Description of some of the clinical pathological characteristics of neuroendocrine tumors of the gastroenteropancreatic tract in Brazilian patients.
INTRODUCTION:Neuroendocrine tumors arise in many organs and share common pathological features. In 2010, the World Health Organization published a new classification for neuroendocrine tumors using a three-tiered system that applies the terms neuroendocrine tumor Grade 1, neuroendocrine tumor Grade 2, and neuroendocrine carcinoma. The tumor grades are based on their mitotic rate and the Ki-67 index. In Brazil, information on neuroendocrine tumors of gastroenteropancreatic tract is scarce.
METHODS:This study investigated clinicopathological features of 773 Brazilian gastroenteropancreatic neuroendocrine tumor cases from all the geographic regions of Brazil. All of the cases emerged from the files of a single institution (a large pathology reference laboratory) between 1997 and 2009. In addition, the gastroenteropancreatic neuroendocrine tumors were graded according to the new 2010 World Health Organization classification.
RESULTS:Overall there were a higher number of neuroendocrine tumors in female over male. The lower ages were seen in patients with appendiceal tumors. The most common anatomic location involved was stomach followed by small and large intestines. All cases involving the appendix were of grade 1 and 92.1% of the neuroendocrine tumors of the esophagus were neuroendocrine carcinomas (grade 3).
CONCLUSIONS:In this series, the proportion of NET cases in the total number of surgical pathology cases at our institution over the past 12 years is increasing.
Neuroendocrine tumors (NETs) are a heterogeneous group of neoplasms composed of cells containing dense-core neuroendocrine secretory granules in their cytoplasm. These tumors are relatively rare and display a diverse spectrum of clinical presentation. Recent data from the SEER (Surveillance, Epidemiology, and End Results Program, USA) suggest that the incidence and prevalence of NETs have increased substantially over the past three decades. The main explanation for this increase is improved awareness of the disease among physicians, including pathologists, and improved diagnostic techniques. The incidence may also be increasing, but the evidence that supports this is unclear.1Approximately two-thirds of NETs are found in the gastrointestinal tract, one-quarter occur in the lungs, and the remaining cases arise in other endocrine tissues, such as the thyroid.2,3 These tumors account for approximately 2% of all malignancies of the gastrointestinal tract. Esophageal NETs are rare, and the majority are high grade, i.e., neuroendocrine carcinoma (NEC).4 In an analysis of 8,305 NETs at different anatomical sites, only three (0.04%) were reported in the esophagus.4,5 In the past, gastric NETs have been reported to account for 2 to 3% of all gastrointestinal NETs.6 Recent studies, however, have suggested that the incidence of these tumors might be higher, as much as 11 to 41% of all gastrointestinal NETs, depending on the series.4 Neuroendocrine carcinomas account for 6 to 16% of gastric neuroendocrine neoplasms.4
In the duodenum, neuroendocrine neoplasms constitute 5.7 to 7.9% of the neuroendocrine neoplasms of the digestive tract, and the proximal jejunum accounts for approximately 1% of gut neuroendocrine neoplasms.4,6 NETs of the cecum and transverse colon represent approximately 8% of all gastrointestinal NETs, while NETs of the descending colon and rectosigmoid combined represent approximately 27%.2,4,5
NETS in the gastrointestinal tract occur predominantly in the small intestine (44.7%), followed by the rectum (19.6%), appendix (16.7%), colon (10.6%), and stomach (7.2%).7 Pancreatic NETs (PETs) are uncommon, representing 1 to 2% of all pancreatic neoplasms. Pancreatic NECs account for less than 1% of all pancreatic carcinomas and less than 3% of all pancreatic neuroendocrine neoplasms.4
The previous World Health Organization (WHO) classifications for NETs of the tubular gastrointestinal tract (WHO, 2000) and pancreas (WHO, 2004) used a hybrid classification system that incorporated both staging and histological grading information into a single prognostic prediction system.8–11 The 2010 WHO classification, which was developed along with the European Neuroendocrine Tumor Society (ENETS), uses two separate and complementary classification tools —histological grading and a site-specific staging system.4,12–17
There is limited information about the gastroenteropancreatic NETs (GEP-NETs) that occur in Brazil.3,18,19,20 The purpose of this study was to describe some of the clinicopathological aspects of 773 GEP-NETs in Brazilian patients using the newly published WHO 2010 classification of NETs.
