Plasma D-dimer levels are directly related to the intra- and extra-vascular coagulation that occurs in acute and chronic lung damage in patients with community-acquired pneumonia (CAP).
OBJECTIVES:This study examines the relationship between the severity of community-acquired pneumonia and D-dimer levels. In addition, the study examines the correlations among community-acquired pneumonia, the radiological extent of the disease and mortality.
METHODS:The Pneumonia Severity Index was used to classify patients into five groups. Patients were treated at home or in the hospital according to the guidelines for community-acquired pneumonia. Blood samples were taken from the antecubital vein with an injector and placed into citrated tubes. After they were centrifuged, the samples were evaluated with the quantitative latex method.
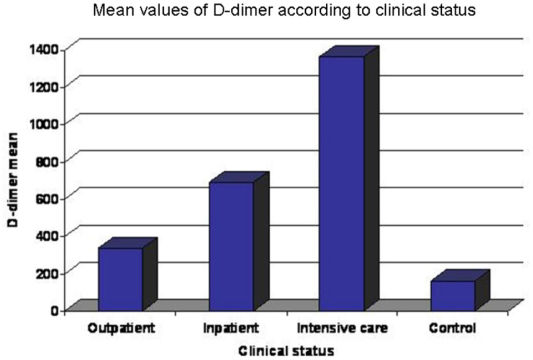
RESULTS:The study included 60 patients who had been diagnosed with community-acquired pneumonia (mean age 62.5 ± 11.7) and 24 healthy controls (mean age 59.63 ± 6.63). The average plasma D-dimer levels were 337.3 ± 195.1ng/mL in the outpatient treatment group, 691.0 ± 180.5 in the inpatient treatment group, 1363.2 ± 331.5 ng/mLin the intensive care treatment group and 161.3 ± 38.1ng/mL in the control group (p<0.001). The mean D-dimer plasma level was 776.1 ± 473.5ng/mL in patients with an accompanying disease and 494.2 ± 280.1 ng/mL in patients without an accompanying disease (p<0.05).
CONCLUSIONS:Plasma D-dimer levels were increased even in community-acquired pneumonia patients who did not have an accompanying disease that would normally cause such an increase.
Community-acquired pneumonia (CAP) is acquired during the course of everyday life by patients who do not have a known immune deficiency. Despite advancements in antibiotic treatment, CAP continues to negatively affect morbidity and mortality. CAP is also the sixth most common infectious cause of death in hospitals.1 Previous studies have shown that the mortality rate of pneumonia varies from 1% to 60% and is related to the weight of the patient.2 Studies have found that the mortality rate in CAP outpatient cases is 1–5%; the mortality rate is 12% in inpatient cases and 40% in intensive care patients.3,4
D-dimer (DD) is a metabolic substance produced during the catabolization of fibrin by plasmin. DD levels have been shown to increase in patients who have disorders that trigger fibrin production and catabolization; these disorders include pulmonary emboli (PE), deep vein thrombosis (DVT), solid tumors, leukemia, severe infections, trauma or a post-operative state, disseminated intravascular coagulation (DIC), pregnancy, acute stroke, sickle-cell anemia, congestive heart failure and chronic kidney failure.5–8 While the measurement of plasma DD levels is a well-known test for venous thromboemboli, the relationship between plasma DD and other diseases is still unclear. A limited number of studies have examined the relationship between CAP and plasma DD levels. Some of these studies suggest that an increase in DD is directly related to the intra- and extra-vascular coagulation that occurs in acute and chronic lung damage in CAP cases.9
The present study investigated the relationship between the severity of CAP and serum DD levels, as well as the potential correlation among plasma DD levels, the radiological extent of the disease and hospital mortality rates. The ultimate goal of this study was to determine whether plasma DD levels can be used to develop prognoses in CAP cases.
