Patients with Type I neurofibromatosis scoliosis with intra-canal rib head protrusion are extremely rare. Current knowledge regarding the diagnosis and treatment for this situation are insufficient. The purpose of this study is to share our experience in the diagnosis and surgical treatments for such unique deformities.
METHODS:Six patients with Type I neurofibromatosis scoliosis with rib head dislocation into the spinal canal were diagnosed at our institution. Posterior instrumentation and spinal fusion without intra-canal rib head resection via a posterior-only approach was performed for deformity correction and rib head extraction. The efficacy and outcomes of the surgery were evaluated by measurements before, immediately and 24 months after the surgery using the following parameters: coronal spinal Cobb angle, apex rotation and kyphosis of the spine and the intra-canal rib head position. Post-operative complications, surgery time and blood loss were also evaluated.
RESULTS:Patients were followed up for at least 24 months post-operatively. The three dimensional spinal deformity was significantly improved and the intra-canal rib head was significantly extracted from the canal immediately after the surgery. At follow-up 24 months after surgery, solid fusions were achieved along the fusion segments, and the deformity corrections and rib head positions were well maintained. There were no surgery-related complications any time after the surgery.
CONCLUSIONS:Systematic examinations are needed to identify patients with Type I neurofibromatosis scoliosis with rib head dislocation into the canal who can be treated by posterior-only spinal fusion without rib head resection.
Neurofibromatosis type 1 (NF1), also known as von Recklinghausen disease, involves the spine in 26% to 50% of patients (1,2). The spinal deformity can be divided into two categories: dystrophic and non-dystrophic. Non-dystrophic forms mimic idiopathic scoliosis and are treated as such. Dystrophic deformities, on the other hand, are characterized by relentless curve progression with short segmental and sharply angulated curves, which are often accompanied by severe vertebral body wedging and neural foraminal enlargement (3–6). These dystrophic curves are usually corrected via combined anterior and posterior fusion, which is also known as circumferential fusion (7–9). In some dystrophic cases, the deformities are so severe that the rib heads on the convex side of the curve penetrate into the spinal canal through the enlarged neural foramen. If unrecognized, the dislocated rib heads could lead to catastrophic injuries by impinging on the spinal cord after corrective procedures (6,10–14). Unfortunately, current knowledge about the diagnosis and surgical management of NF-1 scoliosis with intra-canal rib penetration is insufficient due to the rarity of the condition (6,10–15). Thus far, only 19 cases have been reported in the English literature (Table 1). The purpose of our study is to share our systematic experience with the diagnosis and surgical treatment of this rare and highly risky situation.
Previous Reports of Spinal Canal Rib Penetration in Patients With Neurofibromatosis Type-1.
| Author | Patients (No.) | Age (y) | Signs & symptoms | Radiology Exam | Treatment | Follow-up time |
|---|---|---|---|---|---|---|
| Abdulian et al. (10) | 1 | 14 | None | CT | R,ASF,HT,PSF,SSI | 2 years |
| Capella et al. (15) | 1 | 15 | No pre-operative symptoms; postoperative weakness and paraparesis | CT, MRI | R,ASF,PSF,SSI | 2 years |
| Dacher et al. (6) | 1 | 10 | Bilateral ankle clonus and daytime micturition | CT-M | R,ASF,PSF | 1 year |
