In the last 25 years, liver transplantation in children has become an effective, definitive, and universally accepted treatment for terminal liver diseases. Long-term survival exceeds 80% and improves each year as the result of constant technical advancements and improvements in immediate postoperative intensive care and clinical control.
Approximately 60% of transplants in children are indicated for biliary atresia. Other conditions include virus- or drug-related fulminant hepatitis, biliary hypoplasia, alpha-1 antitrypsin deficiency, tyrosinemia, Wilson's disease, primary sclerosing cholangitis, and autoimmune hepatitis (1).
Until July 2006, the transplant waiting list in Brazil was organized in chronological order, i.e., the first person on the list was the person who had registered first. Currently, the list is sorted by severity, i.e., all candidates are given a score (Pediatric End-Stage Liver Disease [PELD] for children and Model for End-Stage Liver Disease [MELD] for adults) that takes into account serum albumin levels, prothrombin time, bilirubin levels, and other data. The first person on the list is now therefore the one who is in the most critical situation (i.e., has the highest score).
DONORThe acceptance of a potential donor requires the following: ABO compatibility, normal or only slightly altered liver function tests, and hemodynamic stability. Because the transplant waiting list is a single regional list, most donors for children are adults.
When an adult liver is transplanted to a child, it is necessary to reduce the liver size by transplanting only the left lobe. When the discrepancy between the weights of the donor and recipient is very large (or when a living donor transplant is used), only the left lateral segment is used. When a brain-dead donor is in a stable hemodynamic condition and has normal liver function tests, it is possible to use the left lateral segment for a child and the right lobe for an adult recipient (this case is called split liver).
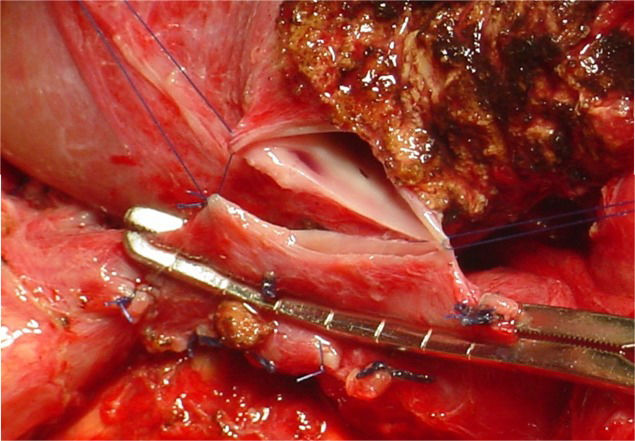
RECIPIENT'S SURGERYHepatectomy of the recipient is usually difficult due to portal hypertension, previous portoenterostomy, intestinal adhesions, and coagulation disorders. To remove the diseased liver, it is necessary to clamp the inferior vena cava in the supra- and infrahepatic region and the hilar structures. When the whole liver or the left lobe is used, the retrohepatic inferior vena cava of the donor is transplanted along with the graft. The process begins with anastomosis of the suprahepatic vena cava followed by the infrahepatic vena cava. In left lateral segment transplants, the left suprahepatic inferior vena cava of the recipient is anastomosed. The portal vein and hepatic artery are then reconstructed, and finally, the biliary tract is restored by Roux-en-Y biliary-digestive anastomosis (Figure1).
In children with liver cirrhosis and established collateral circulation, total clamping of the inferior vena cava causes a decrease in blood pressure that is usually easily manageable by volume administration. However, children with acute liver failure do not present with collateral circulation, and there may be greater hemodynamic repercussions due to blockage of the vena cava. In such cases, one alternative is to perform only a partial clamping of the inferior vena cava for end-to-side anastomosis with the hepatic vein of the graft (Figures2 and 3).
The initial neurological evaluation is difficult due to the influence of anesthetic drugs, the metabolism of which is altered by abnormal liver function and possible abnormal kidney function. The level of consciousness is an accurate parameter for assessing the function of the newly transplanted liver; therefore, it is imperative that drugs with sedative effects, especially benzodiazepines (which undergo hepatic metabolism), be avoided during the early postoperative period.
