We investigated the relationship between metabolic syndrome and breast arterial calcification detected via mammography in a cohort of postmenopausal subjects.
METHODS:Among 837 patients referred to our radiology department for mammographic screening, 310 postmenopausal females (105 patients with and 205 patients without breast arterial calcification) aged 40 to 73 (mean 55.9±8.4) years were included in this study. The groups were compared with respect to clinical characteristics and metabolic syndrome criteria. Univariate and multivariate analyses identified the factors related to breast arterial calcification.
RESULTS:Age, postmenopausal duration and the frequencies of diabetes mellitus, hypertension and metabolic syndrome were significantly higher in the subjects with breast arterial calcification than in those without (p<0.05). Multivariate analysis indicated that age (OR = 1.3, 95% CI = 1.1–1.6, p = 0.001) and metabolic syndrome (OR = 4.0, 95% CI = 1.5−10.4, p = 0.005) were independent predictors of breast arterial calcification detected via mammography. The independent predictors among the features of metabolic syndrome were low levels of high-density lipoproteins (OR = 8.1, 95% CI = 1.0−64.0, p = 0.047) and high blood pressure (OR = 8.7, 95% CI = 1.5−49.7, p = 0.014).
CONCLUSIONS:The likelihood of mammographic detection of breast arterial calcification increases with age and in the presence of hypertension or metabolic syndrome. For patients undergoing screening mammography who present with breast arterial calcification, the possibility of metabolic syndrome should be considered. These patients should be informed of their cardiovascular risk factors and counseled on appropriate lifestyle changes.
Metabolic syndrome (MS) is a constellation of interrelated cardiovascular risk factors, including insulin resistance or glucose intolerance, hypertension, atherogenic dyslipidemia and visceral obesity. Similarly, MS is associated with prothrombotic and proinflammatory conditions (1) as well as with an increased incidence of coronary artery disease (2). The prevalence of MS increases with age, particularly after menopause (3). Using the Adult Treatment Panel (ATP) III definition, Spila et al. have revealed an MS prevalence of 40% in women over the age of 45 (4).
Current clinical practice guidelines recommend that all women of 40 years and older should receive mammographic screening for the early detection of breast cancer (5). Breast arterial calcification (BAC) is commonly observed on screening mammography. The frequency of BAC increases with age and, according to previously published studies, varies from 1% to 49% (6). BAC is identified as medial calcific sclerosis of the small- to medium-sized muscular arteries in the breast and is occasionally reported as benign (7,8). Several studies have demonstrated relationships between BAC and coronary artery disease (9,10), hypertension (11), diabetes mellitus (DM) (11–14) and carotid intima thickening (15,16). One study has indicated an association between BAC and MS; however, no study in the literature has investigated a potential association between BAC and MS among postmenopausal women. Therefore, the objective of this study was to determine the relationship between BAC detected on mammography and MS in postmenopausal patients.
MATERIALS AND METHODSStudy population and designAmong 837 consecutive women who had been referred to our radiology department for screening mammography, 310 postmenopausal females aged 40–73 (mean 55.9±8.4) years were included in this prospective study, which was conducted between October 2011 and September 2013. This study was reviewed and approved by our institutional ethics committee. The investigator explained the research to and obtained informed consent from each participant.
The exclusion criteria included premenopausal status; prior breast surgery or the presence of trauma; coronary artery disease; and any history of malignancy, cerebrovascular diseases, or major systemic diseases such as renal insufficiency, liver disease, or connective tissue disease. Of the 310 selected patients, 105 were assigned to the BAC (+) group and 205 to the BAC (-) group. A questionnaire that addressed the patient's medical history, the number of infants she had delivered, the age of the patient and the duration of menopause was administered and a comprehensive physical examination was performed on each participant. The fasting blood glucose, total cholesterol, low-density lipoprotein (LDL) cholesterol, high-density lipoprotein (HDL) cholesterol and triglyceride levels, as well as the weight and waist circumference, were measured.
