Objective parameters in computed tomography (CT) scans that could predict calyceal access during percutaneous nephrolithotomy have not been evaluated. These parameters could improve access planning for percutaneous nephrolithotomy. We aimed to determine which parameters extracted from a preoperative multiplanar reconstructed CT could predict renal calyceal access during a percutaneous nephrolithotomy.
METHODSFrom January 2009 through April 2011, 230 patients underwent 284 percutaneous nephrolithotomies at our institution. Sixteen patients presented with complete staghorn calculi, and 11 patients (13 renal units) were analyzed. Five parameters were extracted from a preoperative reconstructed CT and compared with the surgical results of percutaneous nephrolithotomy.
RESULTSFifty-eight calyces were studied, with an average of 4.4 calyces per procedure. A rigid nephroscope was used to access a particular calyx, and a univariate analysis showed that the entrance calyx had a smaller length (2.7 vs. 3.98 cm, p = 0.018). The particular calyx to be accessed should have a smaller length (2.22 vs. 3.19 cm, p = 0.012), larger angles (117.6 vs. 67.96, p<0.001) and larger infundibula (0.86 vs. 0.61 cm, p = 0.002). In the multivariate analysis, the only independent predictive factor for accessing a particular calyx was the angle between the entrance calyx and the calyx to be reached (OR 1.15, 95% confidence interval [CI], 1.053–1.256, p = 0.002).
CONCLUSIONThe angle between calyces obtained by multiplanar CT reconstruction is the only predictor of calyx access.
Percutaneous nephrolithotomy (PCNL) is the first-line treatment for managing staghorn calculi, and it is associated with stone-free rates of 74%-83% (1). This technique has a lower morbidity compared to open surgery; however, with increasing stone size, a longer operative time and multiple tracts to achieve stone clearance may be required (2,3). In complex cases, a thorough radiologic study is essential for achieving optimal results and provides the surgeon with the information necessary for preoperative planning and appropriate percutaneous access (4). Computed tomography (CT) has proven to be a cornerstone of the radiologic evaluation of renal calculi and has emerged as the first-line tool for preoperative study and follow-up (5,6).
The CT scan is the gold standard exam for diagnosing urinary calculi (7). It shows the stone burdens and branches, the anatomy of the pyelocalyceal system, the kidney position and its relation to other abdominal structures (4). For patients with ectopic kidneys or fusion abnormalities, the CT scan is also mandatory before surgery because of aberrant vasculature and the incidence of retrorenal colon (8,9). Furthermore, the 3D reconstructive technique of CT scans is less dependent on the observer compared to other radiologic studies. This technique facilitates PCNL planning, can change the access position for surgery and improves the results in selected patients (5,6,10).
The objective parameters in the CT scan that can predict the access to a particular calyx during PCNL have never been evaluated. These parameters could improve access planning during the PCNL for staghorn stones, thereby decreasing the number of punctures needed while maximizing stone clearance.
In this study, we analyzed five parameters that can be extracted by a preoperative multiplanar reconstructed CT and compared these with the surgical results of PCNL for staghorn calculi. The objective was to define which parameters could predict renal navigation and calyceal access. Those parameters could be further used for planning PCNL for staghorn calculi.
MATERIALS AND METHODSFrom January 2009 through April 2011, 230 patients underwent a total of 284 PCNL at a single high-volume University hospital. Sixteen of these 230 (7%) patients were diagnosed with complete staghorn calculi.
All the patients with complete staghorn calculi that had a preoperative 64 channels multidetector CT and underwent a PCNL at our institution during the study period were included. Patients who had multiple accesses, Y punctures or had the post-operative CT after the nephrostomy tube was removed were excluded from the study. We also excluded patients whose procedures finished early because of bleeding and patients whose procedures used the flexible nephroscope for fragmentation or removal of any stone. After applying the eligible criteria and obtaining the local ethics committee approval, 11 patients were evaluable for the study.
