Prevention of the development of paraplegia during the repair of the damage caused by descending thoracic and thoracoabdominal aneurysms remains an important issue. Therefore, we investigated the protective effect of atorvastatin on ischemia-induced spinal cord injury in a rabbit model.
METHOD:Thirty-two rabbits were divided into the following four equally sized groups: group I (control), group II (ischemia-reperfusion), group III (atorvastatin treatment) and group IV (atorvastatin withdrawal). Spinal cord ischemia was induced by clamping the aorta both below the left renal artery and above the iliac bifurcation. Seventy-two hours postoperatively, the motor function of the lower limbs of each animal was evaluated according to the Tarlov score. Spinal cord and blood samples were obtained for histopathological and biochemical analyses.
RESULTS:All of the rabbits in group II exhibited severe neurological deficits. Atorvastatin treatment (groups III and IV) significantly reduced the level of motor dysfunction. No significant differences were observed between the motor function scores of groups III and IV at the evaluated time points. Light microscopic examination of spinal cord tissue samples obtained at the 72nd hour of reperfusion indicated greater tissue preservation in groups III and IV than in group II.
CONCLUSION:This study demonstrates the considerable neuroprotective effect of atorvastatin on the neurological, biochemical and histopathological status of rabbits with ischemia-induced spinal cord injury. Moreover, the acute withdrawal of atorvastatin therapy following the induction of spinal cord ischemia did not increase the neuronal damage in this rabbit model.
Spinal cord injury remains a devastating complication of thoracic and thoracoabdominal aortic interventions, with a reported incidence ranging from 2.4% to 40% 1. To avoid this complication, various methods to protect the spinal cord have been suggested, including the placement of temporary shunts or performing a partial cardiopulmonary bypass, draining the cerebrospinal fluid, inducing hypothermia and administering pharmacologics. Regardless of the surgical technique or procedure used to protect the spinal cord, these methods do not entirely prevent the development of paraplegia. Current pharmacological studies on more efficacious methods include the use of steroids, oxygen-derived free radical scavengers, vasodilators and drugs designed to achieve electrical silence in the spinal cord during the ischemia-reperfusion period 2,3,4.
The 3-hydroxy-3-methylglutaryl coenzyme A reductase inhibitors (also known as statins) are the most widely used cholesterol-lowering medications. Previous clinical investigations have demonstrated that statins cause a significant decrease in the incidence of ischemic stroke in patients with and without high levels of serum cholesterol 5. Thus, it has been suggested that statins may exhibit neuroprotective properties that contribute to a reduction in the severity of the pathophysiological processes induced by the ischemic insult via a mechanism that is independent of their cholesterol-lowering effect 6. Animal studies have demonstrated that statins may be protective in ischemic stroke, most likely because of their effects on different isoforms of nitric oxide synthase (NOS), which can lead to the restoration of cerebral blood flow 7,8. Moreover, statins can decrease the extent of vascular inflammatory responses, modulate cytokine production and promote angiogenesis. Nevertheless, the neuroprotective effect of statins in ischemic stroke remains controversial 8,9,10.
In this study, we examined the neurological, histopathological and biochemical effects of atorvastatin in experimental ischemic spinal-cord injury.
MATERIALS AND METHODSThe experimental protocol was approved by the Fatih University Institutional Animal Care and Use Committee. All of the experimental animals received humane care and treatment in accordance with the “Guide for the Care and Use of Laboratory Animals” developed by the Institute of Laboratory Animal Resources, National Research Council and published by the National Academy Press, revised 1996.
Experimental protocolThirty-two New Zealand white rabbits weighing between 2.4 and 3.5 kg were initially anesthetized using intramuscular ketamine hydrochloride (50 mg/kg) and xylazine (5 mg/kg) and were administered a half-dose as required during the procedure. The animals were allowed to breathe room air without mechanical ventilation. The body temperature was maintained at approximately 38°C using a heating lamp. An ear vein and artery were cannulated prior to surgery. The arterial pressure and heart rate were continuously monitored. Preoperative cefazolin (10 mg/kg) was administered in a single dose. After the animal's abdomen was cleaned using an antiseptic solution, the abdomen was entered through a median laparotomy and the abdominal aorta was exposed inferiorly to the left renal artery and down to the level of the bifurcation. The aorta was encircled with a silk ligature distal to the renal artery and proximal to the bifurcation to facilitate performing a secure occlusion. Each rabbit was administered heparin for anticoagulation at 150 IU/kg prior to aortic cross-clamping. The aorta was occluded for 20 min distal to the renal artery using a pediatric vascular clamp and proximal to the bifurcation using a similar clamp. Following release of the aortic occlusion, the abdomen was closed in layers and the animals were allowed to recover. The procedure was performed in an identical fashion on animals in the control group but without aortic occlusion. The hemodynamic variables (blood pressure and heart rate) and body temperature were continuously monitored throughout the experiment. The arterial blood gas values were determined five minutes prior to the induction of ischemia, during ischemia and ischemia. No differences were found among the experimental groups with respect to the mean arterial blood pressure, heart rate, arterial blood gas values or body temperature.