MATERIALS AND METHODSCase SelectionA total of 773 NETs cases were obtained retrospectively from the cases in the files of Consultoria em Patologia (a large anatomical pathology reference consultation service in Botucatu, São Paulo State, Brazil) dating from January 1997 to December 2009. Clinical data, including gender, age at diagnosis, and anatomic locations, were obtained for all of the GEP-NETs cases. The 2010 WHO NET classification system was applied to all of GEP-NETs, using hematoxylin and eosin-stained slides and the immunohistochemistry (MIB1 monoclonal antibodies against the Ki-67 antigen) cell proliferation index, as described previously.21–24
The pathological diagnoses of the NETs in this series considered the typical morphological findings and the expression of neuroendocrine markers, including chromogranin A and/or synaptophysin, as described previously.25
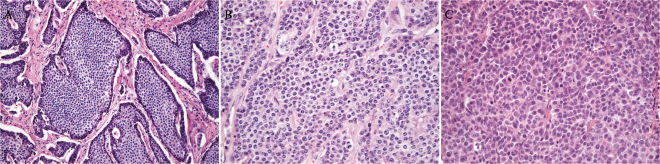
According to the WHO 2010 classification and the ENETS scheme,4,16,17 the grades were assigned as follows: G1 (NET G1/carcinoid), with a mitotic count of <2 per 10 high power fields (HPF) and/or a Ki-67 index ≤2%; G2 (NET G2), with a mitotic count of 2 to 20 per 10 HPF and/or a Ki-67 index of 3 to 20%; and G3 (neuroendocrine carcinoma), with a mitotic count of >20 per 10 HPF and/or a Ki-67 index >20% (Figures 1 and 2). The grading used in this study followed the practice of counting mitotic figures in at least fifty high power fields and using the percentage of 500 to 2000 cells counted in the areas with the strongest MIB1 antibody nuclear labeling (“hot spots”) as the Ki-67 index.4 In cases where the amount of tumor tissue was limited and an accurate mitotic count was not possible, the grading was based on the Ki-67 index alone. In cases where the mitotic count and the Ki-67 index grades differed, the highest grade was recorded. It was not possible to apply a site-specific staging system in this study; in most cases, the gross description of the tumor, including its size, was not available.
A) A G1 neuroendocrine tumor (hematoxylin-eosin, X200). Note the uniformity and the characteristic organoid growth pattern. B) A G2 neuroendocrine tumor (hematoxylin-eosin, X200). Mild atypia and coarser chromatin are observed. C) A neuroendocrine carcinoma (hematoxylin-eosin, X200). Note the cellular atypia and frequent mitotic figures.
All the results are summarized in Table 1.
The distribution of the 773 GEP-NETcases by anatomical location, gender, age, and grading.
| Anatomic Location | N° of cases | Male | Female | Age range (average) | Grade G1 | Grade G2 | Grade G3 |
|---|---|---|---|---|---|---|---|
| Esophagus | 38 (5%) | 27 (71%) | 11 (29%) | 47-85 (63.4) | 3 (7.9%) | 0 (0%) | 35 (92.1%) |
| Stomach | 190 (24.5%) | 74 (38.1%) | 116 (61.9%) | 24-87 (54) | 145 (76.3%) | 16 (8.4%) | 29 (15.3%) |
| Pancreas | 126 (16.4%) | 52 (40.9%) | 74 (59.1%) | 22-82 (52.1) | 81 (64.5%) | 35 (27.5%) | 10 (8%) |
| Small intestine | 161 (20.8) | 72 (44.7%) | 89 (55.3%) | 25-88 (57.7) | 136 (84.4%) | 13 (8.1%) | 12 (7.5%) |
| Colon | 43 (5.5%) | 14 (32.5%) | 29(67.5%) | 31-81 (55.7) | 22 (51.1%) | 7 (16.3%) | 14 (32.6%) |
| Rectum | 159 (20.5%) | 65 (40.9%) | 94 (59.1%) | 27-88 (50) | 123 (77.3%) | 10 (6.3%) | 26 (16.4%) |
| Appendix | 56 (7.3%) | 23 (41%) | 33 (59%) | 8-71 (27.6) | 56 (100%) | 0 (0%) | 0 (0%) |
| Total | 773 (100%) | 327 (42.3%) | 446 (57.7%) | 8-88 (52.8) | 566 (73.2%) | 81 (10.5%) | 126 (16.3%) |
Forty (5%) of the 773 GEP-NET cases were located in the esophagus, with the vast majority of the cases (92.1%) being G3 (NECs) (age range = 47 to 85 years; mean = 63.4 years). Esophageal NETs were more prevalent in men (71%). Dysphagia was the most frequently reported symptom.
