Traditionally, chronic empyema has been treated by thoracotomy and decortication. Some recent reports have claimed similar clinical results for videothoracoscopy, but with less morbidity and mortality than open procedures. Our experience with thoracotomy and decortication is reviewed so that the results of this surgical procedure can be adequately evaluated.
MATERIALS AND METHODSFrom March 1992 to June 2006, 85 patients diagnosed with empyema were treated at Santo Tomás Hospital by the first author. Diagnosis of chronic empyema was based on the duration of signs and symptoms before definitive treatment and imaging findings, such as constriction of the lungs and the thoracic cage. Thirty-three patients fulfilled the criteria for chronic empyema and underwent open thoracotomy and decortication.
RESULTSTwenty-seven patients (81.8 %) were male and the average age of the study group was 34 years. The etiology was pneumonia in 26 patients (78.8%) and trauma in 7 (21.2%). The duration of symptoms and signs before definitive treatment averaged 37 days. All patients had chronic empyema, as confirmed by imaging studies and operative findings. Surgery lasted an average of 139 min. There were 3 (9%) complications with no mortality. The post-operative length of stay averaged 10 days. There were no recurrences of empyema.
CONCLUSIONSOpen thoracotomy and decortication can be achieved with low morbidity and mortality. Long-term functional results are especially promising. We suggest that the validation of other surgical approaches should be based on comparative, prospective and controlled studies.
The treatment of thoracic empyema has evolved since its inception by Hippocrates.1,2 Improvement of equipment and thoracoscopic techniques in the 1990s allowed for the expansion of applications of videothoracoscopy. One indication for videothoracoscopy is the treatment of empyema. There is general agreement that empyemas in the fibrinopurulent stage should be treated thoracoscopically; however, treatment at the chronic stage remains controversial. Presently, some authors3,4 advocate that patients with chronic empyema should be treated with minimally invasive techniques, such as videothoracoscopy. Roberts5 approached all empyema patients thoracoscopically in spite of having a 61.6% rate of conversion to thoracotomy. One point of contention is that thoracotomy and decortication involve increased morbidity and mortality.6,7 Importantly, there are also reports which indicate that morbidity and mortality are low when using this procedure.13,14 To that end, several thoracic surgeons consider thoracotomy and decortication to be the best treatment for chronic empyema.8–12
We have reviewed our experience with thoracotomy and decortication in the management of chronic empyema, focusing on morbidity, mortality, postoperative management and functional results.
MATERIALS AND METHODSThe Santo Tomás Hospital is a third-level medical center located in the capital city of the Republic of Panamá. This hospital receives patients from all over the country. Some of the patients come from rural areas with limited medical facilities.
This is a descriptive, retrospective and observational study. Charts of patients who were treated for empyema in the Thoracic Surgical Section between March 1992 and September 2006 were reviewed. The information obtained from the charts included sex, age, origin, habits, morbidity, etiology of empyema, blood tests, imaging study findings, results of smears, cultures of pleural fluids, biochemical parameters of empyema, signs/symptoms and their duration until definitive surgery, procedures performed before definitive surgery, length of operation, duration of chest intubation, postoperative days in the hospital, morbidity, mortality and follow-up.
Diagnosis of empyema was confirmed by one of the following criteria: (1) drainage of grossly purulent pleural fluid, (2) pleural fluid culture or Gram stain showing bacteria or (3) biochemical parameters of empyema (pH < 7.2, lactate dehydrogenase level > 1,000 IU/L, glucose level < 40 mg/dl.). Chronic empyema was defined in accordance with the American Thoracic Society staging system,15 where stage III empyema corresponds to chronic empyema or the organizing stage. Fibroblasts migrate into the pleural cavity and produce an inelastic membrane, entrapping the lung and rendering it essentially functionless. This diagnosis was corroborated by illness durations of more than 15 days before definitive treatment as well as supportive imaging findings, such as constriction of the chest cavity.
A database was created using Epi-info Version 3.2.2 to calculate the frequency and averages of the analyzed variables and to evaluate the comparisons between the analyzed variables.
