Prolonged invasive mechanical ventilation and reintubation are associated with adverse outcomes and increased mortality. Daily screening to identify patients able to breathe without support is recommended to reduce the length of mechanical ventilation. Noninvasive positive-pressure ventilation has been proposed as a technique to shorten the time that patients remain on invasive ventilation.
METHODS:We conducted a before-and-after study to evaluate the efficacy of an intervention that combined daily screening with the use of noninvasive ventilation immediately after extubation in selected patients. The population consisted of patients who had been intubated for at least 2 days.
RESULTS:The baseline characteristics were similar between the groups. The intervention group had a lower length of invasive ventilation (6 [4;9] vs. 7 [4;11.5] days, p = 0.04) and total (invasive plus noninvasive) ventilator support (7 [4;11] vs. 9 [6;8], p = 0.01). Similar reintubation rates within 72 hours were observed for both groups. In addition, a lower ICU mortality was found in the intervention group (10.8% vs. 24.3%, p = 0.03), with a higher cumulative survival probability at 60 days (p = 0.05). Multivariate analysis showed that the intervention was an independent factor associated with survival (RR: 2.77; CI 1.14-6.65; p = 0.03), whereas the opposite was found for reintubation at 72 hours (RR: 0.27; CI 0.11-0.65; p = 0.01).
CONCLUSION:The intervention reduced the length of invasive ventilation and total ventilatory support without increasing the risk of reintubation and was identified as an independent factor associated with survival.
Patients on invasive mechanical ventilation (MV) who fail the first attempt at the spontaneous breathing test (SBT) are selected for weaning, which means a gradual reduction of ventilatory parameters until the patient is able to breathe without ventilatory support.1-4 The amount of time a patient spends weaning from mechanical ventilation has been estimated to be as long as 42% of the total duration of MV.5,6 Nevertheless, weaning practices have been revisited due to a recent increase in the use of noninvasive positive-pressure ventilation (NPPV) to avoid intubation or during weaning in patients with acute respiratory failure.7,8
Extubation delays are associated with clinical complications that can reduce patient survival and increase hospital costs.9-11 On the other hand, early extubation can result in reintubation, which carries the potential for additional harm and an associated higher risk of mortality.3,12,13 Patients who fail extubation frequently require more time on mechanical ventilation and prolonged hospital stays.14,15 The optimal rate of reintubation is unknown, but it has been estimated to range between 5% and 15% in non-neurological patients.5
To reduce the time on MV, gradual weaning has been replaced by support for early and abrupt extubation as soon the patient is able to breathe without ventilator support or can be noninvasively supported. This new proposal is based on the early identification of patients who are capable of breathing spontaneously, through daily screening with a spontaneous breathing test (SBT)5,11,16-18 and the use of NPPV. NPPV use has been investigated and recommended for three different strategies during weaning: first, to abbreviate MV by facilitating extubation; second, to treat respiratory failure after extubation; and, most recently, to prevent respiratory failure after extubation in selected patients.5,6,19-29
The aim of this study was to evaluate the effectiveness of a weaning protocol based on the recommendations of the American College of Chest Physicians (ACCP),5 combined with NPPV use immediately after extubation in selected patients, with the goal of shortening the length of MV without increasing the reintubation rate.
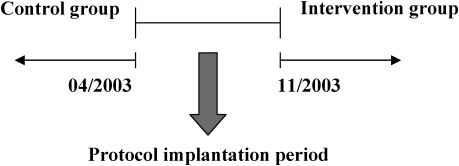
METHODSPatients and study designWe conducted a before-and-after study (Figure 1), which was designed before any data were collected. Consecutive adult patients admitted to a medical-surgical ICU (with 22 beds) in a tertiary hospital in São Paulo, Brazil and ventilated for more than 2 days were included. The data for both groups were collected prospectively after the inclusion criteria were met. Patients transferred from other hospitals, those with a tracheotomy and those with contraindications for using NPPV after extubation were excluded.28,29
Study design. Data collection period; the period between April and November 2003 was considered the time needed for protocol application. The controls are represented by a decreasing time line beginning in April 2003 and continuing until 74 consecutive patients had been enrolled. The intervention group is represented by an increasing time line beginning in November 2003 and continuing until 74 consecutive patients had been enrolled.