| Deuchi et al. (11) | 1 | 12 | Weakness of the lower extremities, difficulty walking with eventual paraparesis, hyperesthesia below waist, ankle clonus and knee/ankle hyperreflexia | CT-M | HT,VCR,R | 2 years |
| Flood et al. (5) | 1 | 15 | Knee & ankle clonus | CT-M | R,ASF,PSF | Not mentioned |
| Gkioka et al. (4) | 1 | 13 | Painful rib hump, gait difficulty, bilateral Bobinski, ankle clonus, right foot drop, decreased sensation/hyperreflexia in lower limbs, and daytime micturition | CT,MRI | R,PSF,SSI | 6 months |
| Kamath et al. (12) | 1 | 13 | None | CT | ASF,PSF,SSI,R | Not mentioned |
| Koshhal et al. (32) | 1 | 16 | No pre-operative symptoms; postoperative T5 paraparesis | CT | ASF,PSF,R | 5 months |
| Major et al. (33) | 3 | 13 | Transient loss of sensation below the waist and inability to move lower extremities after fall on rib hump | CT-M | ASF,PSF,SSI,R | Not mentioned |
| 5 | None | CT | ASF,PSF,SSI,R | Not mentioned | ||
| 11 | None | CT-M | PSF,R | Not mentioned | ||
| Mukhtar et al. (3) | 1 | 10 | Right leg weakness and radiculopathy down to toes when he rolled to his right side | CT-M | R,PSF | 2 years |
| Yalcin et al. (14) | 3 | 14 | None | CT | R,PSF,SSI | Not mentioned |
| 12 | None | CT, MRI | R,PSF,SSI | Not mentioned | ||
| 6 | None | Radiographs &CT | PSF,SSI | Not mentioned | ||
| Ton et al. (24) | 4 | 14 | Mild lower limb hyperreflexia and ankle clonus | CT, MRI | PSF,SSI,R | Not mentioned |
| 11 | None | CT,MRI | R,PSF,SSI | Not mentioned | ||
| 11 | None | CT,MRI | R,ASF,PSF | Not mentioned | ||
| 9 | Right foot weakness, hyperreflexia and clonus | CT,MRI | R,ASF,PSF | Not mentioned |
ASF: anterior spinal fusion; CT-M: CT myelography; HT: halo traction; PSF: posterior spinal fusion; R: rib head resection; SSI: segmental spinal instrumentation; VCR: vertebral column resection.
Following the approval of the Institutional Review Board (IRB) of Southwest Hospital, the records of six patients (2 males, 4 females; 10–16 years) diagnosed with Neurofibromatosis- type I (NF-1) with rib head dislocation into the spinal canal at our institution between 2008 to 2011 were reviewed. The patient data are shown in Table 1.
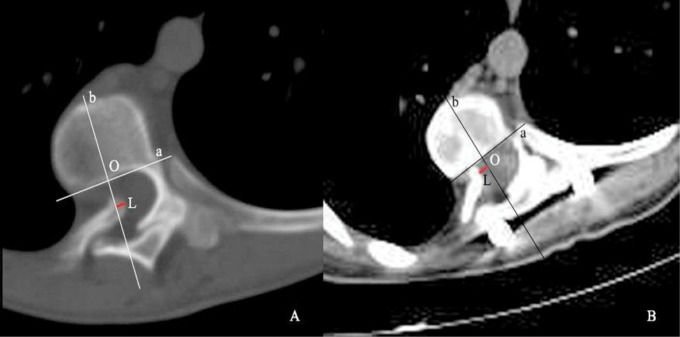
MeasurementsThe following parameters were measured pre- and post-operatively for correction assessment: the coronal and sagittal Cobb angles on plain films, the apex rotation and distance between the intra-canal rib head tip and the line bisecting the vertebral body by computed tomography (CT) scan. The coronal and sagittal deformities were measured by the Cobb method (16,17). The coronal Cobb angle was defined by the angles between the two end vertebrae (the last vertebra that tilted into the curve). Sagittal kyphosis was defined by the angles between the endplates of T2 and T12. The apex rotation was measured using the Aaro-Dahlborn method on a true axial slice (18), in which the axial slices were adjusted to parallel the orientation of the superior endplate. The distance between the intra-canal rib head tip and the line bisecting the vertebral body was measured on a true axial CT slice. It was represented by its absolute value and direction; the distance was recorded as positive if the intra-canal rib head tip passed the bisecting line of the body; otherwise, it was negative (Figure 1). Finally the correction rate of the coronal Cobb angle, kyphosis and the apex rotation and distance of the intra-canal rib head being retracted out of the canal were calculated. Magnetic resonance imaging (MRI) of the whole spine was performed on all patients to reveal any intra-spinal lesions and assess the relationship between the rib head and the dural sac.
