In obsessive-compulsive disorder, early treatment discontinuation can hamper the effectiveness of first-line treatments.
OBJECTIVE:This study aimed to investigate the clinical correlates of early treatment discontinuation among obsessive-compulsive disorder patients.
METHODS:A group of patients who stopped taking selective serotonin reuptake inhibitors (SSRIs) or stopped participating in cognitive behavioral therapy before completion of the first twelve weeks (total n = 41; n = 16 for cognitive behavioral therapy and n = 25 for SSRIs) were compared with a paired sample of compliant patients (n = 41). Demographic and clinical characteristics were obtained at baseline using structured clinical interviews. Chi-square and Mann-Whitney tests were used when indicated. Variables presenting a p value <0.15 for the difference between groups were selected for inclusion in a logistic regression analysis that used an interaction model with treatment dropout as the response variable.
RESULTS:Agoraphobia was only present in one (2.4%) patient who completed the twelve-week therapy, whereas it was present in six (15.0%) patients who dropped out (p = 0.044). Social phobia was present in eight (19.5%) patients who completed the twelve-week therapy and eighteen (45%) patients who dropped out (p = 0.014). Generalized anxiety disorder was present in eight (19.5%) patients who completed the twelve-week therapy and twenty (50%) dropouts (p = 0.004), and somatization disorder was not present in any of the patients who completed the twelve-week therapy; however, it was present in six (15%) dropouts (p = 0.010). According to the logistic regression model, treatment modality (p = 0.05), agoraphobia, the Brown Assessment of Beliefs Scale scores (p = 0.03) and the Beck Anxiety Inventory (p = 0.02) scores were significantly associated with the probability of treatment discontinuation irrespective of interactions with other variables.
DISCUSSION AND CONCLUSION:Early treatment discontinuation is a common phenomenon in obsessive-compulsive disorder patients from our therapeutic setting. Psychiatric comorbidities were associated with discontinuation rates of specific treatments. Future studies might use this information to improve management for increased compliance and treatment effectiveness.
For the majority of obsessive-compulsive disorder (OCD) patients enrolled in controlled clinical trials, the use of selective serotonin reuptake inhibitors (SSRIs) or cognitive behavioral therapy (CBT) results in treatment success.1 The treatment success reported in controlled trials, however, may not be generalizable to clinical practice because of low treatment availability, high disease heterogeneity and low completion rates.2–4
A recent practical clinical trial for OCD showed completion rates for pharmacological and psychotherapeutic interventions that were much lower than those reported in previous controlled trials. Low completion rates were due to early treatment discontinuation (before twelve weeks of treatment) and were associated with low response rates.5
Reasons for treatment discontinuation can be intrinsic (related to the patient), or extrinsic (related to social conditions and treatment characteristics, e.g., medication side effects). Intrinsic factors can include psychiatric comorbidities,6 symptom characteristics,7 disease severity,8 and personality traits.9 Understanding the reasons for early treatment interruption is essential for the delineation of more effective therapeutic strategies. In addition, the factors associated with the discontinuation of psychotherapeutic treatment might be different from those associated with the discontinuation of pharmacological treatment. Therefore, clarifying which factors are associated with noncompliance could help clinicians recognize and prescribe the treatment option that provides the greatest chance of compliance in a given patient.
Using a recently completed clinical trial as a test case, the objective of the present study was to determine whether there are clinical characteristics (with an emphasis on psychiatric comorbidities) associated with the early interruption of pharmacological or psychotherapeutic treatment.5
MATERIALS AND METHODSThe present study was part of a larger treatment study conducted at an OCD outpatient clinic at the University of Sao Paulo School of Medicine - Hospital das Clínicas. We received local Institutional Review Board approval before inclusion of the first patient, and our methods followed the Code of Ethics of the World Medical Association (Declaration of Helsinki). Recruitment occurred between January 2006 and December 2007 with television advertisements, radio spots and newspaper announcements. A psychologist with extensive experience in OCD contacted the interested subjects to determine whether a diagnosis of OCD was likely. Initial selection criteria were patients with a probable diagnosis of OCD, who were not currently receiving appropriate treatment, but were seeking such treatment. Interested patients were scheduled for a psychiatric consultation during which eligible patients were invited to participate in the trial.