The study was approved by the hospital's ethics committee (CEPesq HSL2005/30), and informed consent was waived because the protocol was a standard procedure in the ICU at the time that the data were collected.
Control groupThe control group was composed of patients who met the inclusion and exclusion criteria listed above and were admitted to the ICU before the protocol was initiated. In this group, the decision to extubate was based on physicians' clinical judgment after the patient had been ventilated on pressure support (PSV) at 10 cm H2O above the 5 cm H2O of positive end-expiratory pressure (PEEP) for at least 2 hours. In most, but not all patients, an SBT with a T-piece was conducted before extubation. In the control group, NPPV was considered after extubation only in cases with postextubation respiratory failure despite conventional treatment.
Intervention groupIn the intervention group, extubation was based on the protocol orientations illustrated in Phases I through III of the algorithm (Figure 2). As noted, every morning, the respiratory therapists checked whether the patients had reached the initial protocol criteria and reported this information to the physician in charge, who was responsible for verifying the patient's hemodynamic status. If the patient was considered stable, sedation and diet were interrupted, and after 2 hours, a quick trial test at a PSV of 5 cm H2O above 5 cm H2O of PEEP was conducted to check whether the patient had a stable respiratory drive and was able to perform an SBT on a T-piece.6,3 The protocol was interrupted if any signs of intolerance occurred (i.e., respiratory rate≥ 35 min-1, SaO2≤ 90%, heart rate≥140 min-1 r a 20% change, systolic blood pressure ≥180 mm Hg or <90 mm Hg or increased anxiety, diaphoresis and respiratory workload signals). After a first fail, the patient was returned to PSV, and sedation was adjusted to fall within 3 or 4 on the Ramsay scale. The patient's diet was resumed, and the staff had 24 hours to determine and to address, if possible, the likely reason for weaning failure before subjecting the patient to a new trial on the following day (Figure 2).
Protocol design. IMV invasive mechanical ventilation; PEEP positive end-expiratory pressure; Hb hemoglobin; SBT spontaneous breathing trial; PSV pressure-support ventilation; MIP maximum inspiratory pressure; VT tidal volume; f/VT respiratory frequency to VT ratio; NPPV non-invasive positive-pressure ventilation.
Patients who passed the SBT using the T-piece were extubated (Figure 3). Patients with chronic obstructive respiratory disease (COPD) or congestive heart failure were given NPPV after extubation, based on the good results reported for noninvasive ventilatory support when these patients experience respiratory failure.6,21,22,28,29,32 Patients who had failed a previous SBT, had been reintubated, or had undergone MV for more than 4 days were also given NPPV after extubation because we believed that those patients were more susceptible to postextubation failure. NPPV was used for at least four hours after extubation. NPPV use was guided as follows: first, an interface was selected based on patient comfort and was fixed with gentle pressure, avoiding air leaks into the eyes. Nasal protection was used to prevent injury. Afterward, PEEP was selected with an initial value of 4 cm H2O, with progressive increments of 2 cm H2O until values reached 10 cm H2O. The FiO2 was initially set at 50% and reduced to 40% by 5% increments, with SaO2 kept above 92%. The level of inspiratory pressure above PEEP was initially set at 2 cm H2O and increased progressively by 2-cm-H2O steps, until the respiratory rate was ≤35 min-1, the tidal volume ≥5 mL/kg and f/VT <110 without signs of intolerance. After the initial 4 hours on NPPV, the patient was evaluated without noninvasive support to determine whether this support was still necessary. NPPV was used again only if the patient exhibited signs of ventilatory distress.