True axial CT images of pre- (A) and 24 months post-operation (B) showed the method of recording intra-canal rib head position: Line “bo” is the bisecting line of the vertebral body; line “a” is the perpendicular line of “bo”; line “L“(red line)is the distance between the tip of intra-canal rib head and the bisecting line of vertebral body. The comparison of A and B demonstrated definite intra-canal rib head dislocation before the surgery and significant extraction after the surgery, which was maintained for 24 months after the surgery.
The measurements were performed by two orthopedic residents (D.S. &Y.Y.L.) on our PACS system and were confirmed by a senior spine specialist (F.D.). The parameters for each patient were measured five times by each observer, and reliability was determined by intra-observer and inter-observer interclass coefficients.
Surgical ProceduresThe procedure was performed with multimodality spinal cord monitoring. The patient was in the prone position, and a midline incision was made. After satisfactory exposure, pedicle screws were carefully placed bilaterally at all levels within the two neutral vertebrae except for the apex and its cranial- and caudal-adjacent levels. Afterwards, multi-level Smith-Peterson osteotomy was performed and followed by simultaneous rod rotation on the convex side and translation maneuver on the concave side. Spinal cord status was closely monitored by both transcranial electric motor-evoked potential (MEP) and somatosensory-evoked potential (SEP). Alterations in which the MEP wave amplitude decreased more than 75% and SEP amplitude decreased more than 50% compared to baseline were diagnosed as positive changes. Any correction maneuvers were stopped or even reversed if any indication of neurological impairment was noted. In addition, intra-operative “wake-up” tests were performed at the end of the reduction procedure to confirm. The spinal fusions were accomplished in an extended fashion, which means that the one or two levels above and below the neutral vertebrae at each end were instrumented and grafted with autograft and allograft bones. A cell saver was used in all surgeries. After being discharged, the patients were required to wear a thoracic-lumbar vest for at least four months to protect the fusion site.
Statistical analysisThe measurements were analyzed with SPSS 13.0 (SPSS Inc, Chicago, IL). Paired t-tests were used to determine the difference of parameters. Significance was defined as a p<0.05 and reported as such.
EthicsThis study was approved by the Institutional Review Board (IRB) of Southwest Hospital, Third Military Medical University. All procedures in the study were in accordance with the ethical standards of the IRB of Southwest Hospital and with the Helsinki Declaration.
RESULTSPre-operative examinationAll six patients displayed multiple cafe au lait spots on the skin and were neurologically asymptomatic. Intra-canal rib head dislocation was detected by pre-operative CT and MRI examinations (Figure 2). There were no signs of cord compression or intra- or para-spinal neurofibromatosis on the pre-operative MRI.
Pre-operation radiology examination detected intra-canal rib head dislocation. A) Preoperative CT sagittal image showed the intra-canal portion of dislocated rib head (white arrow); B) 3D reconstruction image of the same patient showed rib head(R) dislocation into the canal; C) MRI demonstrated the intra-canal rib head(R) did not compress on the cord(C), and the boundary(white arrow) between the rib head and the cord was clear.
All six NF-1 patients with rib head dislocation underwent posterior-only approach correction and instrumentation without rib head resection. The average blood loss was 1020±80 ml, and the average surgery time was 238± 63 minutes. Three of the patients required an intra-operative transfusion, which averaged 667±56 ml. No neurological impairment, intra-canal hematoma, dural tear or other form of complication was reported after surgery.