In the atorvastatin groups (groups III and IV), 2.5 mg/kg/day atorvastatin (Lipitor, Parke-Davis, Division of Pfizer Inc., New York, USA) was orally administered; in the I/R group, a similar amount of sterile saline solution was orally administered. In group III, atorvastatin administration began 14 days prior to aortic cross-clamping and was continued for the first two days of the reperfusion period. In group IV (the withdrawal group), atorvastatin was administered 14 days prior to aortic cross-clamping but was not administered during the reperfusion period.
All of the animals were euthanized at 72 h postoperatively using a lethal cardiac injection of pentobarbital (100 mg/kg).
The animals were randomly divided into four groups with 8 animals in each group, as follows:
- I.
Control group (n = 8); spinal cord tissue and blood samples were obtained 72 h after a simple laparotomy was performed.
- II.
I/R group (n = 8); 20 min of ischemia (abdominal aortic occlusion)/72 h of reperfusion.
- III.
Experimental group (atorvastatin) (n = 8); 14 days of pretreatment with atorvastatin/20 min of ischemia/72 h of reperfusion, 2 days of atorvastatin treatment during the reperfusion period.
- IV.
Experimental group (atorvastatin-withdrawal) (n = 8); 14 days of pretreatment with atorvastatin/20 min of ischemia/72 h of reperfusion.
The neurological status of the animals was evaluated by an independent observer who was unaware of the treatment modality of the animal at 12, 24, 48 and 72 h using the Tarlov scale. The animals were classified according to their Tarlov score, as follows: 0 = no voluntary movement, spastic paraplegia; 1 = perceptible movement of the hind limbs; 2 = good movement but unable to stand; 3 = able to stand and walk; 4 = complete recovery (able to stand, walk and run) 11.
Histopathological examinationThe biopsy samples of the lumbosacral spinal cords were fixed using a 10% formalin solution for 24 h. The samples were embedded in paraffin and serial transverse sections (4-µm thick) at the lumbosacral level were obtained. The histopathology of the samples was evaluated by a pathologist who was blinded to the groups of the samples and who rated the extent of neuronal destruction using hematoxylin and eosin (H&E)-stained sections of the spinal cords. According to the extent of vacuolization of the spinal cord, the light microscopic findings were graded on a scale from 0 to +3, corresponding to no change, mild, moderate and severe changes, respectively. Cells that exhibited eosinophilic cytoplasm, had lost Nissl granules or had lost the nucleus were considered injured.
Biochemical analysesSpinal cords and serum obtained from all rabbits in each group were used for biochemical analyses. The spinal cord tissues were washed twice using cold serum physiological solutions and placed in labeled glass bottles. The bottles were stored in a deep freezer (−30°C) until processed (maximum of 10 h). The spinal cords were cut into small pieces using scissors followed by homogenization in four volumes of ice-cold Tris–HCl buffer (50 mM, pH 7.4) using a glass Teflon homogenizer (IKA ULTRA-TURRAX T-18 basic, USA) (for two minutes at 5000 rpm). The nitric oxide (NO), malondialdehyde (MDA) and protein concentrations of the homogenates were determined. The homogenates were subsequently centrifuged to remove debris. The supernatants were removed and the glutathione peroxidase (GSH-Px) and xanthine oxidase (XO) activities and the protein concentrations of the supernatants were determined. The supernatants were extracted using an equivalent volume of an ethanol/chloroform mixture. The supernatants were subsequently centrifuged at 5000 ×g for 30 min. The clarified upper layers were removed and utilized to determine the superoxide dismutase (SOD) activity and protein content. Certain values were determined at different stages of sample preparation because certain biochemical markers may undergo oxidation during the later stages of preparation. Furthermore, an extraction procedure is required for the determination of SOD activity. All of the preparation procedures were performed at +4°C. Blood samples obtained by cardiac puncture were collected into serum separation tubes. The blood samples were centrifuged at 1000 ×g for 10 min at 4°C to separate the sera.
Determination of the MDA contentA method based on the reaction with thiobarbituric acid (TBA) at 100°C was used to determine the tissue and serum MDA levels 12. The results are expressed as µmol/l for the sera samples and as nmol/g protein for the spinal cord tissues.
Determination of the NO contentDue to the difficulty in determining the NO concentration in biological specimens, the tissue nitrite and nitrate levels were determined as an index of NO production. The method used to determine the nitrite and nitrate levels in the spinal cord samples was based on the Griess reaction 13. These values are expressed as µmol/g protein for the spinal cord tissues and as µmol/l for the sera samples.