Data collection and definitionsThe protocol was implemented between April and November 2003. The control group consisted of 74 consecutive patients intubated prior to April 2003. The intervention group consisted of 74 consecutive patients who were intubated after November 2003. The time span between the first and the last consecutive patient in both groups was 11 months (Figure 1). The application of the protocol was the major change in ICU patient care during the study period. Sedation and analgesia practices were the same for the control and intervention groups. Patients who had been included in the control group were excluded from the intervention group in cases of subsequent ICU admissions. In both groups, only the data from the first intubation were considered when a second intubation occurred during the same admission.
All data were collected from protocol worksheets, medical records and the hospital electronic database and were stored in an electronic format (Microsoft Access®) elaborated for this study.
Statistical analysisThe sample size (74 patients per group) was calculated based on a previous pilot study that considered the number of patients necessary to reduce the MV period by a mean of 2 days, given a two-tailed Type I error of 5% and a power of 80%. SPSS version 13.0 (SPSS, Chicago, IL) was used for statistical analyses. Quantitative continuous variables were compared using the Mann-Whitney U test for non-normally distributed variables, with interquartile ranges (IQ) used to represent data dispersion. The means of normally distributed variables were compared using Student's t-test. Pearson's chi-squared test was used to compare categorical variables, and Kaplan-Meier survival curves were used to estimate the cumulative probability of remaining on ventilatory support and the probability of survival during the ICU stay. The groups' curves were compared using the log-rank test. Multivariate analysis with the Cox proportional hazards regression model was used to investigate the predictive role of significant variables in univariate analysis. Relative risks and 95% confidence intervals (CI) were computed for variables that were independently associated with survival. For all tests, the significance level was set at p≤ 0.05 (two-tailed).
RESULTSThe ventilators used for MV and NPPV were the same for both groups, as were the interfaces used for NPPV. A total of 148 patients were included in the analysis. The groups had similar demographic and clinical baseline characteristics, as summarized in Table 1. Among the patients in the intervention group, only three failed the SBT on the first attempt, but all of them succeeded in the next-day trial. In this group, 56 were deemed at risk for respiratory failure after extubation and were thus designated for NPPV after extubation. Of note, 10 of the 56 patients did not use NPPV as recommended because of their primary physician's initial refusal; however, all 10 of those patients developed postextubation respiratory failure and required NPPV. Of those patients, four failed and were reintubated within 72 hours, and one died in the ICU.
Clinical and demographic characteristics of the study patients.
| Characteristics | Control group | Intervention group | ρ value |
|---|---|---|---|
| Number of patients | 74 | 74 | |
| Age, years | 70 (59-83) | 72 (62-79) | 0.67† |
| Female, n (%) | 36 (48.6) | 42 (56.8) | 0.32‡ |
| SAPS II | 54.0 ±15.0 | 55.0 ± 12.8 | 0.66* |
| Cause of intubation, n (%) | 0.16‡ | ||
| Acute respiratory insufficiency | 50 (67.6) | 60 (81.1) | |
| COPD | 7 (9.4) | 4 (5.4) | |
| Coma | 17 (23.0) | 9 (12.2) | |
| Neuromuscular disease | 0 | 1 (1.4) | |
| Fluid balance before extubation, mL | 746.1 ± 2355.5 | 1061.1 ± 2434.4 | 0.42* |
| Axillary temperature, °C | 36.7 ± 0.5 | 36.6 ± 0.4 | 0.17* |
| Hb, g/dL | 10.5 ± 1.1 | 10.3 ± 1.3 | 0.72* |
| Vasoactive drugs, n (%) | 0.81‡ | ||
| None | 47 (63.5) | 40 (54) | |
| Noradrenaline | 12 (16.2) | 14 (18.9) | |
| Dopamine | 1 (1.4) | 1 (1.4) | |
| Dobutamine | 6 (8.1) | 7 (9.5) | |
| More than one | 8 (10.8) | 12 (12.6) |
ICU intensive care unit; Hb hemoglobin before extubation; SAPS II Simplified Acute Physiology Score at ICU admission; COPD chronic obstructive pulmonary disease.