Five parameters were analyzed by comparing the CT scan acquired at least one month before the surgery and another CT acquired before removing the nephrostomy tube on postoperative days 1 or 2. The CT immediately after the procedure was necessary to determine precisely which calyces were not accessed during the procedure, which was defined as the calyces in which the calculi were unchanged in the postoperative CT. The entrance calyx was determined by the presence of the nephrostomy tube, which was similar to the angle used for access.
Surgical TechniqueThe procedures were performed with the patient under general anesthesia. A pyelography was obtained with a 6 Fr ureteral catheter placed at the renal pelvis through cystoscopy. The bladder was drained with a 16 Fr Foley catheter. The calyceal access was achieved under fluoroscopic guidance using an 18-gauge needle and a Teflon curved 0.035” guide wire. The tract dilatation was accomplished with Amplatz dilators of up to 30 Fr. The fragmentation and stone removal were accomplished in all patients using Swiss LithoClast® (Electro Medical Systems S.A., Nyon, Switzerland) and rigid retrieval graspers through a rigid 26 Fr nephroscope. The surgery was completed when no residual calculi could be identified through nephroscopy or fluoroscopy or the residual calculi were not accessible through the same access and another access would overly increase the surgical time or bleeding. The flexible nephroscope was either not available for use, or no calculi were fragmented or removed with it. After completion, an 18 Fr Foley catheter was inserted as a nephrostomy tube, and the proper position was immediately confirmed with a contrast injection. A CT scan without contrast was performed on the first or second postoperative day. If no extra procedure was necessary, the nephrostomy tube was closed, and the bladder and ureteral catheter were removed. The nephrostomy tube was removed the next day (11).
CT techniqueThe patients underwent pre- and post-operative supine unenhanced examinations using a 64 channel multidetector CT (Discovery CT 750 HD General Electric [GE]), 64 channels). The multiplanar reconstruction (MPR) was completed using the Macintosh® version of OsiriX® V 3.3.2 32-bit, 2-Dimension MPR.
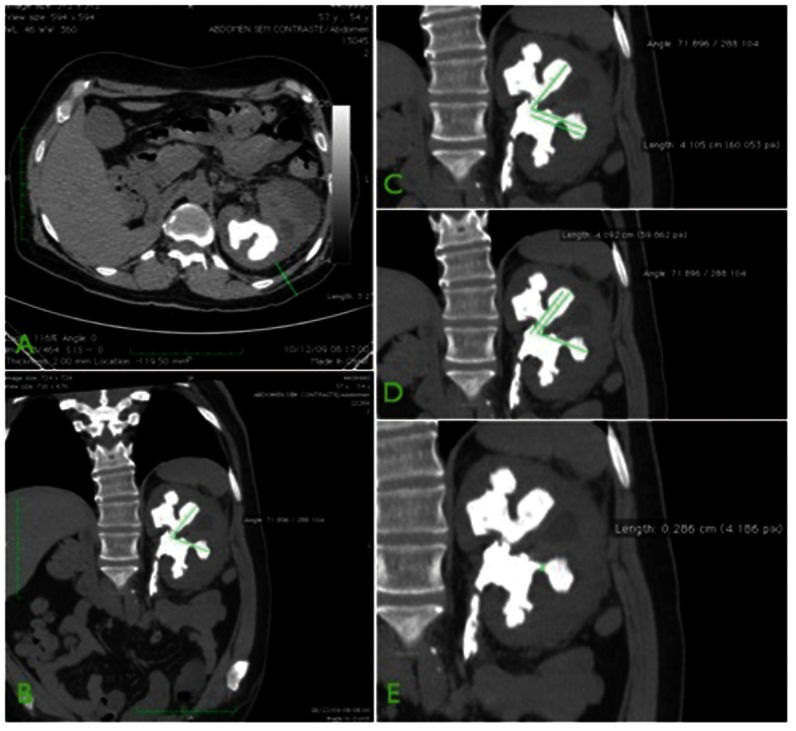
Parameters analyzedFive parameters were studied: 1) the distance between the skin and the kidney measured at the point of and with the surgical access angle (distance A, Figure 1A; 2) the angle formed by two straight lines starting at the middle of the calyces and passing tangentially through the infundibulum (Figure 1B; 3) the length of the calyx entrance, as determined by the distance of the line starting at the middle of the calyx entrance and ending at the previously described angle (distance X, Figure 1C; 4) the length of the particular calyx, as determined by the distance between the line starting at the angle and ending at the middle of the targeted calyx (distance Y, Figure 1D; and 5) the width of the calyx infundibulum to be reached, measured at the wider area (distance I, Figure 1E. Parameters 2, 3 and 4 were extracted to achieve a plane that included the studied calyces and the connection between them by the renal pelvis through the MPR.