Determination of the SOD activityThe total SOD activity was determined using the method described by Sun et al. 14. The results are expressed as U/ml for the sera samples and as U/mg protein for the spinal cord tissues.
Determination of the XO activityThe XO activity was spectrophotometrically determined according to the method described by Prajda and Weber 15. The results are expressed as U/ml for the sera samples and as U/g protein for the spinal cord homogenates.
Determination of the GSH-Px activityGSH-Px activity was determined according to the method described by Paglia and Valentine 16. The results are expressed as U/g protein for the spinal cord tissues.
Determination of the myeloperoxidase (MPO) activity4-Aminoantipyrine/phenol was used as the substrate for the MPO-mediated oxidation by H2O2 to determine the MPO activity 17. The results are expressed as mU/g protein.
Determination of the protein concentrationThe protein assays were performed as described by Lowry et al. 18.
Power and sample sizeThe sample size of this study was calculated using the G*Power (G*Power Ver. 3.00.10, Franz Faul, Üniversität Kiel, Germany, http://www.psycho.uni-duesseldorf.de/aap/projects/gpower/) statistical package based on the Tarlov scores. The sample size required to achieve 80% power, α = 0.05 Type I error, β = 0.20 Type II error and f = 0.70 effect size was found to be 28, which included 7 New Zealand white rabbits in each group. To account for potential losses to follow-up, one more rabbit was included in each group and the study was conducted using a sample size of 32.
Statistical analysisThe normality of the distribution of the biochemical data for the sera and tissues were evaluated using the Shapiro-Wilk test. Depending on whether these values presented a normal distribution, the descriptive biochemical values are presented as the mean values plus the mean standard deviation or as the median (IQR, interquartile range) values.
The spinal cord vacuolization values for the groups are presented in cross-tables and the inter-group differences were evaluated using the chi-squared test. The values for the biochemical markers of each group were compared depending on the normality of the distribution of these values using the Bonferroni post-hoc one-way analysis of variance (ANOVA) or the post-hoc Bonferroni-corrected Mann-Whitney non-parametric Kruskal-Wallis analysis of variance. The statistical analyses were conducted using SPSS software (ver. 15.0, IBM, Chicago, IL, USA). A p-value of less than or equal to 0.05 was considered significant.
RESULTSBiochemical parametersThe MDA and NO levels and SOD activities in the sera and spinal cord tissues and the MPO, XO and GSH-Px activities in the spinal cord tissues are summarized in Table1.
The levels and activities of various biochemical markers in the sera and spinal cord tissues of the experimental groups.
| Control (I) | I/R (II) | Atorvastatin (III) | Withdrawal (IV) | Statistical results* | |||
|---|---|---|---|---|---|---|---|
| Serum/Tissue | Variable | Mean±SD Median (IQR) | Mean±SD Median (IQR) | Mean±SD Median (IQR) | Mean±SD Median (IQR) | F/χ2 | p |
| SERUM | MDA (µmol/l) | 0.22±0.02 | 0.32±0.06 | 0.26±0.04 | 0.27±0.03 | F = 7.055 | 0.001 |
| SOD (U/ml) | 15.73±1.13 | 10.37±0.71 | 13.58±1.10 | 14.26±0.95 | F = 42.174 | <0.001 | |
| NO (µmol/l) | 9.90 (0.76) | 11.27 (0.89) | 7.56 (0.67) | 8.06 (1.12) | χ2 = 26.960 | <0.001 | |
| XO (U/ml) | 0.08 (0.02) | 0.20 (0.12) | 0.03 (0.08) | 0.06 (0.09) | χ2 = 17.356 | <0.001 | |
| TISSUE | MDA (µmol/g) | 17.28±0.87 | 25.77±0.40 | 19.67±0.52 | 21.56±0.59 | F = 267.705 | <0.001 |
| SOD (U/mg) | 0.18±0.02 | 0.53±0.12 | 0.32±0.03 | 0.48±0.04 | F = 45.455 | <0.001 | |
| NO (µmol/g) | 0.23 (0.08) | 1.19 (0.03) | 0.92 (0.29) | 1.06 (0.51) | χ2 = 19.472 | <0.001 | |
| XO (U/g) | 0.24 (0.15) | 0.85 (0.55) | 0.29 (0.07) | 0.25 (0.04) | χ2 = 20.367 | <0.001 | |
| MPO (mU/g) | 2.53±0.43 | 4.23±0.35 | 2.88±0.55 | 3.33±0.51 | F = 20.133 | <0.001 | |
| GSH-Px (U/g) | 0.59±0.07 | 0.52±0.06 | 0.57±0.03 | 0.62±0.04 | F = 4.899 | 0.007 |
The mean serum MDA levels of the experimental groups were significantly different (F = 7.055, p = 0.001). The mean serum MDA level of the I/R group (approximately 12.10 mol/l) was significantly higher than that of the control group (p<0.001). The differences among the MDA values of the remaining groups were not significant. The control group exhibited the lowest mean serum MDA level and the mean serum MDA level of the atorvastatin group was found to be the most similar to that of the control group. The highest mean serum MDA level was observed in the I/R group.