Values are means ± standard deviation, medians (interquartile range) or numbers (%).
Table 2 shows the primary outcomes in both groups, including the numbers of days on MV, the duration of ventilatory support (MV plus NPPV) and the reintubation rate within 72 hours. Compared to patients in the control group, patients in the intervention group had a lower median (IQ) number of days on MV (7.0 [4.0-11.5] vs. 6.0 [4.0-9.0]; p = 0.04) and on ventilatory support (9.0 [6.0-8.0] vs. 7.0 [4.0-11.0]; p = 0.01). Patients in the intervention group had a lower probability of remaining on ventilatory support (p< 0.001; Figure 4). No difference was observed between the groups regarding the reintubation rate within 72 hours (13.5% vs. 9.5%; p = 0.44).
Primary outcomes.
| Variable | Control group (n = 74) | Intervention group (n = 74) | ρ value |
|---|---|---|---|
| Days on MV | 7 (4-11.5) | 6 (4-9) | 0.04* |
| Days on ventilatory support | 9 (6-8) | 7 (4-11) | 0.01* |
| Reintubation rate at 72 hours, n (%) | 10 (13.5) | 7 (9.5) | 0.44† |
MV invasive mechanical ventilation.
Values are medians (interquartile range) or number (%).
The secondary outcomes presented in Table 3 reflected a higher rate of postextubation NPPV use for the intervention group (45.9% vs. 75.7%; p<0.001). The reintubation rate included all reintubations during the ICU stay, and not just the reintubations that occurred within the first 72 hours. Reasons for reintubation were classified into six categories. Reintubation due to respiratory failure occurred in 78.9% of patients in the control group vs. 45% in the intervention group. The second major reason for reintubation was cardiorespiratory arrest in the control group (10.5%) and surgery in the intervention group (35%). Our data also suggested a longer time between extubation and reintubation in the control group, although this difference was not statistically significant. The cumulative ICU survival rate was higher in the intervention group (p = 0.05; see Figure 5).
Mortality, NPPV and reintubation rates.
| Variables | Control group (n = 74) | Intervention group (n = 74) | ρ value |
|---|---|---|---|
| Mortality rate in the ICU, n (%) | 18 (24.3) | 8 (10.8) | 0.03‡ |
| Postextubation NPPV rate, n (%) | 34 (45.9) | 56 (75.7) | <0.001‡ |
| Reintubation in the ICU, hours | 119.7 ± 133.7 | 53.2 ± 43.6 | 0.06* |
| Reason for reintubation in the ICU, n (%) | 19 (25.7) | 20 (27.0) | 0.08‡ |
| Upper airway obstruction | 0 | 0 | |
| Respiratory failure | 15 (78.9) | 9 (45.0) | |
| Congestive heart failure | 0 | 1 (5.0) | |
| Deteriorating mental status | 1 (5.3) | 3 (15.0) | |
| Surgery | 1 (5.3) | 7 (35.0) | |
| Cardiac and respiratory standstill | 2 (10.5) | 0 |
ICU intensive care unit; NPPV noninvasive positive-pressure ventilation.
Values are means ± standard deviation or numbers (percent).
A multivariate analysis using the Cox proportional hazards regression model (Table 4) identified the protocol an independent factor associated with ICU survival (p = 0.03), whereas the reintubation rate within 72 hours was an independent factor associated with ICU mortality (p = 0.01). When the demographic and baseline data from the control patients who used NPPV were compared to those from the intervention group, no differences were found (Table 5).