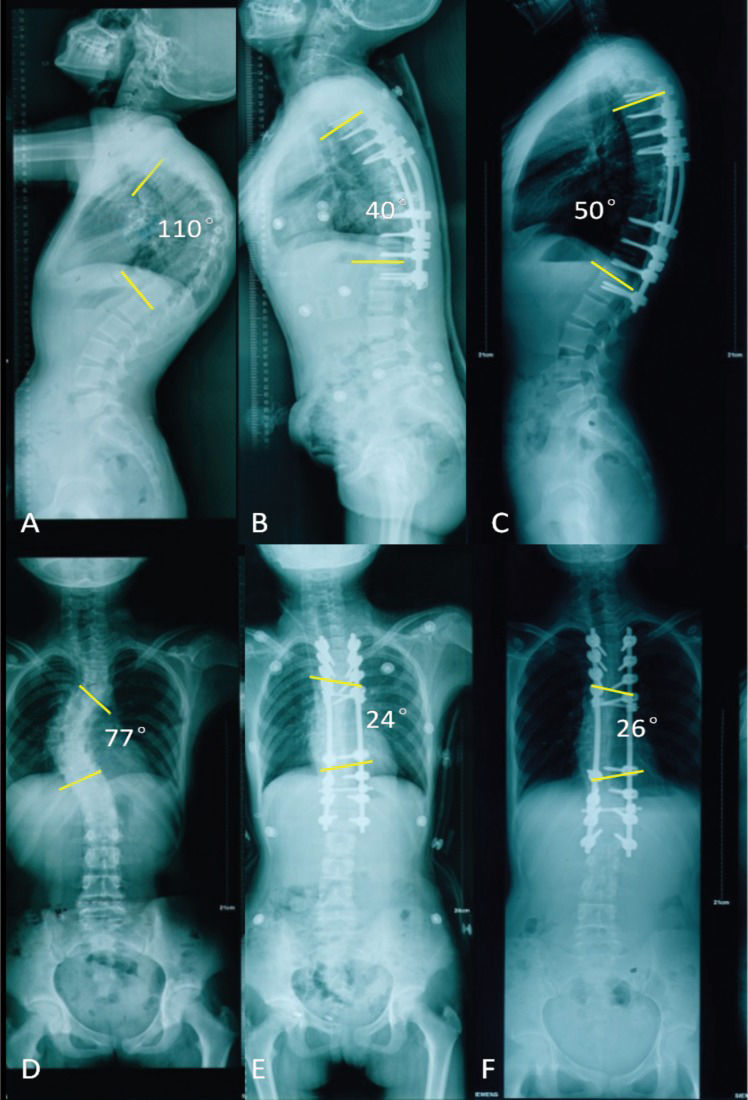
The spinal deformity parameters, radiology and patients' postures at pre-operation, immediately post-operation and 24 months post-operation are shown in Table 2, Figures 3 and 4.
Comparison of pre-and post-operative radiology measurements.
Pre-operative, immediate post-operative and 24 month post-operative radiographs. The coronal Cobb angles (A-C) were defined by the angles between the two end vertebra(yellow lines), and sagittal kyphosis (D-F) was defined by the angles between T2 and T12(yellow lines). A and D)The preoperative coronal and sagittal images showed sharp and short segmental coronal deformity and significant sagittal hyperkyphosis in the thoracic region; B and E) The immediate post-operative coronal and sagittal images showed significant correction of the deformity in both planes; C and F) The 24 month post-operative coronal and sagittal images showed the well-maintained correction of deformity in both planes, solid fusion within the fused regions was achieved, and all the implants remained in position.
Pre-operative, immediately post-operative and 24 month post-operative photos of patient postures. A and D) The preoperative anterior and posterior(AP) views and lateral view showed multiple cafe au lait spots on the patient's skin and significant hyperkyphosis posture; B and E) The immediate post-operative AP and lateral view showed significant improvement of postures; C and F) 24 month post-operative AP and lateral view showed well-maintained body posture in both views; the incision healed well.
To evaluate the efficacy of the surgical correction, we compared the deformity parameters pre-operation and immediately after the operation (Table 2 and Figure 3A, B, D, E). The coronal Cobb angle, kyphosis and axial rotation were significantly reduced after the surgery in all patients. The average correction rate of the coronal Cobb angle was 47.4%, and that of kyphosis was 58.6%. The correction rate of apex rotation was 44.4%. These improvements corresponded to a change in the patients' posture before and after the surgery (Figure 4A, B, D, E). In addition, the intra-spinal rib head tips were retracted away from canals by 5.18±2.6 cm. These results suggested that our procedures significantly corrected the spinal deformity and the intra-canal rib head dislocation.