SubjectsThe inclusion criteria were a primary diagnosis of OCD according to the DSM-IV criteria and current symptoms causing significant distress (Yale-Brown Obsessive Compulsive Scale (YBOCS) > or = 16). Exclusion criteria included clinical or neurological disease that could be worsened by the drugs used in the treatment protocol, substance dependence, psychotic symptoms, risk for suicide, and pregnancy or intention to become pregnant.
Treatment discontinuation was defined as treatment interruption prior to the end of the twelve-week treatment period. Treatment interruption included the failure to initiate treatment after allocation was performed (patients who missed the first consultation/therapy session and were marked as “did not receive intervention” in figure 1), the failure to comply with scheduled visits, or the inability to tolerate medication side effects leading to an aversion to any psychopharmacological treatment alternative. Patients who were removed from the trial because of a clinical decision (e.g., perceived clinical risk) and patients who did not tolerate the SSRI that was initially prescribed but agreed to take another SSRI were not considered dropouts, but they were excluded from the analysis.
Group cognitive behavioral therapy (GCBT).- Group cognitive behavioral therapy (GCBT).
aReasons for exclusion were not having OCD as the primary diagnosis (n = 29), refusal to participate (n = 15), already receiving appropriate treatment (n = 7), Yale-Brown Obsessive-Compulsive Scale score lower than 16 (n = 10), suicide risk (n = 2), or refractory to multiple previous treatments (n = 2).
bSequential allocation methodology has been described elsewhere.10
cReasons for treatment discontinuation were failure to attend clinical consultations or therapy sessions (n = 35), intolerable side effects to more than one medication (n = 6), medication-induced hypomania (n = 2), suicide attempt (n = 1), development of paranoid symptoms regarding psychotherapy (n = 2), and severe alcohol abuse during treatment (n = 1).
dAnalysis included all patients who abandoned treatment after sequential allocation. Exclusions were due to noncompletion of clinical interviews before treatment abandonment (n = 19) and treatment interruption based on clinical risk rather than treatment abandonment (n = 6).
The dropout group was compared with a paired sample of patients who completed the twelve weeks of treatment (the completer group). Patients in the completer group were matched to those in the dropout group in terms of age, sex, first treatment assigned, and period of enrollment.
Figure 1 presents the flow chart.
Among the one hundred four patients allocated to receive an SSRI, nine did not report for the initial consultation, and thirty failed to complete the treatment. Only six patients allocated to receive an SSRI discontinued treatment due to side effects and did not tolerate a second SSRI; they were classified as dropouts. Six patients were excluded due to an interruption decision based on clinical risk, and eight were excluded for not having completed the baseline interviews before treatment discontinuation. Twenty-five of the patients who abandoned SSRI treatment had completed the baseline clinical interviews.
Among the eighty-three patients allocated to receive group CBT, eleven did not report for the initial consultation, and sixteen failed to complete treatment. Of the twenty-seven patients in the CBT group who dropped out, only sixteen had completed the baseline clinical interviews.
Therefore, the dropout group consisted of forty-one patients (twenty-five who abandoned SSRI treatment and sixteen who abandoned CBT).
After describing the study to the participants, we obtained written informed consents.
TreatmentPatients who agreed to participate were sequentially allocated to receive an SSRI or group CBT. We used a method of sequential allocation that was devised by Fossaluza et al.,10 which shares the objectives of previous minimization procedures.11 Briefly, this method minimizes the possibility of differences between groups in a clinical trial that evaluates treatment efficacy by controlling for possible confounders, such as initial Y-BOCS score, gender, age, and previous treatment history. The advantage of the sequential allocation method is that it provides a mechanism to balance samples between group treatments.