Multivariate analysis for survival using the Cox proportional hazards regression model.
| Variables | β | Standard error | RR | 95% CI | ρ value |
|---|---|---|---|---|---|
| Days on MV | -0.37 | 0.44 | 0.69 | 0.29-1.65 | 0.41 |
| Reintubation at 72 hours | 1.32 | 0.45 | 0.27 | 0.11-0.65 | 0.01 |
| Protocol | 1.01 | 0.45 | 2.75 | 1.14-6.65 | 0.03 |
| SAPS II | -0.02 | 0.43 | 0.98 | 0.43-2.22 | 0.97 |
ICU intensive care unit; CI confidence interval; SAPS II Simplified Acute Physiology Score at ICU admission; RR relative risk.
Clinical and demographic characteristics of the patients treated with NPPV postextubation.
| Variables | Control group (n = 34) | Intervention group (n = 56) | ρ value |
|---|---|---|---|
| Age, years | 76.5 (71-81) | 75 (66-81) | 0.16† |
| Female, n (%) | 19 (55.9) | 25 (44.6) | 0.30‡ |
| SAPS II | 55.8 ± 14.2 | 56.5 ± 12.8 | 0.81* |
| Cause of intubation, n (%) | 0.24‡ | ||
| Acute respiratory insufficiency | 22 (64.8) | 45 (80.4) | |
| COPD | 6 (17.6) | 4 (7.1) | |
| Coma | 6 (17.6) | 6 (10.7) | |
| Neuromuscular disease | 0 | 1 (1.8) | |
| Fluid balance before extubation, mL | 376.2 ± 2144.5 | 888.5 ± 2297.6 | 0.32* |
| Axillary temperature, C° | 36.7 ± 0.4 | 36.6 ± 0.4 | 0.46* |
| Hb, g/dL | 10.5 ± 1.3 | 10.2 ± 1.2 | 0.39* |
| Vasopressor drugs, n (%) | 0.73‡ | ||
| None | 18 (52.9) | 27 (48.2) | |
| Noradrenaline | 6 (17.7) | 12 (21.4) | |
| Dopamine | 1 (2.9) | 0 | |
| Dobutamine | 4 (11.8) | 7 (12.5) | |
| More than one | 5 (14.7) | 10 (17.9) |
ICU intensive care unit; Hb hemoglobin before extubation; SAPS II Simplified Acute Physiology Score at ICU admission; COPD Chronic obstructive pulmonary disease.
Values are means ± SD, medians (interquartile range) or numbers (percent).
The most important results of this study are that a protocol combining the ACCP guideline for discontinuing mechanical ventilation with NPPV use immediately after extubation in selected patients was able to shorten MV duration and decrease the probability of remaining on ventilatory support without increasing the reintubation rate within 72 hours. In concurrence with these findings, the protocol was found to be independently associated with ICU survival.
Currently, there are two different approaches to extubating patients after a period on MV. Some groups suggest a weaning protocol after SBT failure, with a gradual reduction of the ventilatory parameters until patients are able to breathe spontaneously.1-5 Other groups have more recently proposed using daily screening to identify patients who meet the clinical conditions for breathing spontaneously, independent of MV parameters.5,11,16-18 In addition, NPPV may be able to reduce the duration of MV and prevent or treat postextubation respiratory failure.