Because dystrophic NF-1 patients are more likely to develop pseudoarthrosis after posterior-only spinal fusion, all patients were followed up for at least 24 months. All of the deformity parameters at 24 months post-operation were compared with those immediately after surgery (Table 2 and Figure 3B, C, E, F), and there was no significant difference between the two groups. There was also no significant difference in the relative position of the rib heads being extracted from the canal. The maintenance of deformity corrections was also supported by the patients' posture 24 months after surgery (Figure 4C, F). Solid fusion was confirmed on radiology at 24 months after surgery, and implant failure and screw pull-out (Figure 3 C, F) were not observed. These results indicated that solid spinal fusions were achieved and all of the corrections were well-maintained 24 months after the surgery.
ReliabilityThe repeated measurements demonstrated good inter-operator reliability and intra-observer reliability (Table 3).
DISCUSSIONMultiple manifestations are associated with NF-1, and 26% to 50% of individuals with this disorder show spinal abnormalities. Two general curve patterns have been widely recognized: Type I curves are characterized by scoliosis of 20 to 40 degrees and normal sagittal curvatures (kyphosis less than 50 degrees), which is known as an idiopathic scoliosis-like curve pattern; Type II curves are short, angulated dystrophic curves with angles of kyphosis more than 50 degrees. The latter type is accompanied by rib-penciling, vertebral scalloping, severe apical wedging and rotation, enlargement of the foramina, and para-vertebral tumors (1,2,8,19–21). Occasionally, the rib heads dislocate into the spinal canal and lead to subsequent neurological impairment (10,12,14,15). Due to the rarity of this particular condition, evidence-based diagnosis and surgical treatments on this deformity have been insufficient, which presents risks to patients with this condition (20,24).
So far, only 12 studies with a total of 19 involved patients have been previously reported (Table 1). These included 11 males and 8 females with a mean age at presentation of 14.1 years (range: 5 to 16 years). Rib head dislocation occurred on the convex side of the curve, usually around its apex. The mean curvature was 68 degrees (range: 29 to 92 degrees). Eight patients showed preoperative neurologic signs or symptoms, whereas 11 did not. All patients underwent rib head resection, and 11 had combined or staged anterior and posterior spinal fusion and segmental spinal instrumentation. Eight patients underwent stabilization with only a posterior spinal fusion and segmental spinal instrumentation. Among all of the reported cases, only a few were followed up over a long term to evaluate the outcomes.
The diagnosis of NF-1 dystrophic scoliosis can be made based on typical clinical features, such as multiple cafe au lait spots on the skin and a characteristic curve pattern on radiology (10,14,15,24). It is fairly important that clinicians are able to identify this disease early. In contrast, the neurological symptoms of NF-1 with intra-spinal rib head dislocation are varied, ranging from mild sensory and motor deficits to paraplegia and paraparesis, with approximately 60% of documented cases being asymptomatic (12). Therefore, we believe intensive radiology examinations are most reliable for finding intra-canal dislocations. CT myelography may have added benefit in detecting intra-canal dislocations but should be weighed against the risks by the clinician, as these risks include adverse reactions to the contrast, iatrogenic headache, nerve injury, or bleeding due to the spinal needle. In our study, we included several steps to aid with the diagnosis and surgical decision-making. First, thin slice (1 mm) CT and 3D reconstruction of the entire spine was performed before and after surgery to detect the dislocation pre-operatively and confirm rib head retraction post-operatively, as it has been reported that the rib penetration can be missed pre-operatively even with CT scanning (10). The CT gantry was adjusted individually to parallel the superior endplate of the scoliotic vertebral body, as the intra-canal rib head can be easily under-recognized in routine CT examinations (24). In addition, whole spine MRI was also performed to demonstrate intra-canal and paraspinal soft tissue details. Rib head dislocations were detected on the axial CT slice and 3D reconstruction. All of the dislocated ribs were on the convex side of the curve and were from the levels at the peri-apical regions. Therefore, we suggest that slices from these regions should be carefully inspected. Furthermore, MRI scanning demonstrated the relationship between the cord and intra-canal rib heads, which was also important to clarify the intra-canal deformity and assist with surgical decision-making.