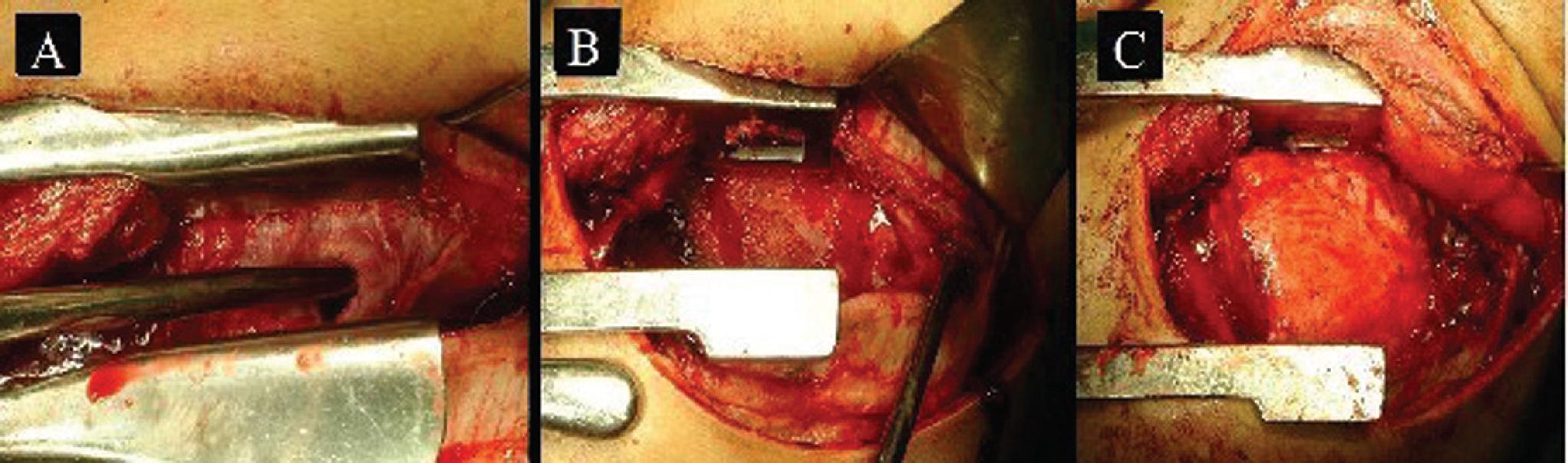
The surgical protocol consisted of double lumen intubation and placement of an epidural catheter for analgesia. The surgical approach was orientated by imaging study findings using limited incision or postero-lateral thoracotomies; the latter were used for large or loculated empyemas. Surgery included evacuation of all purulent material and formal decortication with the aim of obtaining the largest possible pulmonary expansion. In most cases, decortication of parietal pleura was partial and performed in accordance with the need for complete decortication of the visceral pleura. The diaphragm was routinely separated from the lung and from adhesions to promote as much obliteration of the empyema cavity as possible (Figure 1). Two chest tubes were inserted at the end of the operation. No pleural irrigation or fibrin sealant was used in any case.3,4,8 Patients were extubated in the operating room and sent to the ward for postoperative management. Patients were managed in the intensive care unit only when mechanical ventilation or vasopressors were required. Aggressive respiratory therapy was performed. Chest tubes were removed when there was no air leakage and when the drainage was less than 50 to 100 ml per day. Follow-up took place in the outpatient clinic and when needed, patients and primary physicians were contacted by phone.