COPD patients require a longer period of time for extubation compared with other patients; however, they are also less likely to be reintubated because NPPV after extubation can be successfully used in these patients.19 Nava et al. used NPPV as a weaning technique for COPD patients in an attempt to shorten the MV duration. These authors showed that using NPPV after an SBT failure reduced the MV duration, ventilator-related complications and mortality when compared to traditional weaning with invasive PSV.21 Similar results were published by Girault et al.22 Moreover, Ferrer et al. reported improved survival when NPPV was used in patients who had failed the SBT three times.31
NPPV was subsequently proposed to treat patients who develop respiratory failure after extubation; however, Keenan et al.24 found no advantage when they compared this technique to the standard therapy. On the other hand, Esteban and coauthors reported a higher relative risk of mortality associated with the use of NPPV to treat postextubation respiratory failure.25 None of these studies reported a beneficial effect of decreasing the reintubation rate on ICU or hospital mortality.20 In an observational study, Schettino et al. reported that almost half of patients who underwent NPPV to treat postextubation respiratory failure were intubated, and the mortality rate among those patients was 31%.33
The other possible use of NPPV was after extubation in selected patients at risk for postextubation failure. Studies of this use of NPPV have suggested a reduction in the reintubation rate and in ICU mortality compared to traditional weaning practices.20 Nava et al. studied patients with hypercapnia, congestive heart failure, ineffective cough, excessive secretions, more than one failure of a weaning trial, comorbid conditions or upper airway obstruction. In these patients at high risk for postextubation failure, the use of NPPV for 8 hours immediately after extubation decreased the reintubation and mortality rates when compared to controls.26 Based on the same rationale, Ferrer et al. considered patients older than 65 years, those with cardiac failure as the initial cause of intubation, and those with Acute Physiology and Chronic Health Evaluation (APACHE-II) scores exceeding 12 points on the day of extubation as at risk for developing postextubation respiratory failure. These authors reported decreased postextubation failure and ICU mortality in the NPPV group but no difference in 90-day survival rates between the groups.27
Our weaning protocol was designed to combine the concept of MV discontinuation (vs. gradual weaning) with an active daily screening to determine whether patients were able to breathe spontaneously or with the use of NPPV immediately after extubation for selected patients believed to be at risk of postextubation failure. We defined cases at risk of postextubation failure as not only patients with COPD or congestive heart failure but also those with MV durations longer than 4 days and patients who had formerly failed extubation or an SBT.
The incidence of NPPV use in the intervention group, 56 cases (75.7%), was greater than we anticipated; however, the only patients who developed postextubation failure were the 10 previously mentioned, whose primary physician did not permit the use of NPPV until respiratory failure symptoms were evident. In contrast, all patients in the control group used NPPV because of postextubation respiratory failure. The authors were surprised that the patients who used NPPV before and after the protocol was put in place had similar characteristics (Table 5) because NPPV was used in the control group to treat postextubation respiratory failure, while in the intervention group, NPPV was applied to avoid postextubation respiratory distress. Although there was no significant difference, the time interval between extubation and reintubation was shorter in the intervention group than the control group (53.2 ± 43.6 vs. 119.7 ± 133.7 hours, ρ = 0.06), and we believe that this result may be related to the better outcome in the intervention group. The shorter duration of ventilatory support in the intervention group (6 vs. 9, ρ = 0.01) is an important outcome when one considers that NPPV was used more frequently in the intervention group than in the control group (75.7% vs. 45.9%, ρ<0.01).
The reintubation rate within 72 hours was in accordance with the accepted range described by ACCP guidelines5 and was similar in both groups, including coma patients. Respiratory failure was the main reason for reintubation during the ICU stay in both groups but was substantially less frequent in the intervention group (78.9% of the control group and 45% of the intervention group). We believe that it is important to describe the need for reintubation throughout the ICU stay, and not just within 72 hours, because increased NPPV use after extubation in recent years has delayed reintubation in patients who developed postextubation respiratory failure.29 It is also important to note that in the control group, 10.5% of the reintubations occurred immediately before a cardiorespiratory arrest. The time to reintubation in the intervention group was less than half of the value for the controls; this could be an important factor favoring survival, as suggested by other studies.13,18
The main limitation of our study was the use of a historical control group; however, we emphasize that the implementation of the protocol was the most important change that took place in the care of ventilated patients in our ICU during the study period. Furthermore, this study was not designed to evaluate mortality, but our results are promising because the protocol was found to be independently associated with ICU survival. Other studies – ideally, randomized trials – are needed to confirm this result, particularly the impact on mortality.
Our study provides evidence that combining a daily check of patients' clinical readiness for extubation with the use of NPPV immediately after extubation in selected patients reduces the duration of MV and total ventilatory support without increasing the reintubation rate.