Seizures may occur in up to 30% of children following liver transplantation (2,3). Hypoglycemia, electrolyte disturbances (including hypomagnesemia), and very high serum levels of immunosuppressive drugs, such as cyclosporine or tacrolimus, are among the causes of seizures. Any generalized tonic-clonic seizures of unknown cause and all focal seizures should indicate the use of cranial computed tomography to evaluate the possibility of central nervous system bleeding.
A nonfunctional primary graft causes cerebral edema and increased intracranial pressure, often requiring an intracranial pressure monitor to better manage and maintain cerebral perfusion pressure.
Respiratory concernsAlmost all patients arrive at the ICU with an endotracheal tube, although extubation of stable patients is usually possible within 48 hours. The need for longer ventilatory support may be associated with increased respiratory demand due to pulmonary edema, pleural effusion, atelectasis, increased carbon dioxide production, or airway infection or obstruction. In addition, decreased ventilatory capacity due to respiratory depression caused by excessive sedation, liver dysfunction, malnutrition, or metabolic disorders may also be associated with the need for longer ventilatory support.
Fluid overload causes pulmonary edema and pleural effusion, typically on the right side. This effusion involves ascitic fluid that is displaced through the right diaphragm, which can be injured during surgery due to the negative pressure in the pleural cavity. Treatment consists of the use of diuretics and volume restriction because the effusion is self-limited and does not require drainage. A chest tube may be inserted to drain the liquid and allow lung expansion, but this is only done in cases involving respiratory compromise.
In some cases, the effusion starts to form again after a month, leading to ventilatory restriction that requires punctures (sometimes repeatedly). Recurring effusion is usually associated with hepatomegaly and ascites and can occur concurrently with suprahepatic anastomotic stenosis (a condition similar to Budd-Chiari syndrome) (4).
Electrolyte disturbances, such as hypophosphatemia, hypocalcemia, hypomagnesemia, and hypokalemia, may lead to respiratory muscle dysfunction and difficulty in extubation.
Lung atelectases are important causes of respiratory distress, especially in very young children with ascites and abdominal distension. Attempts to wean chronically undernourished individuals from ventilation before feeding are useless and harmful because they merely lead to increased energy consumption and fatigue.
Finally, both pulmonary and systemic infections are a frequent cause of respiratory dysfunction in the early postoperative period after liver transplantation.
Cardiovascular concernsAll patients should continue to receive electrocardiographic monitoring and be monitored with invasive and noninvasive blood pressure-measuring devices and central venous pressure-measuring devices.
Over 70% of patients present with hypertension, which often requires drug-based treatment (5). The cause of this hypertension is multifactorial, involving volume overload, elevated renin levels, and the use of steroids and calcineurin inhibitors. Hypertension is particularly dangerous due to its frequent association with coagulopathy and thrombocytopenia. In addition to the use of diuretics, the use of sodium nitroprusside is frequent in the first days after surgery, and oral medications, such as amlodipine and eventually angiotensin-converting enzyme inhibitors, are gradually introduced.
The presence of hypotension is associated with liver dysfunction, abdominal bleeding, and systemic infections. Finally, approximately 30% of patients may have episodes of bradycardia of unknown cause, without any hemodynamic repercussions (6).
Fluids and electrolytesPatients usually experience hypervolemia after surgery, and the intravascular compartment can be expanded, normal, or reduced in volume. Heart rate, central venous pressure, arterial pressure, and urine output should be monitored to calculate the initial water requirement, which is usually restricted to 60-80% of baseline maintenance. Dilutional hyponatremia is commonly observed, with increased total body sodium; therefore, this electrolyte should not be added to the maintenance fluid. Due to cell lysis in the transplanted organ during the ischemia-reperfusion process, there is a tendency toward hyperkalemia; thus, potassium should also not be added to the fluid.