A. Chronic empyema. Note the thickness and fibrotic nature of the pleural cortex. B. Purulent material has been removed and the visceral pleural cortex can be observed on the bottom, where it restricts lung expansion. C. The lung has been completely decorticated and there is no residual dead space
Eighty-five patients diagnosed with empyema were treated by the first author over a period of 14.5 years. Of these, 35 satisfied the criteria for chronic empyema. Two patients were excluded from analysis as they were managed with rib resection and placement of an empyema tube; these patients did not undergo thoracotomy and decortication due to high surgical risk. The remaining 50 cases were treated with tube thoracostomy, videothoracoscopy or open thoracotomy (either limited or postero-lateral) and decortication, and will not be discussed. Thus, 33 patients were managed with the previously described surgical protocol and form the basis of this study. Twenty-seven patients (81.8%) were male and six (18.2%) were female. The average age of the patients was 34 years (range 16 to 65 years). The cause of empyema was pneumonia in 26 (78.8%) and trauma in 7 (21.2%) of the patients. Of the post-pneumonic empyemas, 20 cases were pyogenic, 5 were mixed (pyogenic and tuberculous) and 1 tuberculous. In the trauma group, 5 patients suffered stab wounds and developed a clotted hemothorax and 1 patient had a gunshot wound with perforation of the esophagus. One other patient suffered perforation of the esophagus caused by a foreign body (fish bone). Fourteen (42.4%) patients were referred from Panamá City and 19 (57.6%) were referred from second-level hospitals outside Panamá City and rural areas. The most frequent habits included 20 (60.6%) patients with alcoholism, 15 (45.5%) smokers, and 8 (24.2%) drug addicts (cocaine and its variant “crack”). Comorbidities consisted of 4 (12%) patients with bronchial asthma. Diabetes mellitus type II, high blood pressure and AIDS were reported in one case each (9%).
Symptoms included coughing in 27 (81.8%) patients as well as chest pain and fever (>/= 38.5°C) in 26 (78.8%). Dyspnea was found in 21 (63.6%) patients. Twenty five (75.7%) patients had leukocytosis. The average white blood cell count was 13,560 per mm3 (range 4,400 to 31,700 per mm3), and twenty-four (72.7%) patients were anemic. The average HgB was 11.64 g/dl (range 8.3 to 16.5 g/dl) and 10.28 g/dl (range 8.2 to 13.6 g/dl) for men and women, respectively. All patients were treated with antibiotics for a variable period of time before being admitted to our unit.
Forty-four diagnostic and therapeutic procedures were performed on the 33 patients before definitive treatment. Patients underwent 25 thoracocenteses and 19 chest tube insertions (5 patients had two chest tubes). Pleural fluid was routinely cultured and bacterial growth was found in 12 (36.4%) samples. Among the assessed biochemical parameters, lactic dehydrogenase was consistently elevated, with an average value of 6,133.8 UI/L (range 1,617 to 11,250 UI/L).
All patients underwent chest roentgenography. Chest computed tomography (CT) was performed in 21(63.6%) patients, and 15 (45.5%) underwent ultrasound.
The average time prior to definitive surgery was 37 days (range 15 to 90 days). The average surgical time was 139 min (range 60 to 225 min) and the average blood loss was 531 ml (range 100 to 2000 ml). The first chest tube was removed after an average of 4 days (range 2 to 11 days) and the second tube was removed after an average of 5 days (range 3 to 17 days). Thirty patients did not have complications. Two patients developed prolonged air leakage that was managed with a Heimlich valve. In one patient, it was necessary to leave an empyema tube for 4 weeks due to purulent drainage and a residual small empyema cavity. There was no mortality or recurrence of empyemas. The average postoperative stay was 10 days (range 4 to 45 days). The patient who remained in the hospital for 45 days after thoracotomy and decortication was septic. This empyema was secondary to a delayed diagnosis of perforation of the esophagus by a gunshot wound, which necessitated prolonged mechanical ventilation. Patient follow-up examinations averaged 180 days (range 30 to 360 days).
DISCUSSIONIt is generally accepted that pleural empyema should be treated early to avoid complications, extensive operations and lengthy hospital stays.6,16 Unfortunately, there are some patients for whom early treatment is not possible and in whom chronic empyema will develop, mainly due to delayed diagnosis or delayed referral. At this stage, the standard treatment is open thoracotomy and decortication. Historically, other surgical procedures have been practiced, including open window thoracostomy, rib resection, thoracoplasty, Claggett’s procedure and percutaneous drainage guided by ultrasound or CT.17,18 With the increasing popularity of minimally invasive techniques, videothoracoscopy has been proposed for the treatment of chronic empyemas.3,4,7,19 There are reports in which open procedures have shown higher morbidity and mortality.6,7 It is for these reasons that we decided to analyze our experience with open thoracotomy and decortication in the management of chronic empyemas.