MATERIALS AND METHODSThis study began in October 2007–June 2008 at the Department of Chest Diseases, Faculty of Medicine, Cumhuriyet University, Sivas, Turkey, and included 60 consecutive CAP patients and 24 healthy controls. The study was approved by the ethics committee of the Faculty of Medicine, Cumhuriyet University, and all participants gave their informed consent. Individuals were excluded from the study because of cancer, leukemia, known blood-clotting and bleeding disorders, disseminated intravascular coagulation (DIC), renal failure, rheumatological diseases, vasculitis or sickle-cell anemia, pregnancy, an age less than 18 years or thromboembolic diseases. The demographic characteristics, physical examination findings and laboratory findings (leucocytes, hemoglobin, hematocrit, glucose, sodium, potassium, urea, creatinine, CRP and sedimentation) of all study participants were monitored regularly. Initial lung X-rays were taken for all patients in the CAP group and the control group. Patients were placed into two groups according to their lung X-rays: lobar (i.e., more than one segment of the same lobe involved) and multilobar (i.e., more than one lobe involved). Patients were divided into five groups according to the Pneumonia Severity Index (PSI) (PSI groups I, II, III, IV and V).10,11 CAP guidelines were used to determine whether patients would be treated at home or in the hospital.12 The criteria are shown in Table 1. The plasma DD levels of all participants were measured in the hospital’s hematology laboratory before starting the treatments of their CAP.
Hospital Admission Criteria in Patients with CAP.
| Patient Type | Criteria |
|---|---|
| Outpatients | Patients in PSI categories I and II |
| Outpatients (home treatment under observation) | Patients in PSI category III |
| Patients in PSI categories I and II with a comorbidity | |
| Inpatients (conventional hospitalization) | Patients in PSI categories IV and V |
| Patients in any PSI class who have significant pleural effusion | |
| Multilobar involvement | |
| Uncontrolled COPD (i.e., respiratory rate > 30 breaths/min or PO2 < 50 mm Hg) | |
| Acute respiratory failure (i.e., respiratory rate > 30 breaths/min or PO2 <60 mm Hg) | |
| Chronic renal failure (i.e., creatinine level > 2 mg/dL) | |
| Liver failure (child > 5 points) | |
| Alcohol abuse | |
| Lack of family support | |
| Psychosocial problems | |
| Uncontrolled coexisting disease | |
| Inpatients (ICU) | Respiratory failure requiring mechanical ventilation |
| Severe hypotension (systolic BP < 90 mm Hg) with oliguria | |
| Renal failure requiring dialysis | |
| Coma | |
| Septic complications | |
Blood samples taken from the antecubital vein with an injector were placed into 1.8 mL citrated tubes. The blood samples were centrifuged at 40,000 rpm for 15 minutes at room temperature and then evaluated using the quantitative latex method (ACLTOP, Italy). Plasma DD levels over 232 ng/mL were considered to be high. Statistical analyses were conducted with SPSS (version 14) for Windows. Kruskal-Wallis (CV), Tukey’s and Mann-Whitney U tests were used in the statistical analyses, and p-values of less than 0.05 were accepted as significant.
RESULTSThe study included 60 CAP patients with an overall mean age of 62.5 ± 11.7 years (29 males with an average age of 63.0 ± 11.7 years and 31 females with an average age of 62.0 ± 11.7 years) and 24 healthy controls with a mean age of 59.6 ± 6.6 years (10 males with an average age of 59.5 ± 4.6 years and 14 females with an average age of 59.4.0 ± 7.9 years). The age and sex distributions for the CAP and control groups are shown in Table 2.
The relationship between plasma DD levels and PSI was found to be statistically significant (p<0.05). Statistically significant differences (p<0.05) were found between the following groups: the control group and PSI groups III, IV and V; PSI group I and PSI group IV and V; PSI group III and PSI group V as well as between PSI group IV and PSI group V. Differences between the other groups were not found to be statistically significant (p>0.05) (Table 3).
Kruskal-Wallis (CV): 66.57, p<0.05. Statistically significant (p<0.05) differences were found between the following groups: the Control Group and PSI group III, IV and V; PSI group I and PSI group IV and V; PSI group II and PSI group IV and V; PSI group III and PSI group IV as well as between PSI group IV and PSI group V. No statistically significant differences were found among the other classes (p>0.05).
Plasma DD levels were 337 ± 195.1ng/mL in the outpatient group, 691.0 ± 180.5ngmL in the Inpatient Group, 1363.2 ± 331.5ng/mL in the Intensive Care Group and 161.3 ± 38.1ng/mL in the Control Group (see Table 4 and Figure 1).
In addition to CAP, 38 patients had other accompanying diseases (15 patients: asthma/COPD (Chronic obstructive pulmonary disease) 9 patients: diabetes mellitus; 8 patients: coronary artery disease; 3 patients: chronic liver disease and 3 patients: peptic ulcus); 22 patients had no accompanying disease. The mean plasma DD level for patients who had an accompanying disease was 776.15 ± 473.58, while the mean serum DD level for patients without an accompanying disease was 494.23 ± 280.18 ng/mL.