To simulate the experience of naturalistic clinical settings, patients allocated to receive an SSRI were preferentially treated with fluoxetine, which is the most frequently used SSRI in Brazilian psychiatric clinical settings, and medical appointments were scheduled every four weeks during the first year of the trial. Patients were allowed unlimited telephone access to a psychiatrist. The potential side effects and the delayed onset of therapeutic effects were explained in detail at the first consultation. Patients were instructed to increase their fluoxetine dosage by 20 mg per week for the first month until the maximum tolerated dosage or 80 mg/day was reached.
Intolerable side effects were managed by reducing the dosage and administering symptomatic medication. If side effects persisted at the subsequent consultation, a second SSRI (sertraline) was used (n = 6) in the place of fluoxetine.
A twelve-week group course using CBT was administered in weekly 2-h sessions with up to 10 patients per group. Additional information on the structured protocol employed can be found in the study conducted by Cordioli et al.12
Prior to treatment initiation, patients were evaluated using the following instruments:
Structured Clinical Interview for DSM-IV Axis I Disorders – patient edition,13Structured Clinical Interview for Impulsive Disorders adapted from DSM-IV criteria (available upon request)
The Yale-Brown Obsessive-Compulsive Scale14
The Dimensional Yale-Brown Obsessive-Compulsive Scale15
The Brown Assessment of Beliefs Scale (BABS)16
The Beck Anxiety Inventory (BAI)17
The Beck Depression Inventory (BDI)18
The Social Adjustment Scale (SAS).19
Interviews were performed by experienced clinical psychiatrists or psychologists who had junior interviewer in at least three training sessions involving videotaped interviews and five involving live interviews performed by the senior interviewer. After this training, each junior interviewer conducted five interviews under the supervision of the senior interviewer. If there was agreement between the junior and senior interviewer on most of the results, the new interviewer was allowed to conduct interviews without assistance.
Statistical analysisThe dropout and completer groups were compared using the chi-square test for categorical variables and the Mann-Whitney test for continuous variables. Variables with a p value < 0.15 with respect to the difference between groups in this initial analysis were included in a logistic regression analysis where dropping out was the response variable.
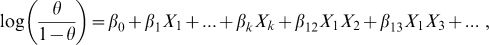
The logistic regression model was adjusted to estimate the chance of a specific patient abandoning treatment before completing the twelve weeks of the trial. We constructed the following formula, which considered the main effects and first-order interactions:
where θ is the chance that a patient will abandon treatment, Xi is the ith variable, β0 is the intercept, βi is the main effect of the ith variable, and βij is the interaction effect between the ith variable and the jth variable; i,j = 1,...,k, j goodness of fit of an estimated statistical model.Only current diagnoses were entered in the analysis.
RESULTSThe comparisons between groups regarding demographic characteristics, age at obsessive compulsive symptoms onset, duration of illness, and OCD symptoms content are shown in Table I.
Demographic and clinical characteristics.