Statistical AnalysisThe continuous parametric variables were reported as the mean value plus the standard deviation (SD). The continuous non-parametric variables were presented as the median values and interquartile range (IQR). A t-test was used to test the differences between averages when the variables were continuous and had a normal distribution. When the distribution was not normal, the Mann-Whitney U-test was used. A logistic regression was then used to analyze the independent predictive factors for calyceal access during PCNL. The independent variables entered into the regression model were distance X, distance Y, the angle between the calyces and the infundibular width. All statistical analysis was performed using SAS 9.1 software (Cary, NC) for Windows, and a p-value of <0.05 was considered statistically significant.
RESULTSEleven patients with complete staghorn stones in 13 renal units underwent 13 PCNL (two patients had bilateral complete staghorn stones). The median age was 38 years (range 13 to 61 years), and 60% of the patients were males. Most of the patients had comorbidities. The most frequent comorbidity was high blood pressure (40%) and obesity (30%). Three patients had no comorbidities; one was born with a bladder exstrophy and underwent an enterocystoplasty, one had diabetes and one had a history of pyeloplasty at childhood. The median Charlson index was 0 (0 to 3).
The inferior calyx was most frequently used for access (46.6% of the surgeries). The superior and middle calyces were each used for access in 26.6% of cases. Thirteen procedures were performed with the patient in a ventral decubitus position. Two patients had a modified Valdivia Uria access to the kidney (12). The average operative time was 240.6 minutes (range 180 to 300 minutes). Two patients received blood transfusions after the procedure, and one patient developed a pleural effusion, which was treated with drainage. Six patients required secondary procedures for stone clearance: five had one procedure, and one had two procedures. The most frequent procedure was extracorporeal lithotripsy (5), followed by flexible ureterolithotripsy (2).
Fifty-eight different calyces were studied with an average of 4.4 calyces (range 3 to 7) per procedure. Thirty calyces were considered as accessed and 28 as non-accessed.
In the univariate analysis, the accessed calyces had a smaller distance X (2.73 vs. 3.98 cm, p = 0.018), smaller distance Y (2.22 vs. 3.19 cm, p = 0.012), larger angles (117.6 vs. 67.96, p<0.001) and larger infundibula (0.86 vs. 0.61 cm, p = 0.002). There was no difference in distance A between the accessed and non-accessed calyces (Table 1).
Univariate analysis.
| Accessed Calyces | Non-Accessed Calyces | p-value | |
|---|---|---|---|
| Distance A (median – ICQ) | 4.93 (2.90-5.12) | 4.93 (2.90-5.57) | 0.737 |
| Distance X (median – ICQ) | 2.73 (1.80-4.6) | 3.98 (3.61-4.91) | 0.018 |
| Distance Y (median – ICQ) | 2.22 (1.28-3.27) | 3.19 (2.39-4.04) | 0.012 |
| Angle (mean±SD) | 117.6±20.81 | 67.96±20.00 | 0.001 |
| Infundibula (mean±SD) | 0.86±0.27 | 0.61±0.32 | 0.002 |
In the multivariate analysis, the only independent predictive factor for calyceal access was the angle between the calyces (OR 1.15, 95% CI 1.053 – 1.256, p = 0.002) (Table 2). For angles larger than 95°, 96.3% of the calyces were accessed with the rigid nephroscope compared to 12.9% when the angle was smaller than 95°. No calyx could be accessed when the angle was smaller than 75°. For angles between 75° to 95°, only 33.3% of the calyces were accessed (Table 3).