Mammography techniqueEach study participant underwent a full-field digital mammographic examination in the bilateral standard, mediolateral oblique and craniocaudal positions (Mammomat Inspiration, Siemens, Erlangen, Germany). The mammographic images were analyzed in accordance with the recommended breast-reporting guidelines of the American College of Radiology by an experienced radiologist (17). BAC was characterized by deposits of two parallel lines of calcium distributed along the periphery of the configuration of the tapered structures of the arteries, distinct from the breast ducts (Figure1).
Definition of MSThe National Cholesterol Education Program Adult Treatment Panel III (NCEP-ATPIII) (1) defines MS as follows: (i) a waist circumference of >102 cm for males and >88 cm for females; (ii) fasting serum triglycerides ≥150 mg/dL or drug treatment for elevated triglycerides; (iii) HDL cholesterol <40 mg/dL in males and <50 mg/dL in females or treatment with drugs for reduced HDL cholesterol; (iv) high blood pressure, i.e., diastolic blood pressure ≥85 mmHg, systolic blood pressure ≥130 mmHg, or treatment with drugs for hypertension; and (v) high glucose levels (fasting serum glucose ≥100 mg/dL or treatment with drugs for elevated glucose levels).
Baseline definitions and measurementsFor the purposes of this study, hypertension was defined by systolic blood pressure ≥140 mmHg, diastolic blood pressure ≥90 mmHg, or treatment with an antihypertensive drug (18). The diagnosis of DM was based on a fasting plasma glucose concentration of ≥126 mg/dL in two measurements or treatment with insulin or oral glucose-lowering agents. The BMI (kg/m2) was calculated by dividing each patient's weight (kg) by her height (m2). The waist circumference of each patient was measured from the midpoint of the line between the last rib and the crista iliaca, following exhalation and while the patient was in a standing position.
Statistical analysesThe statistical analyses were performed using version 12 of the Statistical Package for Social Sciences for Windows (SPSS Inc., Chicago, IL, USA). The continuous variables were reported as the mean±SD and the categorical variables were expressed as percentages. An independent Student's t-test for normally distributed data was used to compare each continuous variable between the two patient groups, whereas the categorical variables were compared using Fisher's exact test or the chi-squared test, as appropriate. Pearson's correlation coefficient was used to evaluate the correlations among all variables. Univariate and multivariate analyses were performed for the identification of the factors related to BAC. The statistical tests were all two-sided; a p-value of <0.05 was considered to be statistically significant.
RESULTSThe percentage of BAC (+) individuals among the women referred for mammographic screening was 16.6% (139 of 837 cases). Our study population included 105 patients in the BAC (+) group and 205 in the BAC (-) group. Table1 presents the clinical, hemodynamic and reproductive characteristics and laboratory parameters of each group.
The demographic factors, reproductive characteristics and laboratory parameters of the breast arterial calcification (+) and breast arterial calcification (−) groups.
| BAC (+) (n = 105) | BAC (-) (n = 205) | p-value | |
|---|---|---|---|
| Age (years) | 60.7±9.4 | 53.4±6.2 | <0.001 |
| Cigarette smoking (n, %) | 8 (7.6%) | 54 (26.3%) | 0.011 |
| Hypertension (n, %) | 45 (43%) | 48 (23%) | 0.016 |
| Diabetes mellitus (n, %) | 18 (17%) | 15 (7%) | 0.033 |
| Systolic blood pressure (mmHg) | 132.8±35.4 | 125.4±28.9 | NS |
| Number of infant deliveries (n) | 4.3±1.5 | 3.8±1.1 | NS |
| Duration of breast feeding (months) | 47.4±20.0 | 35.9±17.9 | NS |
| Menopausal status | |||
| Postmenopausal duration (years) | 9.3±2.6 | 6.4±1.9 | 0.04 |
| Age at menopause (years) | 48.3±11.4 | 50.1±12.2 | NS |
| Body mass index (kg/m2) | 31.6±6.3 | 26.3±5.4 | NS |
| Waist circumference (cm) | 96.1±22.2 | 90.9±21.9 | NS |
| LDL cholesterol (mmol/L) | 130.8±29.7 | 129.9±27.3 | NS |
| HDL cholesterol (mmol/L) | 52.5±15.2 | 61.3±16.8 | 0.049 |
| Triglycerides (mmol/L) | 151.7±76.6 | 127.9±76.0 | NS |
| Fasting glucose (mg/dL) | 122.7±35.3 | 115.8±31.6 | NS |
| Metabolic syndrome (n, %) | 65(61.9%) | 32(15.6%) | <0.001 |
BAC: breast arterial calcification; LDL: low-density lipoprotein; HDL: high-density lipoprotein; NS: not significant.