It is generally accepted that if any neurological symptoms are present due to spinal cord compression from intra-canal rib head dislocation, it is necessary to resect the compressing part. In contrast, if the patient shows no neurologic symptoms, whether to resect the dislocated rib head in the canal remains controversial. As a result, current surgical approaches to this situation vary greatly among surgeons. Crawford (21,22) and Abdulian et al. (10) believed that the rib head would impale the spinal cord in the correction process; therefore, intra-spinal rib heads needed to be resected before the correction procedure. It was also reported that patients with dislocated rib heads were predisposed to spinal cord injury after a traumatic event (23). The only case without resection of the rib head was reported by Yalcin et al. (14), who claimed that the intra-canal rib head had moved away from the spinal cord while the apex was translated to the concavity. However, the reliability of this claim was questioned because it was based on a single case without any long-term follow up. In our study, we had six consecutive patients with at least 24 months of follow-up. We feel our study guides identification and care of patients with such a deformity. To quantify the extraction effect on the intra-canal rib head, we used the line bisecting the vertebral body on a true axial CT cut as the reference line and measured the distance between this line and the intra-canal rib head. As demonstrated in our postoperative results, the rib head had been extracted out of the canal significantly and remained extracted 24 months after surgery. The benefit of reduction without rib head resection was that we could avoid the risk of impaling the spinal cord or tearing the dural sac while achieving good reduction.
Another innovation in the surgical management of our study was that we used a posterior-only approach for spinal fusion and segmental instrumentation. A high incidence of pseudarthrodesis has been reported in dystrophic NF-1 scoliosis, and circumferential spinal fusion via a combined anterior and posterior approach was recommended as the standard treatment (1). At least three groups have reported alarmingly high failure rates (63%–72%) with posterior-only fusion of dystrophic NF-1 scoliosis (8). However, those surgeries frequently involved forms of internal fixation now considered biomechanically inferior to pedicle screw-rod systems (25). An anterior and posterior combined approach necessitates more extensive surgery and therefore carries a higher risk of complications, including decreased respiratory function and excessive bleeding from the plexiform venous channels that are sometimes associated with neurofibromatosis. Several authors (8,18,26,27) have proposed and performed posterior vertebral body resection (pVCR) and circumferential spinal fusion in treating dystrophic scolio-hyperkyphosis. However, this procedure utilizes a challenging technique and should only be performed by a highly experienced surgical team (28). Therefore, the posterior-only approach with extended fusion levels in our study has the advantage of being less invasive and less technique demanding. In our study blood loss and surgery time was limited to approximately 1020 ml and 238 min with a posterior-only approach, which was relatively less invasive than the combined approach (9,29-31). The corrections on three planes were also significant, as demonstrated by the results, and were well maintained at the two-year post-operative follow-up. These outcomes validated the efficacy and reliability of the posterior-only approach in treating NF-1 dystrophic scoliosis.
Limitations and future directionsOur study is not without limitations. Due to the rarity of NF-1 dystrophic scoliosis with rib head dislocation, more extensive studies should be conducted to better understand the natural history, diagnosis and management of this deformity. In addition, the parameters describing intra-canal rib head dislocation still need further verification and improvement. Our study did, however, include more cases of this unique situation than have been previously reported in the English literature; we feel this study was strong enough to provide some primary guidelines in caring for NF-1 dystrophic scoliosis patients without any neurological symptoms.
NF-1 dystrophic curves with rib head dislocation into the canal can be treated by extended segmental instrumentation and fusion without rib head resection via a posterior-only approach. Appropriate surgical candidates should be carefully selected prior to any procedure; inclusive pre-operative evaluation and sufficient intra-operative exposure and monitoring are necessary to improve surgical outcomes.
co-first authors
Sun D and Dai F contributed equally to the study and are considered co-first authors. Sun D drafted the manuscript. Dai F and Xu JZ performed surgery and commented on the manuscript. Sun D and Liu YY collected and analyzed the data.
No potential conflict of interest was reported.