| Characteristic* | Completers | Dropouts | p† |
|---|---|---|---|
| Males:Females, n (%):n (%) | 23 (56.1):18 (43.9) | 23 (56.1):18 (43.9) | NA |
| Age (years), mean (SD) | 33.8 (9.83) | 33 (10.74) | NA |
| First treatment assigned | |||
| SSRI, n (%) | 25 (61) | 25 (61) | NA |
| Group CBT, n (%) | 16 (39) | 16 (39) | NA |
| Marital status | 0.122 | ||
| Married, n (%) | 20 (48.8) | 11 (26.8) | |
| Divorced, n (%) | 3 (7.3) | 4 (9.8) | |
| Single, n (%) | 18 (43.9) | 26 (63.4) | |
| Socioeconomic level | 0.490 | ||
| Upper class, n (%) | 1 (2.4) | 3 (7.7) | |
| Middle class, n (%) | 35 (85.4) | 30 (76.9) | |
| Lower class, n (%) | 5 (12.2) | 6 (15.4) | |
| Employment status | 0.439 | ||
| Currently employed, n (%) | 25 (61) | 29 (70.7) | |
| Other**, n (%) | 16 (39) | 12 (29.3) | |
| Years of schooling, mean (SD) | 13.7 (3.63) | 13.3 (4.94) | 0.703 |
| Age at symptom onset (years), mean (SD) | 15.1 (8.89) | 12.3 (6.86) | 0.159 |
| Interval between symptom onset and first treatment received (years), mean (SD) | 16.0 (12.60) | 17.8 (11.85) | 0.549 |
| Duration of illness (years), mean (SD) | 18.7 (12.02) | 20.7 (11.46) | 0.444 |
| Symptoms, by dimension (DY-BOCS) | |||
| Aggression, n (%) | 26 (63.4) | 30 (73.2) | 0.342 |
| Sexual and religious, n (%) | 24 (58.5) | 25 (61.0) | 0.822 |
| Symmetry and ordering, n (%) | 37 (90.2) | 36 (87.8) | 0.724 |
| Contamination and cleaning, n (%) | 33 (80.5) | 30 (73.2) | 0.432 |
| Hoarding, n (%) | 19 (46.3) | 20 (48.8) | 0.825 |
| Miscellaneous, n (%) | 38 (92.7) | 39 (97.5) | 0.317 |
| Beck Depression Inventory score, mean (SD) | 17.4 (10.96) | 21.3 (12.19) | 0.147 |
| Beck Anxiety Inventory score, mean (SD) | 15.2 (9.94) | 20.6 (11.45) | 0.030 |
| Social Adjustment Scale score, mean (SD) | 2.3 (0.74) | 2.4 (0.66) | 0.197 |
| BABS score, mean (SD) | 4.2 (3.55) | 6.8 (6.04) | 0.074 |
| DY-BOCS Global Severity score, mean (SD) | 8.8 (1.34) | 8.7 (1.90) | 0.660 |
| DY-BOCS Global Impairment score, mean (SD) | 10.0 (3.10) | 10.2 (2.69) | 0.672 |
| Y-BOCS obsessions score, mean (SD) | 12.7 (2.93) | 12.4 (3.26) | 0.615 |
| Y-BOCS compulsions score, mean (SD) | 12.6 (2.67) | 12.6 (3.24) | 0.873 |
| Overall Y-BOCS score, mean (SD) | 25.3 (4.92) | 25.1 (6.00) | 0.874 |
Pearson's chi-square test was used for categorical variables, and the Mann-Whitney test was used for continuous variables.
Groups were paired according to sex, age, first treatment assigned and period of inclusion in the trial.
Includes unemployment, retirement, part-time studies and unwaged domestic work. Full-time students were considered currently employed.
SD: standard deviation; SSRI: selective serotonin reuptake inhibitor; CBT: cognitive behavioral therapy; BABS: Brown Assessment of Beliefs Scale; DY-BOCS: Dimensional Yale-Brown Obsessive-Compulsive Scale; Y-BOCS: Yale-Brown Obsessive-Compulsive Scale.
The groups did not differ in terms of sociodemographic characteristics or OCS content. Except for the higher severity of anxiety symptoms in the dropout group (measured with the BAI), there were no significant differences between groups for any of the measures of symptom severity. Interestingly, there was a tendency for lower insight in the dropout group, which was measured by the BABS (p = 0.074).
Differences in Axis I psychiatric comorbidities between groups are shown in Table II.
Psychiatric comorbidities.