Commonly, there is a need for a packed red blood cell transfusion during the intraoperative period; the citrate anion present in stored blood chelates the calcium ion, resulting in a tendency toward hypocalcemia in the immediate postoperative period.
Hypoglycemia occurs in graft dysfunction; however, there is a tendency toward hyperglycemia when the liver is functioning well due to the stress caused by the surgical procedure and the use of corticosteroids. A 5% glucose solution is therefore initially used, with periodic monitoring of blood glucose levels.
Gastrointestinal concernsAfter transplantation, there is risk of ulceration of the stomach and duodenum due to stress and steroid therapy. All patients should therefore receive gastric acid secretion blockers.
When gastrointestinal bleeding is present, coagulation abnormalities should be assessed, and anticoagulants and antiplatelet drugs may be discontinued. Upper gastrointestinal endoscopy is an important resource for the diagnosis and treatment of gastrointestinal bleeding in most cases. When bleeding esophageal varices are present or when the source of bleeding is not diagnosed by endoscopy, emergency Doppler ultrasound of the abdomen is required because this bleeding can be a manifestation of portal vein thrombosis.
As noted, most of the indications for liver transplantation in children involve biliary atresia with previous portoenterostomy. Thus, during the recipient's surgery, it is necessary to release large numbers of adhesions between the bowel loops and liver. It is not uncommon for accidental perforation of these loops or seromuscular injuries to go unnoticed. The early postoperative immunosuppression state of the transplant hinders the healing process and masks the signs and symptoms of perforated acute abdomen. Abdominal reexploration is indicated whenever there is any doubt regarding abdominal pain, increased nasogastric tube output, or prolonged ileus.
Treatment of the liver graftIschemia-reperfusion leads to characteristic injuries in the newly transplanted liver that are known as preservation injuries. The histology of the post-reperfusion biopsy reveals neutrophilic infiltrate in the sinusoids and hepatocyte apoptosis. The progression of this injury is evidenced by cell ballooning and cholestasis (7). Preservation injury, which is present to some degree in all cases, produces a characteristic enzymatic curve in which there is a linear increase in serum hepatocyte enzymes starting from the first postoperative day and then a decrease from the fourth to fifth day. The levels of canalicular enzymes (particularly gamma-glutamyl transpeptidase or GGT) increase more gradually and slowly decline from the seventh to the tenth postoperative day.
Primary graft dysfunction is the most common cause of early graft loss and is characterized by acute liver failure (e.g., encephalopathy, coagulopathy, and hemodynamic instability), significant elevation in serum liver enzymes (AST/ALT above 2,500 IU/L), and multiple organ failure (kidney failure and pulmonary complications).
The cause of primary graft dysfunction is the irreversible loss of hepatocyte function due to ischemia-reperfusion injury. The risk factors include a donor age greater than 50 years, macrosteatosis (greater than 30% of hepatocytes), severe donor hypernatremia (greater than 170 mEq/L), and prolonged cold ischemia time (over 18 hours) (8).
There is no effective treatment for primary graft dysfunction, and patient survival depends on early retransplantation.
Vascular occlusionsHepatic artery thrombosisThrombosis of the hepatic artery is the most common vascular occlusion, especially for living donor transplants, in which anastomosis is performed between smaller arteries (8). It is a catastrophic complication and may present as acute liver failure, biliary fistula, intermittent fever, or asymptomatic elevation of enzymes. Hepatic artery thrombosis and biliary complications are correlated because irrigation of the biliary tract is exclusively arterial.
Arterial thrombosis in recipients of cadaveric grafts typically manifests in the first two weeks as fulminant hepatic necrosis with rapid clinical deterioration. Large increases in hepatocyte enzymes and worsening of encephalopathy and coagulation are observed. Late occlusions may be asymptomatic and may involve the formation of collaterals that supply the liver.