The mean serum SOD activity was significantly different in at least one of the evaluated groups. No significant differences were observed between the SOD activities of the atorvastatin and withdrawal groups (p = 1.000), whereas the mean SOD activities of the remaining groups were significantly different from each other (p<0.05) (Table2). The SOD activity of the withdrawal group was the most similar to that of healthy rabbits (control). The lowest mean serum SOD activity was observed in the I/R group.
Results of pairwise comparisons of the biochemical markers in the sera and spinal cord tissues of the experimental groups.
| Control (I) | I/R (II) | Atorvastatin (III) | ||
|---|---|---|---|---|
| Group | p (difference)** | p (difference)** | p (difference)** | |
| SERUM MDA | I/R (II) | 0.001 (I | ||
| Atorvastatin (III) | 0.310 (nd) | 0.098 (nd) | ||
| Withdrawal (IV) | 0.274 (nd) | 0.112 (nd) | 1.000 (nd) | |
| SERUM SOD | I/R (II) | <0.001 (I>II) | ||
| Atorvastatin (III) | 0.001 (I>III) | <0.001 (II | ||
| Withdrawal (IV) | 0.035 (I>IV) | <0.001 (II | 1.000 (nd) | |
| SERUM NO* | I/R (II) | <0.001 (I | ||
| Atorvastatin (III) | <0.001 (I>III) | <0.001 (II>III) | ||
| Withdrawal (IV) | <0.001 (I>IV) | <0.001 (II>IV) | 0.083 (nd) | |
| SERUM XO* | I/R (II) | <0.001 (I | ||
| Atorvastatin (III) | 0.105 (nd) | 0.001 (II>III) | ||
| Withdrawal (IV) | 0.878 (nd) | <0.001 (II>IV) | 0.574 (nd) | |
| TISSUE MDA | I/R (II) | <0.001 (I | ||
| Atorvastatin (III) | <0.001 (I | <0.001 (II>III) | ||
| Withdrawal (IV) | <0.001 (I | <0.001 (II>IV) | <0.001 (III | |
| TISSUE SOD | I/R (II) | <0.001 (I | ||
| Atorvastatin (III) | 0.002 (I | <0.001 (II>III) | ||
| Withdrawal (IV) | <0.001 (I | 0.991 (nd) | <0.001 (III | |
| TISSUE NO* | I/R (II) | <0.001 (I | ||
| Atorvastatin (III) | <0.001 (I | 0.010 (nd) | ||
| Withdrawal (IV) | <0.001 (I | 0.959 (nd) | 0.721 (nd) | |
| TISSUE XO* | I/R (II) | <0.001 (I | ||
| Atorvastatin (III) | 0.038 (nd) | <0.001 (II>III) | ||
| Withdrawal (IV) | 0.721 (nd) | <0.001 (II>IV) | 0.105 (nd) | |
| TISSUE MPO | I/R (II) | <0.001 (I | ||
| Atorvastatin (III) | 0.848 (nd) | <0.001 (II>III) | ||
| Withdrawal (IV) | 0.011 (I | 0.003 (II>IV) | 0.377 (nd) | |
| TISSUE GSH-Px | I/R (II) | 0.062 (nd) | ||
| Atorvastatin (III) | 1.000 (nd) | 0.062 (nd) | ||
| Withdrawal (IV) | 1.000 (nd) | 0.006 (II | 0.626 (nd) |
The median serum NO level was significantly different in at least one of the groups compared with the remaining groups (χ2 = 26.960; p<0.001). No significant differences were observed between the serum NO levels of the atorvastatin and withdrawal groups (p = 1.000), whereas those of the remaining groups significantly differed from one another (p<0.05) (Table2).
The median serum XO activities of the experimental groups significantly differed (χ2 = 17.356; p<0.001). The median serum XO activities of the I/R and control groups (p<0.001) and those of the atorvastatin (p = 0.001) and withdrawal groups (p<0.001) were significantly different, whereas those of the remaining groups were similar (p>0.05) (Table2).
Tissue levelsThe mean tissue MDA levels of the experimental groups were significantly different (F = 267.705; p<0.001) (Table2). The I/R group exhibited the highest mean tissue MDA level, whereas that of the withdrawal group was most similar to that of the I/R group.