The ages of the women participating in this study ranged from 40 to 73 years, with an average of 55.9±8.4 years. The mean ages of the BAC (+) and BAC (-) groups were 60.7±9.4 years and 53.4±6.2 years, respectively (p<0.001). The mean postmenopausal periods for the two groups were 9.3±2.6 years and 6.4±1.9, respectively (p = 0.04).
The incidences of hypertension and DM were higher among the BAC (+) subjects than among the BAC (-) subjects (p = 0.016 and p = 0.033, respectively). Systolic blood pressure was higher in the BAC (+) group, in which more childbirths, longer breastfeeding durations, greater BMI scores and larger waist circumferences as well as higher levels of LDL cholesterol, triglycerides and fasting glucose were also reported; however, these differences were not statistically significant. The mean HDL cholesterol levels were significantly lower among the BAC (+) subjects than among the BAC (-) subjects (52.5±15.2 dL vs. 61.3±16.8 dL, respectively; p = 0.049). The BAC (-) group reported significantly higher cigarette consumption than did the BAC (+) group (7.6% and 26.3%, respectively; p = 0.011).
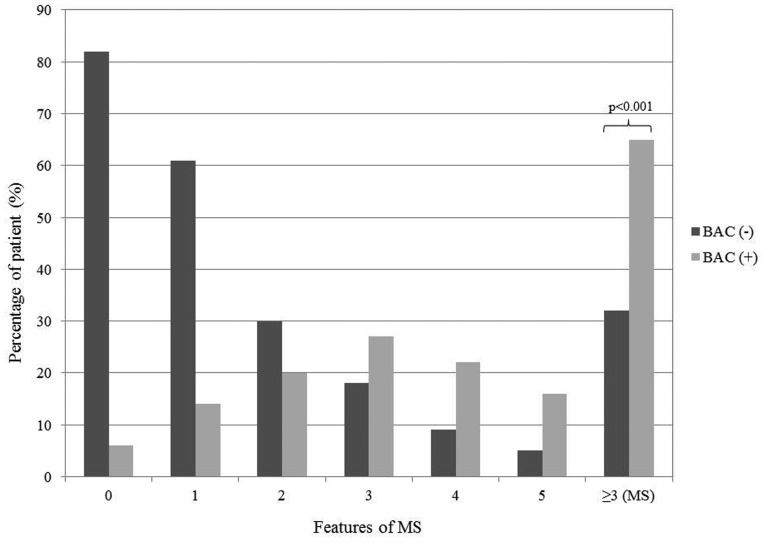
In our study population, the overall prevalence of MS was 31.3%. The prevalence of MS was significantly higher in the BAC (+) group than in the BAC (-) group (61.9% vs. 15.6%, respectively; p<0.001) (Figure2). In a comparison of the individual parameters constituting MS between the BAC (+) and BAC (-) groups, the BAC (+) was found to contain higher percentages of patients with high fasting blood glucose levels (45.7% and 30.7%, respectively; p = 0.041), low HDL cholesterol levels (21.9% and 9.8%, respectively; p = 0.015) and high blood pressure (59.1% and 34.6%, respectively; p = 0.01). In a comparison of waist circumferences and serum fasting triglyceride levels between the two groups, no statistically significant differences were found (Table2).