Patients were divided into two groups (lobar and multilobar), and plasma DD levels in the multilobar group were significantly higher than those in the lobar group (Table 5) (p<0.001)
Five of the 36 inpatients (13.8%) died; all of the deceased patients had plasma DD levels that were higher than the normal limit (1429.8 ± 511.3ng/mL), and all had another disease in addition to CAP.
DISCUSSIONAn increase in plasma DD levels may result from the activation of the fibrinolytic system and from fibrin catabolization within the alveoli. In addition, plasma DD levels may be increased by the activation of the blood coagulation process; this activation is caused by endotoxins in the Gram-negative pathogens that trigger CAP.12–15
This study found that the plasma DD levels of CAP outpatients, inpatients and intensive care patients correlated positively with the severity of their pneumonia. Plasma DD levels were also higher in CAP patients than in healthy controls.
The PSI is commonly used to evaluate disease severity in CAP patients. This study found a statistically significant relationship between patients’ PSI scores and their plasma DD levels. Shilon et al.,16 in a study performed on 68 CAP patients and no control group, found that PSI groups IV and V were associated with increased plasma DD levels when compared with groups I, II and III. Guneysel et al.17 studied 51 CAP patients and a healthy control group. They found mean DD levels of 2438.1 ± 2158.1 ng/mL in the Severe Pneumonia Group, 912.6 ± 512.6 ng/mL in the Non-severe Pneumonia Group and 387.94 ± 99.56 ng/mL in the Control Group; their results were statistically significant.17 Ribelles et al.18 found that increased plasma DD levels were correlated with PSI; their results were also statistically significant. Chalmers and coworkers19 also found that increased DD levels were correlated with PSI. In their study, median DD levels were as follows: Class I: 543 ng/mL; Class II: 727 ng/mL; Class III: 1192 ng/mL; Class IV: 1128 ng/mL and Class V: 1801 ng/mL; p<0.001.
The present study also found a statistically significant relationship between serum DD level and PSI score; these findings are consistent with the findings of previous studies.
Plasma DD levels were found to be statistically significant in the inpatient Group than outpatients group (defined according to the CAP guidelines).12 Guneysel et al. and Ribelles et al. found increased plasma DD levels in intensive care patients,17,18 and Shillon et al. found increased plasma DD levels in inpatients.16 The present study also found that plasma DD levels were significantly increased in intensive care patients.
Several studies have examined the relationship between plasma DD levels and the extent of disease in the lungs of CAP patients.18,20 Levi et al.20 reported a correlation between the extent of pulmonary disease, radiological appearance and plasma DD levels in severe pneumonia patients. Ribelles et al.18 suggested that plasma DD levels were higher in patients with lobar or multilobar pneumonia than in patients with segmental pneumonia. No relationship was detected between a high plasma DD level and either the radiological extent of the disease, microorganisms present or the antibiotics previously administered No segmental involvement was determined in the present study. This could be because patients came to our hospital only in the later stages of the illness or because they had received treatment previously in other healthcare settings. Patients were divided into two groups (lobar and multilobar), and plasma DD levels in the multilobar group were significantly higher than those in the lobar group (p<0.05).
Ribelles et al. found a strong correlation between the mortality rate and serum DD levels in CAP patients18. While the mean serum DD level was 3,786 ± 2,646 ng/mL in patients who died, it was only 1,609 ± 1,808 ng/mL in patients who survived (p <0.0001).18 They also determined that CAP patients in PSI classes IV and V who had plasma DD levels higher than 2000 ng/mL had a higher risk of mortality.18 Some researchers have suggested that increased plasma DD levels are related to the extent of pneumonia because the PSI and APACHE II score are closely associated with the mortality rate.21 Low plasma DD levels in CAP patients (less than 500 ng/mL) at the time of admission to the hospital has been linked to a decreased likelihood of an early death or major morbidity.19 Several researchers have identified meaningful relationships between plasma DD levels and PSI.16,17 However, because these studies included an insufficient number of patients, no strong relationship between plasma DD levels and mortality could be identified.16,17 The present study was able to identify a strong relationship between plasma DD levels and the rate of mortality (13.8%).
CONCLUSIONCAP patients show increased plasma DD levels even in the absence of an accompanying disease that can increase DD levels. Increased plasma DD levels in CAP patients were correlated with the severity of the disease, the radiological extent of the disease and in-hospital mortality rates. Additional studies with more patients are needed to determine whether plasma DD levels can be used to develop prognoses for cases of pneumonia.