One hundred ninety cases (24.5%) were located in the stomach. Most of the cases (84.7%) were well-differentiated NETs (G1 = 76.3%; G2 = 8.4%; age range = 24 to 87 years; mean = 54 years). Women represented 61.9% of these cases. “Polyp” was the major endoscopic finding. The tumor sizes ranged from 0.3 to 8.5 cm (average = 1.8 cm).
In the pancreas, a total of 126 (16.4%) NECs accounted for 8% of the pancreatic NETs, compared to 92% well-differentiated NETs (64.5% were G1, and 27.5% were G2) (age range = 22 to 82 years; mean age = 52.1 years), and 59% occurred in females. Hypoglycemia and diarrhea were the most frequent related symptoms. There was only one reported case of increased serum gastrin levels, which was confirmed by immunohistochemistry. The tumor sizes ranged from 0.3 to 8.0 cm (average = 2.6 cm).
Intestinal NETsIn the small intestine (161 cases or 20.8%), G1 was the most frequent tumor type (84.4%), followed by G2 (8.1%) and G3 (7.5%). The mean age at diagnosis was 57.9 years (age range = 25 to 88 years). Women were affected slightly more frequently (57.7%). The mean tumor size was 2.4 cm (size range = 0.4 to 7.0 cm).
In the colon (43 cases or 5.5%), the NET grades were divided as follows: G1, 51.1%; G2, 16.3%; and G3, 32.6%. The mean age was 55.7 years (age range = 31-81 years). Females accounted for 67.5% and males for 32.5% of the cases. Most of the colon tumors were polyps. The rectal NETs (161 or 20.5%) included 77.3% G1, 6.3% G2, and 16.4% G3; the patients' mean age was 50 years, with a range of 27 to 88 years. Rectal NETs were slightly more prevalent in women (59.1%). Hematochezia was the most frequent complaint. The tumor sizes ranged from 0.4 to 5.0 cm (average = 1.4 cm). Appendix NETs (56 cases or 7.3%) occurred at a significantly younger age than did the NETS at other sites, with a mean age at presentation of 27.6 years (range = 8 to 71 years). They were all G1 tumors and presented more frequently in women (59%). Abdominal pain was the most common complaint.
In the 773 study cases, the average age was 52.8 years, and 57.7% of the patients were female. The stomach was the most commonly involved anatomic site (190 cases or 24.5%), followed by the small intestine (161 cases or 20.8%) and the rectum (159 cases or 20.5%). The esophagus was the least commonly affected organ (38 cases or 5%).
DISCUSSIONNETs, which are defined as epithelial neoplasms with predominant neuroendocrine differentiation, arise in most organs. Most NETs develop in the gastrointestinal tract and bronchopulmonary tree.1,26
Although NETs have been considered a fairly rare disease, the SEER database suggests that their prevalence has increased dramatically over the last three decades. In fact, it is believed that the incidence of these tumors is increasing globally. It is likely that this increase is due to an increase in the actual number of cases and/or increased clinical and pathological experience with diagnosing this disease.26 In this series, we found that the proportion of NET cases in the total number of surgical pathology cases at our institution over the past 12 years is increasing (Table 2).
The distribution of the number and percentage of GEP-NET cases from 1997 to 2009 per three-year period and their percentage out of the total number of surgical pathology cases from a single pathology institution.
| 1997-1999 | 2000-2002 | 2003-2005 | 2006-2009 | 1997-2009 | |
|---|---|---|---|---|---|
| Number (%) of GEP-NETs | 27 (0.18%) | 104 (0.30%) | 186 (0.35%) | 456 (0.50%) | 773 (0.40%) |
| Total number of surgical pathology cases | 14,393 | 34,492 | 52,820 | 89,705 | 191,410 |
Overall, the gastrointestinal tract represents the site of greatest NET incidence (64.3%), followed by the bronchopulmonary system (27.9%).27 Approximately 0.46% of all malignancies are NETs of bronchopulmonary or gastrointestinal origin. GEP-NETs are substantially less common than their counterpart, adenocarcinomas; the incidence is approximately two to five cases per 100,000.2 Unfortunately, information regarding the incidence or prevalence of GEP-NETs in Brazil is virtually nonexistent.
NETs of the esophagus are rare, representing only 0.04% of all the gastrointestinal NETs reported.4,5,28 The literature clearly shows that NETs in this anatomical location occur more frequently in males in the sixth and seventh decades of life (mean age = 56 years), as our study confirms. Additionally, the literature clearly shows that the vast majority of NET cases involving the esophagus are indeed of high grade, as was also seen in our study.4,5 In our series, only three of the 38 esophageal NETs were low-grade (G1), and all of the remaining cases were NECs.