| Axis I Diagnosis (DSM-IV) | Completers n (%) | Dropouts n (%) | p† |
|---|---|---|---|
| Obsessive-compulsive spectrum disorders | 11 (26.8) | 14 (34.1) | 0.472 |
| Chronic tic disorders | 7 (17.1) | 9 (22.5) | 0.540 |
| Tourette syndrome | 1 (2.4) | 4 (10.0) | 0.157 |
| Body dysmorphic disorder | 5 (12.2) | 5 (12.5) | 0.967 |
| Trichotillomania | 1 (2.7) | 0 (0.0) | 0.308 |
| Mood Disorders | 19 (46.3) | 26 (63.4) | 0.120 |
| Major depressive disorder | 15 (36.6) | 20 (48.8) | 0.264 |
| Dysthymia | 4 (9.8) | 8 (19.5) | 0.211 |
| Bipolar type I | 2 (4.9) | 4 (9.8) | 0.396 |
| Bipolar type II | 1 (2.4) | 1 (2.4) | 1,000 |
| Anxiety Disorders | 22 (53.7) | 30 (73.2) | 0.067 |
| Panic disorder with agoraphobia | 0 (0.0) | 3 (7.5) | 0.074 |
| Panic disorder without agoraphobia | 1 (2.4) | 1 (2.5) | 0.986 |
| Agoraphobia | 1 (2.4) | 6 (15.0) | 0.044 |
| Social phobia | 8 (19.5) | 18 (45) | 0.014 |
| Specific phobia | 14 (34.1) | 15 (37.5) | 0.753 |
| Posttraumatic stress disorder | 3 (7.3) | 4 (10.0) | 0.667 |
| Generalized anxiety disorder | 8 (19.5) | 20 (50.0) | 0.004 |
| Somatoform disorders* | 8 (19.5) | 13 (31.7) | 0.206 |
| Somatization | 0 (0.0) | 6 (15.0) | 0.010 |
| Chronic pain disorder | 2 (4.9) | 3 (7.5) | 0.624 |
| Hypochondria | 0 (0.0) | 3 (7.5) | 0.074 |
| Conversion disorder | 1 (2.4) | 1 (2.5) | 0.986 |
| Eating disorders** | 4 (9.8) | 4 (9.8) | 1,000 |
| Impulse control disorders*** | 10 (24.4) | 7 (17.0) | 0.332 |
Includes body dysmorphic disorder, hypochondria, chronic pain disorder, conversion disorder and somatization, although body dysmorphic disorder results were shown under obsessive-compulsive spectrum disorders.
There were significant differences between the two groups in terms of agoraphobia, social phobia, generalized anxiety disorder (GAD), and somatization disorder. Indeed, all of these disorders were more common in the dropout group. No significant differences were found for other psychiatric disorders.
In the dropout group, there were six patients with a comorbid diagnosis of agoraphobia (two abandoned group CBT, and four terminated SSRI treatment), eighteen with social phobia (seven abandoned group CBT, and eleven terminated SSRI treatment), twenty with GAD (seven abandoned group CBT, and thirteen terminated SSRI treatment), and six with somatization disorder (one abandoned group CBT, and five terminated SSRI treatment). The mean BDI scores were 18.86 (SD = 13.74) and 22.75 (SD = 11.24) in the group CBT and SSRI dropouts, respectively, whereas the mean BAI scores were 19.86 (SD = 15.11) and 21.08 (SD = 9.02) in the group CBT and SSRI dropouts, respectively.
Many patients presented with multiple comorbidities. Five patients who abandoned group CBT and twelve who abandoned SSRI treatment had at least two comorbid psychiatric disorders that were associated with noncompliance.
Logistic regression model with interaction between variablesThe coefficients that were adjusted according to the logistic regression model are shown in Table III. The p value corresponds to the hypothesis testing H0: βi = 0. In other words, the hypothesis was that the ith variable does not modify the chance that a specific patient abandoned treatment. A p value < 0.05 was required to reject this hypothesis and indicate that a given variable modified the chance of treatment discontinuation by a specific patient. Positive and negative coefficients indicate that the corresponding variable increases or decreases the chance of treatment discontinuation, respectively, compared with the chance that the reference individual will do the same. The intercept represents the reference individual, which was a female who was allocated to pharmacological treatment, had no diagnosis of GAD or agoraphobia and had scores of 0 on the BAI, BDI and BABS.
