FDG for staging of lymphomas. Tatsumi et al13 evaluated 30 patients with non-Hodgkin lymphoma, resulting in a concordance rate of CGC-PET with FDG and CT of 63%, with
CGC-PET with FDG detecting more involved sites than CT. Similarly, Pichler et al,14 in a study with 28 patients with HL and non-Hodgkin lymphoma, observed that CGC-PET with FDG detected more involved lesions than CT (100 versus 77, respectively).
In addition to staging, the metabolic test with FDG can be a useful diagnostic tool in the evaluation of residual masses observed after treatment. The challenge in this setting is the detection of tumor activity before the progression of disease, with minimum related morbidity. The use of FDG-PET has been evaluated by several authors9–11 to determine the diagnostic accuracy of PET, with observed negative predictive values ranging from 81% to 100%, and first-year relapse rates for patients with a negative PET ranging from 95% to 100%, but there are no studies using CGC-PET with FDG for this purpose as far as we know. In the present study, using CGC-PET technology, a method that has the advantage of being cheaper and more available in our country, the results observed were similar to those with the dedicated PET equipment. Additionally, more than 60% of the patients with a positive CGC-PET scan had histological confirmation of viable tumor cells in the suspected lesion. The 2 patients with a false-positive CGC-PET scan had thymic hyperplasia, a condition commonly encountered after chemotherapy for HL that can lead to false-positive scans, as previously reported with the use of dedicated PET devices.9–11
We concluded that although CGC-PET has a worse spatial resolution than dedicated PET with limitations in the detection of lesions smaller than 15 to 20 mm,15 the CGC-PET with FDG technique as performed in this study has high sensitivity and specificity; therefore, it is a useful noninvasive tool for staging and evaluation of residual masses or recurrence of Hodgkin lymphoma.