In our cases, pleural fluid cultures showed bacterial growth in 36.4% of patients, which is comparable to several previous reports.5,8–10 Additionally, lactic dehydrogenase was consistently elevated with an average value of 6133.8 UI/L. Soriano et al.16 established a direct relationship between higher levels of lactic dehydrogenase and a longer disease duration. Imaging studies consisted of chest roentgenograms, ultrasound and chest CT. These studies demonstrated a thick pleural cortex and constriction of the thoracic cage. Chest CT was particularly useful for showing the pleural cortex, loculations, size of the empyema and evidence of constriction of the thoracic cage. There are no specific indicators to confirm the chronicity of the empyemas;20 however, in this series, the presence of the pleural cortex and constriction of the thoracic cage (Figure 2) coupled with evolution times of more than 15 days was indicative of chronic empyema in all cases. During surgery, reduction of the intercostal spaces and the fibrous pleural cortex were evident; these are features of chronic empyema. In addition to showing the characteristics of the empyemas, chest CT allows the surgeon to locate and determine the best surgical approach, either limited or postero-lateral thoracotomy. Since 1996, we have routinely performed chest CT before surgery for all patients diagnosed with empyema.
A. Chest roentgenogram shows a large left empyema. B. Computed tomography of the chest showing significant restriction of the thoracic cage and thick pleural cortex. C. Postoperative chest roentgenogram with excellent pulmonary expansion (Incidentally, partial removal of a rib can be seen; this was the only patient that required such a procedure)
In the present work, it is important to note that the surgical time averaged 139 min, chest intubation time averaged four and five days, and postoperative stay averaged 10 days. Only three patients presented complications and there was no mortality. These results show shorter surgical time, shorter duration of chest intubation, fewer postoperative days and less or similar morbidity and mortality as compared to patients treated with videothoracoscopy.4,7
The definitive results of the surgical procedure were assessed using the scheme proposed by Melloni et al.,14 which takes into account elimination of symptoms, normalization of the white blood cell count, removal of pleural drains, return to pre-illness physical activities, and roentgenography. The results of all patients in this study were classified as “very good”. Symptoms resolved, white blood cell counts became normal, no patients required a new pleural drain (one patient had a chest tube converted to an empyema tube for 4 weeks), and patients returned to their regular activities by postoperative week 4. Roentgenography did not show residual pleural effusion, and pulmonary expansion was complete or slightly diminished. Spirometry for evaluation of functional results was not used on a regular basis, as there was no point of comparison since many patients were too ill to establish a pre-surgery baseline. Additionally, spirometry during illness would not reflect the real spirometric values of the patient.7
This study had several limitations; the number of cases was relatively small, although all patients were operated on by a single surgeon using the same approach and technique. The range of number of days from symptom manifestation to definitive surgery might be considered low, but these patients were classified using the staging system of the American Thoracic Society.15 In previous reports, including those utilizing videothoracoscopy4 for management of chronic empyema, the mean duration of disease before surgery has been shorter than ours. Furthermore, other reports19 have classified patients as having phase III empyema without indicating the number of days before definitive treatment. It is not always possible to recognize the exact beginning of the disease process due to the indolent presentation of the infection in many patients. Finally, we included post-traumatic chronic empyemas in this study as the aim was to evaluate the results of open thoracotomy and decortication. It has been suggested that traumatic empyema may behave differently21 and may be easier to detect, thus resulting in shorter delays in diagnosis;22 however the cases of traumatic empyema presented here fulfilled the criteria for chronic empyema.
Empyema treatment is included in the category 3b level of evidence-based medicine and expert opinions.23 In our study, open thoracotomy and decortication was found to be an excellent surgical procedure with low morbidity and mortality. Functional results were also excellent, as all patients returned to the normal activities that they performed before surgery. Open thoracotomy and decortication is the standard treatment for chronic empyema, but there have been no prospective, randomized studies comparing open thoracotomy and decortication with videothoracoscopy. Such a study is necessary to define with certainty which patients would benefit from open thoracotomy and which ones from videothoracoscopy.