Logistic regression model with interaction between variablesa.
| coefficient | Standard error | p-value | |
|---|---|---|---|
| Interceptb | −13.320 | 6.350 | 0.0359* |
| Group CBT | −78.427 | 39.637 | 0.0479* |
| Male gender | 11.439 | 6.537 | 0.0801** |
| BDI | 0.018 | 0.053 | 0.7346 |
| BAI | 1.257 | 0.572 | 0.0279* |
| BABS | −2.773 | 1.261 | 0.0279* |
| Agoraphobia | 81.540 | 6,254.101 | 0.9896 |
| GAD | 10.193 | 6.899 | 0.1395 |
| Group CBT:Male | 10.781 | 6.084 | 0.0764** |
| Group CBT:BDI | −2.344 | 1.111 | 0.0349* |
| Group CBT:BAI | 3.148 | 1.504 | 0.0364* |
| Group CBT:BABS | 8.106 | 4.038 | 0.0447* |
| Group CBT:GAD | 63.596 | 31.004 | 0.0402* |
| Male:BAI | −1.233 | 0.582 | 0.0339* |
| Male:BABS | 2.822 | 1.249 | 0.0238* |
| Male:GAD | 8.131 | 3.697 | 0.0278* |
| BAI:GAD | −1.222 | 0.583 | 0.0360* |
| BABS:Agoraphobia | −8.935 | 803.827 | 0.9911 |
| BABS:GAD | 3.014 | 1.283 | 0.0188* |
The results shown in Table III should be interpreted with caution because of the large number of interactions between variables. To clarify the impact that the values for each variable and the scores have on the probability of treatment discontinuation, an interactive model is available at the following site:
http://protoc.incubadora.fapesp.br/portal/art/spreadsheet.xls
To determine whether the model resulting from the logistic regression was suited to predict the chance of discontinuation, a cutoff point (0.4272) for the adjusted probabilities was chosen so that the adjusted proportion of dropouts in the model was the same as that presented in the sample. If this cutoff point distinguishes between groups with significantly different frequencies of treatment discontinuation, the model would be considered appropriate. Of the 76 patients in the final sample, 66 (86.8%) were classified correctly using the adopted cutoff point. Patients for whom the index was above the cutoff point had a much higher chance of abandoning treatment than those for whom the index was below the cutoff point.
To illustrate the interactions occurring in this model, we calculated the dropout probabilities for several hypothetical situations:
A woman with a current diagnosis of agoraphobia and scoring near zero on the BAI, BDI, and BABS would have a low probability of abandoning CBT (near 0%) and a high probability of abandoning pharmacological treatment (near 100%).
A man with a BDI score of 55 and a BAI score of 40 would have a much higher chance of abandoning pharmacological treatment (50%) than abandoning CBT (near 0%). If his insight was low (BABS = 12), however, the situation would be reversed: the probability of abandoning the pharmacological treatment (65%) would be lower than abandoning CBT (near 100%).
A woman with GAD and low insight (BABS = 10) would have a greater probability of abandoning CBT (near 100%) than pharmacological treatment (33%).
A man with significant depressive symptoms (BDI = 30) and low insight (BABS = 20) would rather abandon CBT (near 100%) than pharmacological treatment (42%).
DISCUSSIONMain findingsThe major finding of the present study was that anxiety disorders and somatization were associated with treatment discontinuation in OCD patients. Many patients presented with multiple comorbidities, which made it difficult to distinguish the individual impacts of a given comorbidity on noncompliance. Building a logistic regression model inclusive of interactions made it clear that complex interactions occurred between variables. Treatment type (pharmacological or psychotherapeutic) interacted with other variables to produce different probabilities of treatment discontinuation.