Diagnosis is made based on the absence of flow in Doppler ultrasound, which is performed daily during the first week after transplantation, with sensitivity rates that reach 100% depending on the experience of the examiner. Emergency surgical reexploration and thrombectomy may be indicated in cases of early occlusions (9). In most patients, thrombosis recurs, indicating the need for retransplantation. A peculiar and interesting aspect of living donor transplants is that within the first few days after surgery, hepatic artery thrombosis progresses silently without clinical or laboratory manifestations, and a diagnosis may only be performed by ultrasound examination.
Antiplatelet agents are used for the prophylaxis of arterial thrombosis. When the International Normalized Ratio (INR) levels are less than or equal to 3.0, intravenous heparin infusion is initiated at a dose of 100 U/kg/day, which is maintained for 15 days.
Portal vein thrombosisThis condition is less frequent than hepatic artery thrombosis. It manifests as liver failure (in early thrombosis), complications of portal hypertension, such as variceal bleeding and encephalopathy, or an asymptomatic elevation in enzymes. Diagnosis is performed by Doppler ultrasound, and a positive diagnosis indicates the need for a new surgery during early thrombosis; the success rate of this approach is satisfactory. Late cases are usually asymptomatic or present as portal hypertension, which tends to be compensated for over time.
Obstruction of the hepatic veinsIn cases of transplantation of the left lateral segment (end-to-side anastomosis of the left hepatic vein in the cava of the recipient), the hepatic vein may be obstructed (4,11). Thrombosis itself is rare, and stenosis is most frequently observed in this anastomosis starting at one month after transplantation. Obstruction of the hepatic vein presents as hepatomegaly and ascites, which is sometimes responsible for the formation of a high-volume pleural effusion that leads to respiratory failure.
Doppler ultrasound can detect large increases in blood flow velocity in the region of the anastomosis; thus, cavography is indicated. Interventional radiology can dilate the region of stenosis or a stent can be fitted, with immediate relief of symptoms (4,11).
Biliodigestive anastomotic dehiscenceBiliary complications typically occur after the fifth postoperative day. Biliary fistula manifests as fever, pain in the right upper quadrant, and discharge of bilious liquid through the abdominal drains. Leukocytosis, increased canalicular enzyme levels, and eventual fluid collection that can be detected on ultrasound may occur. New surgical procedures are required for effective drainage of the fluid collection and detection of the fistula site. If the leak originates from the raw liver surface in cases of partial transplants, drainage of the fluid collection is sufficient. In cases of biliodigestive anastomotic dehiscence, a new anastomosis with adequate drainage should be performed.
In late fistulas of the raw surface and fistulas that are difficult to close, the possibility of stenosis of the biliodigestive anastomosis must be considered. Stenosis can also manifest as increased canalicular enzyme levels; in this case, a liver biopsy reveals canalicular biliary proliferation (Figure4).
Most stenoses can be treated with dilation by percutaneous transhepatic cholangiography, wherein a bile drain is placed to shape the anastomosis for approximately six months. When percutaneous treatment is not possible, a new surgery is indicated.
ImmunosuppressionImmediately after graft reperfusion, 20 mg/kg of methylprednisolone is administered; on the following day, 5 mg/kg is divided into four doses. Thereafter, the dose is decreased on a daily basis to 5 mg and is replaced by 5 mg of prednisone (or a half dose in young children), which is maintained for at least one year.
In addition to the corticosteroid, the immunosuppressive drug of choice is currently tacrolimus (FK 506), a calcineurin inhibitor that inhibits the action of interleukin-2, which activates T lymphocytes, a central component in transplant rejection. Tacrolimus is a potentially nephrotoxic drug and can cause vomiting, central nervous system disorders, and hypertension when administered at very high levels. In cases of late renal injury caused by calcineurin inhibitors, the doses of these immunosuppressant agents may be reduced by combining them with other drugs with similar effects and less renal toxicity, such as mycophenolate and sirolimus (10).