The mean tissue SOD activity of at least one group was significantly different from those of the remaining groups (F = 45.455; p<0.001). No significant differences were observed between the SOD activities of the I/R and withdrawal groups (p = 0.991). However, the SOD activities of the remaining groups were different from that of at least one other group (p<0.01) (Table2).
The median tissue NO level of at least one of the groups was significantly different from that of the remaining groups (χ2 = 19.472; p<0.001). The average tissue NO level of the control group was significantly different from those of the remaining groups (p<0.001). The median tissue NO levels of the remaining groups were similar (p>0.05) (Table2). The control group exhibited the lowest median tissue NO level, whereas the I/R group exhibited the highest median tissue NO level.
Significant differences were observed in the median tissue XO activities of the experimental groups (χ2 = 20.367; p<0.001). The median tissue XO activities of the I/R and control groups (p<0.001) and those of the atorvastatin (p<0.001) and withdrawal groups (p<0.001) were significantly different, whereas those of the remaining groups were similar (p>0.05) (Table2).
The mean tissue MPO activities of the experimental groups were significantly different (F = 20.133; p<0.001). The mean tissue MPO activities of the I/R and control groups (p<0.001), those of the atorvastatin (p<0.001) and withdrawal groups (p = 0.003) and those of the control and withdrawal groups (p = 0.011) were significantly different, whereas those for the remaining groups were similar (p>0.05) (Table2). The I/R group exhibited the lowest mean tissue MPO activity, whereas the control group exhibited the highest mean tissue MPO activity.
The mean tissue GSH-Px activities of the experimental groups were significantly different (F = 4.899; p = 0.007). The mean tissue GSH-Px activities of the I/R and withdrawal groups (p = 0.006) were significantly different. No significant differences were observed among the mean tissue GSH-Px activities of the remaining groups (p>0.05) (Table2). The withdrawal group exhibited the lowest mean tissue GSH-Px activity, whereas the I/R group exhibited the highest mean tissue GSH-Px activity.
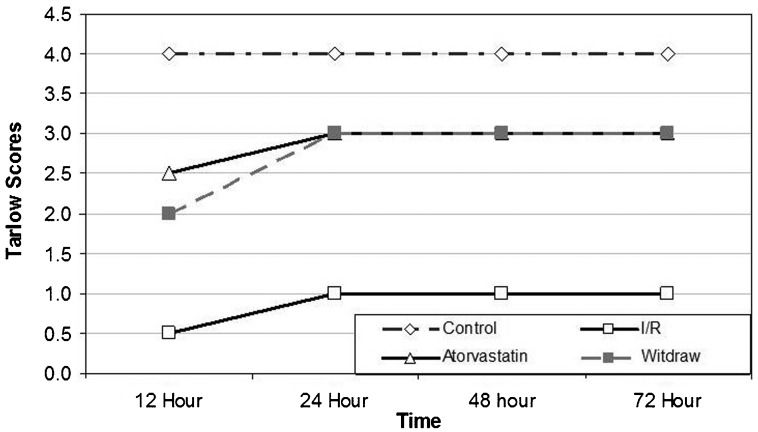
Neurological status of the treatment groupsAll of the rabbits in the control group exhibited Tarlov scores of 4 points at all of the evaluated time points. The median Tarlov scores are summarized in Table3. The median Tarlov scores of the experimental group at 12, 24, 48 and 72 hours following spinal-cord injury were significantly different (p<0.001). None of the rabbits in the experimental group regained the ability to move in a manner observed for the rabbits in the control group (p<0.001). The median Tarlov scores of the control group were higher than those of the remaining groups (p = 0.002).
Median Tarlov mobility scores of the experimental groups at selected time points following ischemic injury.
| Control (I) | I/R (II) | Atorvastatin (III) | Withdrawal (IV) | Statistical differences between the groups | ||
|---|---|---|---|---|---|---|
| Min – Max | Min – Max | Min – Max | Min – Max | |||
| Time point (h) | Median (IQR) | Median (IQR) | Median (IQR) | Median (IQR) | χ2 | p |
| 12 h | 4 – 4 | 0 – 1 | 0 – 3 | 1 – 3 | 24.266 | <0.001 |
| 4 (na) | 0.5 (1.0) | 2.5 (1.8) | 2.0 (1.8) | |||
| 24 h | 4 – 4 | 0 – 2 | 1 – 3 | 1 – 4 | 22.886 | <0.001 |
| 4 (na) | 1.0 (0.8) | 3.0 (1.8) | 3.0 (1.8) | |||
| 48 h | 4 – 4 | 0 – 2 | 2 – 4 | 2 – 4 | 22.968 | <0.001 |
| 4 (na) | 1.0 (1.0) | 3.0 (1.5) | 3.0 (1.8) | |||
| 72 h | 4 – 4 | 0 – 2 | 1 – 4 | 2 – 4 | 21.309 | <0.001 |
| 4 (na) | 1.0 (1.0) | 3.0 (2.0) | 3.0 (2.0) | |||
| Time-dependent differences (χ2; p) | na | 4.385; 0.223 | 13.824; 0.003 | 16.286; 0.001 |
na: not available; h: hours.