According to Modlin et al.29, gastric NETs account for approximately 6% of all gastrointestinal NETs. Most gastric NETs are well differentiated and nonfunctional. Three distinct types are recognized: Type I, associated with autoimmune atrophic gastritis; Type II, associated with multiple endocrine neoplasia Type 1 (MEN-1) and Zollinger-Ellison (SZE); and Type III, sporadic. Unfortunately, we were unable to classify the gastric NETs into these different types because we had only biopsy material for each case and not the entire specimen or detailed clinical information. In our series, the stomach was the site most frequently affected (196 cases or 24.5%) by GEP-NETs. Similar findings have been described recently by Yildiz et al.30 Most of our gastric NET cases were well-differentiated G1 and G2 neoplasms (84.7%) rather than high grade tumors (NECs), which are rarely found in the stomach.4 In most series, the most frequent anatomic location of GEP-NETs is the appendix. We believe that appendix NETs were not the most frequent type in our series because our cases were seen in consultation. Most pathologists are more comfortable diagnosing NETs in the appendix than in other anatomic locations.
PETs are rare and represent one to two percent of all pancreatic cancers. In our study, they represented 16.4% of all the GEP-NETs. Pancreatic NETs have no sex predilection and occur in a broad age range (30 to 60 years).10 In our study, we found a slightly higher prevalence in women (59.1%). Based on their clinical manifestations, PETs can be separated into functioning and nonfunctioning tumors. Functioning tumors are associated with clinical syndromes caused by inappropriate synthesis of hormones: insulinomas (27.2%), gastrinomas (12.5%), glucagonomas (8%), VIPomas (6.4%), and somatostatinomas (3.8%).10 Nonfunctioning tumors make up 39.7% of PETs. In our series, clinical information on tumor hormone production was available in only one case, which was hypergastrinemia. It is interesting to note that the vast majority of our PET cases were graded G1 or G2. High-grade PETs are also rare. We found 64.5% G1s, 27.5% G2s, and 8% G3s (neuroendocrine carcinomas-NEC) among our cases.
According to a Swedish study, the incidence of all intestinal NETs is approximately 2.0/100,000 for men and 2.4/100,000 for women.31 NETs of the small intestine have site-related differences that depend on their anatomical locations. NETs of the duodenum and jejunum represent 22% of all gastrointestinal endocrine malignancies.12 They commonly present in the sixth decade of life with symptoms of abdominal pain or bowel obstruction. Typical carcinoid syndromes are rare, manifesting in approximately 5 to 7% of patients. In our series, the small intestine was the second most affected site (161 cases). As seen in our series, the majority of intestinal NETs are well differentiated and nonfunctioning. NECs are rare and more often affect the ampulla of Vater.
NETs are found in three to nine of every 1,000 appendectomies, but they usually behave as benign neoplasms. They account for 50% of abdominal NETs. According to some series, 19% of GI NETs are located in the appendix.4,5 They are the most common tumors of the appendix, far out numbering adenocarcinomas. As in our series, the mean age at presentation is usually younger (32-43 years) than for other gastrointestinal tract NETs, and they are more common in women.4,5,32–34 Probably reflecting the good prognosis of NETs involving the appendix, all of our appendiceal NETs were well differentiated (G1).
NETs located from the cecum to the transverse colon represent approximately 8% of all gastrointestinal NETs, while NETs of the descending and rectosigmoid and colon combined represent approximately 27%.2,4,5 They are found incidentally in one out of 2,500 proctoscopies and are usually smaller than one centimeter. Their sex distribution is equal, and the average age at diagnosis is 56 years for rectal NETs and 66 years for colonic NETs.4 In our series, we observed a higher frequency in women (67.5% for colonic and 59.1% for rectal NETs). NECs are rare in the large bowel, representing approximately 0.6% of all carcinomas in this location. Nevertheless, they are more common there than in any other part of the intestine.4
A NET diagnosis is based on the clinical presentation and the blood hormonal profile, and it is always confirmed and classified by a pathologist.10,35 An immunohistochemical study is essential to confirm the neuroendocrine differentiation of neoplastic cells and define the primary site of metastatic NETs.25,36 Furthermore, immunohistochemistry is useful for evaluating the production of hormones by the neoplasm and the rate of cell proliferation through Ki-67 expression.21–24
Our series is a descriptive study of some of the clinical and pathologic characteristics of GEP-NETs, based on the files of a single institution. To our knowledge, it represents the first overview study of GEP-NETs in Brazilian patients.
ACKOWLEDGMENTThe authors thank the staff of Consultoria em Patologia for their excellent technical assistance.
No potential conflict of interest was reported.