Univariate and multivariate analyses for the association of MS features and age with the presence of breast arterial calcification.
| Univariate analysis | Multivariate analysis | |||||
|---|---|---|---|---|---|---|
| BAC (+) n = 105 | BAC (-) n = 205 | p-value | OR | 95% CI | p-value | |
| Age | 57.7±9.4 | 46.4±6.2 | <0.001 | 1.3 | 1.1–1.6 | 0.001 |
| Waist circumference>88 cm (n, %) | 66 (62.9%) | 105 (48.8%) | 0.72 | 1.1 | 0.1–9 | 0.92 |
| HDL cholesterol <50 mg/dL (n, %) | 23 (21.9%) | 20 (9.8%) | 0.015 | 8.1 | 1.0–64.0 | 0.047 |
| Fasting serum triglyceride ≥150 mg/dL (n, %) | 75 (71.5%) | 105 (48.8%) | 0.94 | 0.3 | 0.3–2.5 | 0.26 |
| Fasting serum glucose ≥110 mg/dL (n, %) | 46 (45.7%) | 63 (30.7%) | 0.041 | 2.7 | 0.5–14.9 | 0.23 |
| High blood pressure ≥130/85 mmHg (n, %) | 62 (59.1%) | 71 (34.6%) | 0.01 | 8.7 | 1.5–49.7 | 0.014 |
BAC: breast arterial calcification; OR: odds ratio; CI: confidence interval; HDL: high-density lipoprotein.
In one multivariate model, age (OR = 1.3, 95% CI = 1.1−1.6, p = 0.001) and metabolic syndrome (OR = 4.0, 95% CI = 1.5−10.4, p = 0.005) were found to be independent predictors of BAC (Table3). Among the features of MS, low high-density lipoprotein (HDL) levels (OR = 8.1, 95% CI = 1.0−64.0, p = 0.047) and high blood pressure (OR = 8.7, 95% CI = 1.5−49.7, p = 0.014) independently predicted the presence of BAC (Table2).
Results of multivariate analysis for predictors of the presence of breast arterial calcification.
| Odds ratio | 95% CI | p-value | |
|---|---|---|---|
| Age | 1.1 | 1.1–1.2 | 0.001 |
| Cigarette smoking | 3.4 | 1.4–35.7 | 0.24 |
| Postmenopausal duration | 6.3 | 1.2–45.9 | 0.37 |
| Metabolic syndrome | 4 | 1.5–10.4 | 0.005 |
BAC: breast arterial calcification; CI: confidence interval.
In the univariate analyses, cigarette consumption and postmenopausal duration were statistically significant; however, these factors were not determined to be independent predictors for BAC in the multivariate analysis. Classic hypertension (OR = 2.4, 95% CI = 1.2−7.5, p = 0.002) was an independent predictor of BAC (+) patients in a multivariate model that included classic hypertension, DM and HDL cholesterol.
DISCUSSIONThe present study represents a unique evaluation of the relationship between BAC and MS in postmenopausal women. Our results indicate that the detection of BAC via mammography is associated with MS in a relationship that is apparently independent of age.
Breast arterial calcification, which is occasionally reported as benign, develops as a result of extensive calcification of the small- to medium-sized muscular arteries in the breast and is commonly found on mammograms (7,8). The reported frequency of BAC detected via mammography in previously published studies varies from 1% to 49% (6); our study indicates a 16.6% prevalence rate.
Associations between BAC detected via mammography and reproductive factors such as the duration of breastfeeding, the number of infant deliveries, early menopause and the duration of menopause have previously been reported (19–21). In these studies, hormonal changes during pregnancy and milk production during lactation were considered to be determinants of BAC formation. In our study, the number of infant deliveries and the duration of breastfeeding were higher in the BAC (+) group than in the BAC (-) group, but the differences were not statistically significant. Although the duration of menopause was longer in the BAC (+) group, this factor was not found to be an independent predictor of BAC.
A relationship has been established between age and medial arterial calcification (6). In our study, the rate of BAC was also observed to increase significantly with age.