The median Tarlov scores in the withdrawal group were higher than those of the I/R group. No significant differences were observed among the scores of the remaining groups (p>0.05) (Figure1). The median Tarlov scores at 24 h following spinal cord injury of the control and withdrawal groups were similar (p = 0.010). The I/R and atorvastatin groups exhibited lower median Tarlov scores than that of the control group (p<0.001 and p<0.001, respectively). The Tarlov scores of the I/R group were lower than those of the atorvastatin (p = 0.007) and withdrawal (p = 0.002) groups. No significant differences were observed between the atorvastatin and withdrawal groups (p = 0.505) (Figure1).
The median Tarlov scores of the atorvastatin and withdrawal groups were similar to those of the control group at 48 and 72 h post-ischemic injury (p = 0.010 and p = 0.038; p = 0.038 and p = 0.038, respectively). The Tarlov scores of the I/R group were lower than those of the atorvastatin and withdrawal groups (p = 0.002 and p<0.001, respectively). No significant differences were observed between the scores of the atorvastatin and withdrawal groups at 48 or 72 h post-ischemic injury (p = 0.798, p = 0.878) (Figure1). No significant differences were observed in the median Tarlov scores of the animals in the I/R group at the evaluated time points (χ2 = 4.385; p = 0.223). No significant differences were observed in the hind-limb motor-function scores of the animals in the I/R group at the evaluated time points (Figure1).
The atorvastatin group exhibited a median Tarlov mobility score at at least one time point that was different from that of the remaining groups (χ2 = 13.824; p = 0.003). Because the scores at the evaluated time points were not significantly different, pairwise comparisons using a Bonferroni correction were performed to determine whether a time-dependent median Tarlov score was significantly different in the atorvastatin-treatment groups. The median Tarlov score of the withdrawal group was significantly different at different time points (χ2 = 16.286; p = 0.001) (Figure1). The hind-limb motor functions of the withdrawal group significantly improved between 12 and 72 h post-injury (Table3). The function scores at the remaining time points were not significantly different (p>0.05) (Figure1).
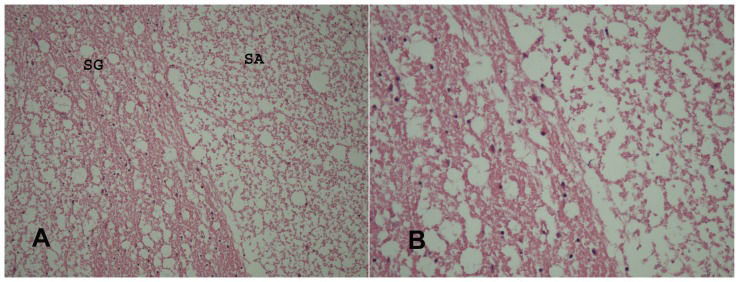
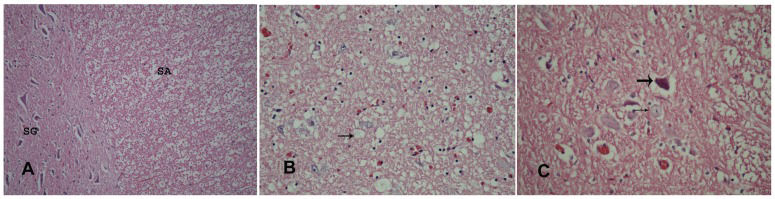
Histopathological evaluationThe vacuolization scores of the experimental groups are summarized in Table4. For the statistical analysis of these scores, the vacuolization scores were combined into two groups, as follows: group 1 included no and mild vacuolization scores, whereas group 2 included moderate and severe vacuolization scores. The distributions of the vacuolization scores according to the experimental groups are summarized in Table5. No vacuolization or mild vacuolization was observed in all of the rabbits in the control group, whereas the highest level of vacuolization was observed in the I/R group. All of the rabbits in the I/R group exhibited moderate or severe vacuolization scores. The vacuolization scores of the atorvastatin and withdrawal groups were similar. The vacuolization scores were significantly different between the experimental groups. The I/R group exhibited higher vacuolization scores than those of the remaining groups. The vacuolization scores were similar in the control, atorvastatin and withdrawal groups (Figures2 and 3).