Hematological careIntra-abdominal bleeding may occur in the first few days after surgery; thus, periodic monitoring of the serum hemoglobin level and abdominal drain output is important. The intensity of bleeding is usually greater in reduced-size liver transplants due to the presence of the raw surface of the graft.
A relatively common scenario known as retained clot syndrome occurs during the early postoperative period. After the initial gradual improvement in coagulation, platelet count, and decreased blood drainage, there is a significant increase in intracavitary bleeding, thrombocytopenia, and coagulopathy, which do not revert despite the administration of blood products. With the improvement of liver function, the collected blood in the abdominal cavity forms large clots due to slow and diffuse hemorrhaging. These clots are responsible for the local consumption of platelets and coagulation factors, thus perpetuating the bleeding. Laparotomy is therefore necessary to clean the cavity and remove the clots, with possible hemostasis of some of the active bleeding.
INFECTIOUS DISEASESInfectious diseases are very common because patients are generally in a very compromised condition, may be malnourished, are likely to have multiple points of entry for microorganisms (e.g., incisions, catheters, probes), and are commonly using immunosuppressive drugs.
In the first weeks after transplantation, bacteria are the main infectious agents, the most common of which include enterococci and gram-negative bacteria in the abdomen. Thus, many centers prophylactically use a combination of ampicillin and cefotaxime in the perioperative period. Signs of infection in children who have undergone transplantation can vary from laboratory abnormalities without clinical symptoms (such as leukocytosis or leukopenia; hyponatremia; and elevated serum, liver, and urea enzymes) to irreversible fulminant septic shock. The presence of fever may indicate culture collection and investigation of the focus of infection, and it is important to immediately administer either specific or broad-spectrum antibiotics, depending on whether the agent can be identified.
Fungal infections are also relatively frequent, with Candida albicans being the most common infectious agent. Risk factors are prolonged antibiotic therapy, the presence of vascular complications, intestinal perforations, the need for endotracheal reintubation, steroid therapy, and retransplantation. Disseminated disease is the most common presentation. Thus, fluconazole may be prophylactically administered during the first weeks after transplantation.
Viral infections usually occur during the first month, with Cytomegalovirus being the most common infectious agent.
REJECTIONAcute cellular rejection is very common and can occur in 70% of cases (7). The peak incidence occurs between the fifth and tenth postoperative day and can manifest with nonspecific symptoms such as mild fever and abdominal pain. There is a predominant increase in canalicular enzymes (e.g., GGT) because the inflammatory process occurs through a lymphocytic infiltrate in the portal space with duct and endothelial insult of the portal branches. Hepatocytes are destroyed only in severe cases. The diagnosis must be confirmed by biopsy. After confirmation, treatment is introduced, which consists of pulse corticosteroids (methylprednisolone 20 mg/kg once a day for three days) and adjustment of the immunosuppressive drugs, with resolution occurring in most cases.
Chronic rejection usually appears after the first month of transplantation, presenting as progressive jaundice and itching, sometimes accompanied by acholic stools. Canalicular enzyme levels are increased, and diagnosis is confirmed by a liver biopsy showing the disappearance of bile ducts in the portal space. The prognosis is poor, and treatment consists of increasing levels of immunosuppressants and eventual retransplantation.
RELAPSE OF PRIMARY DISEASEIn autoimmune diseases, such as autoimmune hepatitis and primary sclerosing cholangitis, relapse may occur in the graft, and maintenance with higher levels of corticosteroids is required to prevent this process from occurring.
In cases in which adequate prophylaxis is not administered, viral hepatitis B and C recur with great frequency in the transplanted liver. For hepatitis B virus, anti-HBV immunoglobulin and nucleoside analogues (lamivudine) may be administered. Interferon and ribavirin may be used to prevent the recurrence of hepatitis C virus.
AUTHOR CONTRIBUTIONSTannuri U performed the liver transplant surgery and wrote the manuscript. Tannuri AC performed the liver transplant surgery and revised the manuscript.
No potential conflict of interest was reported.