Several studies have demonstrated relationships between BAC and coronary artery disease (9,10) and between BAC and cardiovascular risk factors such as hypertension (11), DM (11–14), biochemical findings (22) such as hypertriglyceridemia and high levels of homocysteine and high-sensitivity C-reactive protein (hs-CRP) and the body mass index (23). Although both conventional DM and hypertension were more prevalent in our BAC (+) group, only hypertension was found to be an independent predictor of BAC in our study. Smoking, despite its established relationship with coronary artery disease, was more prevalent in the BAC (-) patients; however, according to the multivariate analysis, smoking was not an independent risk factor. The inverse association between smoking and BAC observed in the present study is consistent with previous reports (24,25).
Although cardiovascular risk factors are associated with both coronary artery disease and BAC, studies of the development of BAC have indicated that different basic factors play the more important role in the pathogenesis of BAC. Whereas atherosclerosis results in marked intimal calcification of the coronary arteries, calcification of the tunica media is more predominant in BAC (26). Inflammation, lipid storage and vascular smooth muscle cells play an active role in intimal calcification; however, in medial calcification, macrophage and lipid accumulation is not evident (27,28). At present, it is impossible to definitively distinguish between intimal and medial calcification using digital mammography.
Patients with coronary artery disease were excluded from the present study because several prior studies have already investigated the relationship between coronary artery disease and BAC (9,10,29). In a meta-analysis of 927 patients, the incidence of coronary artery disease diagnosed via angiography was found to be higher in patients with BAC (+) mammograms (30). Another study demonstrated no independent relationship between BAC and coronary artery disease diagnosed via angiography (29). In that study, patients with significant coronary artery disease were compared with patients with normal coronary arteries. Patients with non-significant coronary artery disease, however, were not included in the study, which might explain the discrepancy.
Carotid intima-media thickness is a well-known marker of early atherosclerotic disease. Two independent studies have demonstrated that BAC is associated with carotid intima-media thickness independent of age; reproductive factors, such as parity and postmenopausal duration; and cardiovascular risk factors, including diabetes, systolic blood pressure, fasting glucose levels and triglyceride levels (15,16).
Metabolic syndrome is associated with an increased risk of coronary artery disease. MS results from a combination of cardiovascular risk factors, including high blood pressure, insulin resistance or glucose intolerance, visceral obesity and atherogenic dyslipidemia (1,2). The prevalence of MS increases with age, particularly after menopause. In a study of patients of over 45 years in age, the prevalence of MS was reported to be as high as 40% (3,4). Although several clinical studies have investigated the relationships between BAC and cardiovascular risk factors, coronary artery disease, other vascular diseases and reproductive factors, only one study has explored the relationship between MS and BAC. This study found that the incidences of diabetes and MS were higher in the BAC (+) group than in the BAC (-) group (31). It also demonstrated that MS was the only independent predictor of BAC. In our study, a significant association was found between BAC and MS, independent of age, smoking and postmenopausal duration. When the parameters constituting MS were examined individually, independent of age, low HDL cholesterol levels and high blood pressure were found to be accurate predictors for BAC. One limitation of the present study is that it was performed in a local region and therefore, the sample may not be representative of the general population. Because the relationship between MS and coronary artery disease has been well established (2), efforts were made to exclude patients with known coronary artery disease from the study. Second, asymptomatic patients with coronary artery disease could not be effectively excluded and therefore, some of the patients diagnosed with MS might have had asymptomatic coronary artery disease. Third, a relatively small number of BAC (+) patients were included in this study; hence, additional large-scale trials are required to confirm our findings.
In conclusion, the likelihood of the detection of BAC on mammography increases with age as well as in the presence of hypertension and MS. In BAC (+) screening mammography patients, the possibility of MS should be considered because BAC is closely associated with coronary artery disease and cardiovascular risk factors. Based on the results of this study, we recommend that patients with BAC should be informed of their cardiovascular risk factors and encouraged to consider appropriate lifestyle changes.
AUTHOR CONTRIBUTIONSYildiz S, Toprak H, Oktay V, Abaci O and Kocas C designed the study, performed the statistical analysis of the results and wrote the manuscript. Aydin S and Bilgin M collected the patient data and contributed to the Discussion section.
No potential conflict of interest was reported.