Despite the high prevalence of substance abuse and mood disorders among victimized children and adolescents, few studies have investigated the association of these disorders with treatment adherence, represented by numbers of visits per month and treatment duration. We aimed to investigate the effects of substance abuse and mood disorders on treatment adherence and duration in a special program for victimized children in São Paulo, Brazil.
METHODS:A total of 351 participants were evaluated for psychiatric disorders and classified into one of five groups: mood disorders alone; substance abuse disorders alone; mood and substance abuse disorders; other psychiatric disorders; no psychiatric disorders. The associations between diagnostic classification and adherence to treatment and the duration of program participation were tested with logistic regression and survival analysis, respectively.
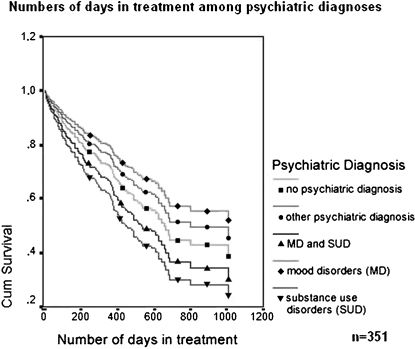
RESULTS:Children with mood disorders alone had the highest rate of adherence (79.5%); those with substance abuse disorders alone had the lowest (40%); and those with both disorders had an intermediate rate of adherence (50%). Those with other psychiatric disorders and no psychiatric disorders also had high rates of adherence (75.6% and 72.9%, respectively). Living with family significantly increased adherence for children with substance abuse disorders but decreased adherence for those with no psychiatric disorders. The diagnostic correlates of duration of participation were similar to those for adherence.
CONCLUSIONS:Mood and substance abuse disorders were strong predictive factors for treatment adherence and duration, albeit in opposite directions. Living with family seems to have a positive effect on treatment adherence for patients with substance abuse disorders. More effective treatment is needed for victimized substance-abusing youth.
Child and adolescent victimization is a global public health problem. In the United States, it is estimated that between 2005 and 2006, 1,256,600 children suffered some kind of abuse, with 58% experiencing physical abuse, 27% experiencing emotional abuse, and 24% experiencing sexual abuse (1). In Brazil, it is estimated that there are approximately 28 million victimized children and adolescents (2). Severe physical punishment for children and adolescents is also highly prevalent (10.1%) (3). Domestic violence increases the risk of later psychiatric problems and other adverse life events, such as homelessness (4).
Children with a history of mistreatment who were also separated from their parents are more susceptible than others to mental disorders (5). Mental health problems are estimated at between 30% and 85% of youths in out-of-home placements or living in group shelters, with about four times the rate of serious psychiatric disorders as those remaining with their own families (5). The most common of these disorders have been reported to include depression, social disorders, anxiety, and PTSD (7). Few studies of this population have focused on issues of both substance abuse disorders (SUD) and non-substance-abuse behavioral disorders, and none have focused on the specific impact of mood disorders (MD), which are associated with distinct impairments in psychosocial function, including academic deficits, family conflicts, legal problems, substance abuse, and suicidal behavior, all of which may add to their risk of prematurely dropping out of treatment and/or becoming homeless (8).
Treatment adherence has been investigated for many psychiatric disorders and is, at face value, an important quality indicator and a potential proxy outcome measure. Although quality measures for adult psychiatric care have received extensive scrutiny, such measures have received little attention among children/adolescents (9), and there are virtually no studies of victimized children and adolescents who have been placed in group shelters with non-familial supervision. Studies have suggested that SUD is associated with poorer adherence to treatment, both for adults and adolescents (10–12), and premature dropout has been found to be strongly associated with many comorbidities (13). The few studies of treatment adherence among adolescents with MD have focused exclusively on medication non-adherence, with estimates ranging from 10 to 60% (14), but there are few data about overall treatment adherence.
Despite the high prevalence of psychiatric disorders in victimized children, no previous study, to the best of our knowledge, has focused on the impact of MD, SUD and the interaction of SUD and MD on the treatment of victimized children and adolescents living in group shelters. This prospective study investigates the association of SUD and MD, among other factors, with treatment adherence and early dropout in victimized children and adolescents (most of whom were formerly homeless) referred by the juvenile court system to an intensive treatment program in São Paulo, Brazil.
METHODSTreatment InterventionThe Equilibrium Project (TEP). TEP is an interdisciplinary intervention program whose goal is to provide multi-dimensional bio-psycho-social treatment for children and adolescents referred by the juvenile court system for intensive treatment. The vast majority of TEP participants had been living on the streets or in slums prior to placement in group shelters with supervision. Children and adolescents are referred for assessment and treatment due to mistreatment, which can include neglect or emotional, physical and/or sexual abuse. TEP offers comprehensive mental and physical health care along with social services in an Urban Community Center where participants can receive specialized services and support for school attendance while participating in social and recreational activities with their peers. Although all patients are referred by a judge, participation is voluntary. The ultimate goal of the program is active community reintegration. At entry, interpersonal violence within the families is carefully assessed and addressed by family therapy at the appropriate intensity. In Brazil, many parents lack the resources to support their children, and they sometimes become abusive due to the stresses of extreme poverty. The juvenile court system is reluctant to order permanent family separation and prescribes intensive treatment, when available, with the goal of family reunion before removing children from the family for adoption. The goals of treatment are thus to decrease symptoms, promote adequate education and social development, and ultimately enable social and family reintegration. More details on TEP have been presented elsewhere (15).