The spiral CT was first introduced into clinical practice in the late 1980s (13), and since then, it has revolutionized the radiologic evaluation of the urinary tract, becoming the gold standard exam for diagnosing urinary calculi (14,15). Recently, the CT has been used not only for diagnostic matters but also for obtaining detailed images of the calculi and its branches, 3D images of the collecting system anatomy, the relationship between the kidney and other abdominal structures and the density of the calculi (4,16). This imaging helps with planning the procedure to minimize morbidity and optimize results (17,18).
Flexible nephroscopy is part of the contemporary PCNL to reduce residual fragments and to reduce the number of renal access. A large volume stone in a particular calyx is difficult to manage with flexible nephroscopy because of limited irrigation. Therefore, PCNL of a complete staghorn stone frequently requires multiple renal accesses to reach a stone-free status, regardless of whether flexible nephroscopy is used. Some high-volume centers worldwide do not have flexible nephroscopes for all PCNLs. In this scenario, it is important to determinate the limits of renal access for reaching a particular calyx using a rigid nephroscope.
It is well known that increasing the stone-surface area can decrease the overall stone-free rate and increase the complication rate, operative time, and need for secondary-procedures and multiple tracts. The same philosophy can be attributed to complex renal stones with large calyceal components (19). In a study of 179 patients who were evaluated by CT and underwent PCNL, Gücük et al. (20) showed that the Hounsfield unit (HU) size and position of the calculi are independent predictors for the failure of the procedure. Having an HU value <677.5 increased the likelihood of procedure failure by 2.65 times, whereas stones with a staghorn morphology increased failure by 5.68 times. There was a positive correlation between a hematocrit decrease and a decrease in HU values (p<0.05).
Mishra et al. (21) studied 94 renal units with staghorn calculi with CT reconstruction. They found that a large total stone volume, a low pelvic and entry calyx stone volume and a large unfavorable calyx stone volume/percentile volume were independent factors associated with a greater risk for requiring multiple stone clearance surgeries. In this study, an unfavorable calyx was defined as having acute angles and infundibula width <8 mm. This definition was arbitrary and based on medical experiences.
Barcellos Sampaio et al. (22) studied the renal collecting system anatomy and concluded that knowledge of it is essential for urologists during operations on the collecting system. It is hypothesized that acute angle and narrow infundibula are associated with difficulties in accessing calyces and with stone clearance. However, this is the first study to compare these parameters with the likelihood of accessing the calyces. In the multivariate analysis, the angle was the only parameter related to the likelihood of accessing the calyx. All other parameters were found to be confounding factors. We found that no calyx can be accessed if the angle between the entrance calyx and the intended calyx is <75°. It is easy to predict the ability to access a particular calyx through a given access and plan preoperatively the need for multiple tracts.
Our analysis is restricted to complete staghorn calculi, but it can potentially be expanded to multiple calculi in different calyces with the aid of CT urography. More studies examining CT urography are necessary to determine whether the calyx angle can be used to predict calyceal access in patients without staghorn calculi.
Our study demonstrated that the angle between the calyces obtained by a 3D multiplanar CT reconstruction is the only predictor of calyx access. This procedure is simple and can be performed with a common computer without special training.
AUTHOR CONTRIBUTIONSGuglielmetti G participated in the drafting of the manuscript and data acquisition. Danilovic A participated in the study conception and design. Torricelli FC participated in the drafting of the manuscript. Coelho RF participated in the data analysis and interpretation. Mazzucchi E contributed to the critical revision of the manuscript. Srougi M supervised the study.
No potential conflict of interest was reported.