The extent of vacuolization of the spinal cord tissue for each group.
| Vacuolization | ||||||
|---|---|---|---|---|---|---|
| Group | None | Mild | Moderate | Severe | Total | |
| Control | n (%) | 8 (100.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 8 |
| I/R | n (%) | 0 (0.0) | 0 (0.0) | 1 (12.5) | 7 (87.5) | 8 |
| Atorvastatin | n (%) | 3 (37.5) | 4 (50.0) | 1 (12.5) | 0 (0.0) | 8 |
| Withdrawal | n (%) | 2 (25.0) | 5 (62.5) | 1 (12.5) | 0 (0.0) | 8 |
| Total | n (%) | 13 (40.6) | 9 (28.1) | 3 (9.4) | 7 (21.9) | 32 |
The combined results of the vacuolization of the spinal cord samples for each group.
| Vacuolization | ||||
|---|---|---|---|---|
| Group | None or mild | Moderate or severe | Total | |
| Control | n (%) | 8 (100.0) | 0 (0.0) | 8 |
| I/R | n (%) | 0 (0.0) | 8 (100.0) | 8 |
| Atorvastatin | n (%) | 7 (87.5) | 1 (12.5) | 8 |
| Withdrawal | n (%) | 7 (87.5) | 1 (12.5) | 8 |
| Total | n (%) | 22 (68.8) | 10 (31.3) | 32 |
Spinal cord samples of the I/R group with paraplegia exhibited complete destruction of the motor neurons, with intensely eosinophilic cytoplasm, the loss of Nissl granules and the pronounced vacuolization of the substantia alba (SA) and the substantia grisea (SG). A) Hematoxylin and eosin (H&E)-stained spinal cord tissues at 200× magnification and B) H&E-stained spinal cord tissues at 400× magnification.
A) Histopathological features of the spinal cords of rabbits with healthy cells in the substantia grisea (SG) and a mild level of vacuolization in the substantia alba (SA) (H&E, 200×). B) Representative micrograph showing a moderate level of vacuolization (arrow) in the cells of the substantia grisea (H&E, 400×). C) Representative micrograph showing vacuolization, neurons containing pyknotic nuclei (thick arrow) and sparse Nissl-stained substances (thin arrow) in the cytoplasm of the large neurons in the substantia grisea (H&E, 400×).
The findings of the present study can be examined in terms of two primary endpoints. First, this study demonstrated the neuroprotective effects of pre-ischemic administration of atorvastatin in a spinal cord ischemia-reperfusion model and, second, that the acute withdrawal of atorvastatin therapy following spinal cord ischemia did not increase the extent of neuronal damage compared with continuous therapy during the reperfusion period.
Neuroprotective effectsClinical studies have demonstrated that statin therapy decreased the incidence of ischemic stroke, most likely through effects on the precerebral atherosclerotic plaques and antithrombotic mechanisms 6. Furthermore, statins have been shown to decrease the infarct size in experimental animal models of stroke. Statins upregulate the level of endothelial nitric oxide synthase (eNOS) and inhibit the production of inducible nitric oxide synthase (iNOS), effects that are potentially neuroprotective 7,8. Our study revealed a marked elevation in the NO level of the I/R group and that atorvastatin treatment significantly attenuated this increase. This increase in NO generation in the sera of the I/R group supports a mechanism that involves the generation of NO from free radicals produced under oxidative stress. The preservation of eNOS activity in the cerebral vasculature, particularly in the ischemic penumbra, is highly important in preserving blood flow and limiting the extent of neurological damage. Statins may also attenuate the inflammatory cytokine responses that accompany cerebral ischemia and they possess antioxidant properties that likely ameliorate ischemic oxidative stress in the brain 22. Simvastatin treatment has been shown to reduce the extent of ischemic brain injury and perfusion deficits in an embolic model of stroke 23.
Atorvastatin, which is a hypocholesterolemic agent, exhibits anti-inflammatory, antithrombotic and antioxidant activities 24,25. The potential anti-inflammatory activity of atorvastatin may ameliorate neurological impairment mechanisms that most likely result from the unpredictable side effects of inflammatory cascades. Several studies have indicated that atorvastatin exerts a neuroprotective effect on spinal cord injury 26. Pannu et al. 27,28 reported that atorvastatin treatment following traumatic injury of the spinal cord attenuated the levels of inflammation, neuronal apoptosis and demyelination and improved the functional outcome. Dery et al. 29 found that following experimental thoracic spinal cord contusion injury, atorvastatin was effective in preventing early apoptosis at the injury site within 2 h post-administration and in promoting locomotor recovery. Eroglu et al. 30 demonstrated that the administration of microspheres containing atorvastatin improved the functional outcome of an experimental traumatic SCI model, attenuating the expression of TNF-α, IL-1β and IL-6, lowering the lipid peroxidation levels and preserving cellular integrity. Nacar et al. 31 demonstrated that the systemic administration of atorvastatin reduced the level of expression of inflammatory cytokines, such as IL-1β and IL-6, as well as the level of lipid peroxides following experimental spinal cord injury in rats. These authors also demonstrated the beneficial effect of atorvastatin treatment in terms of the Tarlov scores. The results of our current investigation are similar to the outcomes observed by Nacar et al.