Very few trials have investigated the clinical correlates of treatment discontinuation in OCD patients, and no trial has specifically addressed the impact of comorbidities on completion rates. Therefore, we discussed our findings in the light of psychiatric disorders other than OCD. The relationship between the presence of anxiety disorders and adherence to treatment has been previously addressed20. Among anxious patients, social phobia has been implicated in treatment discontinuation. This observation led to the development of distance therapeutic techniques,21 which have also been developed for OCD treatment.22–23 In Food and Drug Administration trials6, GAD patients primarily abandoned treatment due to side effects rather than factors such as lack of treatment efficacy. This finding agreed with our results that GAD patients primarily abandoned treatment when allocated to pharmacological intervention. Interestingly, SSRIs (e.g., fluoxetine) can cause an initial worsening of anxiety symptoms during the initial phase of treatment, which might explain the lack of treatment compliance. We also observed that increasing the frequency of consultations in the initial phase of the pharmacological arm decreased the discontinuation rate. Therefore, reducing the time interval between initial consultations might have a positive influence on treatment compliance in highly anxious patients. Because there was a higher completion rate in the psychotherapeutic arm, it is also reasonable to hypothesize that highly anxious patients are better treated through early referrals for psychotherapy.
The present study indicates that noncompliance is an important issue in OCD treatment in our clinical setting; however, there are methods (e.g., psychotherapy and frequent consultations at the beginning of pharmacotherapy) to minimize compliance issues. Nevertheless, studies with different populations are needed to determine whether dropout rates are as high and as susceptible to pragmatic measures as they were in our setting.
Somatization disorder has been shown to be a common and chronic disorder associated with GAD, panic disorder, and agoraphobia24–25. Somatization disorder has also been associated with premature antidepressant treatment discontinuation in patients with functional gastrointestinal disorders or depression26–27. Like GAD, somatization disorder seems to increase the dropout rate associated with intolerable side effects27. In our sample, somatization disorder rarely appeared without the presence of an anxiety disorder. Therefore, we were unable to calculate the impact of somatization disorder on dropout rates independent of the diagnosis of a comorbid anxiety disorder. In addition, the frequency of treatment discontinuation due to side effects was low in our sample, which was in agreement with the findings of a previous study28. In addition to affecting noncompliance associated with anxiety disorders, somatization disorder may act as a marker of anxiety chronicity and severity. These speculations need to be tested in future studies.
We failed to replicate the previous findings from Mataix-cols et al.7 regarding the association between hoarding symptoms and poor treatment compliance. In the test case,5 hoarding was not associated with poor treatment response.
The present study had several limitations. Although there was an attempt to make our sample similar to a sample from a non-research environment, patients were sequentially allocated to the initial treatment (with an SSRI or group CBT) rather than choosing their initial treatment. This difference might have negatively affected the compliance rate. In future practical studies, other study designs should be considered to reduce treatment discontinuation as a consequence of dissatisfaction with the allocated intervention29. In addition, there was a subgroup of premature dropouts (i.e., patients who abandoned treatment before clinical evaluation) who were not represented in our sample. Furthermore, the small sample size made it difficult to draw any conclusions from the psychiatric comorbidities that were infrequent in our sample, such as eating disorders, bipolar mood disorder, and impulse control disorders. Results regarding group CBT should also be considered with caution because the dropout group only consisted of sixteen patients, and findings from the regression analysis were not evident in models that did not account for the interactions between variables.
CONCLUSIONIn conclusion, our results demonstrate that psychiatric comorbidity among OCD, other anxiety disorders, and somatization disorder are associated with dropout before the completion of twelve weeks of treatment. Therefore, future studies assessing measures to reduce treatment discontinuation among patients with anxiety disorders are needed to increase OCD treatment effectiveness.
In addition, our data suggest that treatment compliance and effectiveness in OCD can be optimized if the assigned treatment modality is tailored according to specific psychopathologic features. Furthermore, future studies should investigate additional strategies for treating OCD patients with comorbid conditions.
This study received financial support in the form of grants provided by the following Brazilian governmental agencies: the Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq, National Council for Scientific and Technological Development, Grant number: 0742/07, 521369/96-7 and 475919/2006-8) and the Fundação de Amparo à Pesquisa do Estado de São Paulo (FAPESP, Foundation for the Support of Research in the State of São Paulo, Grant number: 2005/55628-08 and 06/50273-0).
Disclosure of Conflicts of Interest: The first author is the principal investigator of an ongoing investigator initiative trial partially funded by Novartis. None of the other authors received any financial support from the pharmaceutical industry in the past 12 months.