In this study, administration of atorvastatin prior to ischemia-reperfusion injury protected the spinal cord, as indicated by the improved neurological function based on a higher Tarlov score. The administration of atorvastatin (groups III and IV) resulted in a significant reduction in motor dysfunction. The improved neurological functional outcome was supported by the light microscopic observation of more intact cellular structures. The motor neurons in the animals of the I/R group were completely destroyed. The administration of atorvastatin (groups III and IV) attenuated the ischemia-induced histopathological injury. Medulla spinalis I/R injury is defined by a complex cascade of events, including the increased liberation of reactive oxygen species (ROS) from a variety of cell types. The role of ROS in I/R spinal cord injury has been examined through detection of the by-products of oxidation of target molecules (lipid peroxidation and protein oxidation) and determination of the consumption of tissue antioxidants, such as GSH. Numerous studies have shown a positive correlation between increased levels of antioxidant enzymes in the spinal cord and/or decreased levels of antioxidant defense 19,20,21.
Our study indicated that atorvastatin significantly inhibited the depletion of SOD, XO and MPO activities in spinal cord tissue. This preventive effect may be due to the free radical scavenging and antioxidant activities of atorvastatin. Moreover, atorvastatin significantly reduced the increase in the MDA concentration in rabbit spinal cord tissue. In this study, lipid peroxidation was monitored by measuring the level of MDA, which is produced from free radical damage of the membrane components of cells. We observed a significant increase in the MDA concentration in the spinal cord tissue of the rabbits in the I/R group. Atorvastatin significantly attenuated this increase in the MDA concentration. This observation is most likely due to the ROS scavenging capacity of atorvastatin. The atorvastatin-mediated protection of the spinal cord from I/R injury may also be due to the reduction of the level of lipid peroxidation in the neurons of the spinal cord. MPO is an enzyme that is expressed in leukocytes. The increased levels of MPO in the spinal cord tissue following I/R suggest leukocyte infiltration into the spinal cord. According to our findings, the MPO levels were elevated in the tissues of the I/R group and atorvastatin treatment prevented this elevation, protecting the spinal cord. In summary, we observed that atorvastatin treatment improved the extent of locomotor recovery following ischemic spinal cord injury in rabbits. This result was confirmed by the determined levels of lipid peroxidation and antioxidant enzymatic activities and the histopathological findings. These findings revealed the antioxidant activity and beneficial neuroprotective effect of atorvastatin on rabbit SCI.
Effects of the withdrawal therapyNo differences were observed in the neurological and histopathological findings of the acute withdrawal group and the group in which atorvastatin administration was continued during the reperfusion period following ischemia. Regarding the neurological functional outcome, no significant differences were observed in the motor function scores of groups III and IV at the evaluated time points. Under ischemic conditions, no significant morphological differences were observed between groups III and IV, either grossly or microscopically. However, significant differences were observed between the I/R group and the groups that were administered atorvastatin (groups III and IV). Regarding the oxidative stress parameters, no significant differences were found between the values of the serum biochemical markers of groups III and IV. However, significant differences in two markers (MDA and SOD) of tissue oxidative stress were observed in these 2 groups. Additionally, the GSH-Px activity in the spinal cord tissue of the withdrawal (IV) group was higher than that of the control (II) group. However, the effects of these differences were not reflected in the results of the neurological and histopathological examinations.
Acute termination of statin treatment may suppress the production of endothelial NO and impair vascular function 32. In our study, a marked elevation in the tissue NO level was observed in groups II, III and IV; however, no difference was observed in the NO levels of the withdrawal group and the group in which treatment with atorvastatin was continued during the reperfusion period. Gertz et al. 33 have reported that the withdrawal of atorvastatin treatment leads to the rapid abrogation of statin-mediated stroke-protective effects. However, we did not observe additional deterioration of neurological function due to the withdrawal of statin therapy compared with the group in which statin administration was continued during the reperfusion period. Furthermore, no significant differences were found between groups III and IV in the biochemical and histopathological evaluations.
This study demonstrates a considerable neuroprotective effect of atorvastatin on the neurological, biochemical and histopathological status in ischemia-induced spinal cord injury in rabbits. However, the acute withdrawal of atorvastatin therapy following the induction of spinal cord ischemia did not increase the extent of neuronal damage in this rabbit model.
AUTHOR CONTRIBUTIONSNazli Y and Colak N conceived and designed the study, analyzed and interpreted the data, and prepared the manuscript. Nazli Y and Alpay MF performed the experiments. Uysal S and Uzunlar AK analyzed and interpreted the data. Cakir O critically revised the final version of the manuscript.
No potential conflict of interest was reported.