Initial Evaluation and Psychiatric DiagnosesChildren and adolescents are referred to TEP either directly by the juvenile court system of São Paulo or indirectly by supervisory shelter staff after mandated placement in a group shelter. The primary caregiver, whether shelter staff or, less often, a family member, is engaged in the initial evaluation. A clinical evaluation is conducted to identify medical or nutritional problems that might hinder the psychological assessment process. Socio-demographic characteristics, prior and present stressors, family and clinical history are formally evaluated. During the subsequent four-week "Diagnostic Phase", detailed assessments, including a neuropsychological assessment, are completed by multiple professionals. Psychiatric diagnoses are made by psychiatrists specializing in child and adolescent psychiatry using the K-SADS (Schedule for Affective Disorders and Schizophrenia) (16).
Individualized Intervention PlanAfter the initial assessment, an individualized intervention plan is constructed to meet each childs needs, which may include psychiatric consultations, individual or group psychotherapy, occupational therapy, speech therapy, psycho-educational therapy, physiotherapy, social work assessment, family therapy, physical activities, or art therapy. In addition to these therapeutic interventions, participants are also encouraged to participate in ongoing recreational activities.
Considering that children with a history of mistreatment who were also separated from their parents are more susceptible than others to mental disorders, even those children that are not diagnosed with a mental disorder at the initial evaluation are included in therapeutic intervention focused on preventive strategies and supportive psychotherapy. For example, those children may participate in group speech therapy, to improve communication skills; psycho-educational support, to improve learning abilities; occupational therapy, to develop new abilities not developed previously because of poor stimulation; or group psychotherapy, to improve self-esteem.
Long-term Supervision and Case ManagementIn order to follow patients from the initial contact in group shelters (or occasionally on the streets) to the point of full socio-family reintegration, the program has adopted a case management strategy in which one professional from the TEP team is identified as the focal point of service for each child/adolescent. The case manager modifies the treatment plan according to changes in the childs needs while actively engaging other team members and agencies to promote school, family and social reintegration. The case manager also maintains active links with the juvenile court system. Attention to the familýs needs, apart from those of the child or adolescent, is attempted when possible. The team thus works actively with other partner organizations and natural supports to provide continuous care, developing the childs confidence in the case manager as a central means of preventing program attrition. When patients are absent for more than two weeks, the case manager makes assertive efforts to renew contact. However, assertive community outreach is often not possible because of security concerns in some neighborhoods.
Study Design and EthicsThis prospective observational study examined the association of psychiatric disorders with treatment adherence, controlling for potentially confounding factors. IRB approval for this study was obtained from the Hospital das Clínicas research ethics committee of the University of São Paulo Faculty of Medicine. To be eligible for this study, patients and their legal guardians signed an approved consent form.
Sample Characteristics, Inclusion and Exclusion CriteriaAll children/adolescents admitted to TEP between September 2007 and September 2009 were enrolled in this study. The inclusion criteria for admission to TEP included: 1) living in a socially vulnerable, high-risk situation, as determined by the juvenile court system; and 2) no longer living in the streets, i.e., living either in a group shelter or, in selected cases, with their original family. Exclusion criteria were: 1) children or adolescents from locations other than São Paulo; 2) age greater than 19 years at first assessment; 3) refusal of all healthcare assessments or services. Because the children/adolescents were referred to this treatment by the juvenile court system, all of them underwent the initial assessment. Some of them declined to continue the follow-up treatment and were considered dropouts, as described below (outcome measures).
Data Collection and MeasuresVariables available for analysis include age, gender, psychiatric diagnosis (according to DSM-IV criteria) (17), residence at the time of treatment referral (i.e., living with family, in a group shelter or on the streets), and documented social stressors. Social stressor data were collected at the first assessment and classified according to the parameters listed in the Z axis of the 10th International Classification of Diseases (18). Program data documented the number of clinical visits, the date of the last visit, and the reason for termination.
Outcome measures thus addressed both treatment adherence and the total treatment duration. While therapeutic plans were individualized, all participants were scheduled to attend group activities at TEP at least once a week. Patients were considered as “adhering to treatment” if they attended the clinical program at least twice a month (i.e., recreational activities were not considered in the measure of adherence, although they were considered important for maintaining treatment motivation).
In the survival analysis of treatment duration, patients who were still in treatment at the end of data collection, who were considered to have been discharged successfully or who had moved to other cities were censored at the time of their last contact. Those who stopped attending the program or asked to be referred to other treatment centers were considered to have “dropped out” at the time of their last visit.
Data AnalysisThe primary predictor of interest was a diagnostic indicator that classified each participant into one of five mutually exclusive groups: 1) MD, 2) SUD without MD, 3) MD and SUD, 4) other psychiatric disorders (OPD), and 5) no psychiatric disorder (NPD). First, an analysis of co-variance and the Kruskal-Wallis test for normality were used to identify correlates of the diagnostic classification that might confound the relationship of diagnosis with the outcomes of interest. Gender, age, number of social stressors, and residence with family at the beginning of treatment were all analyzed as possible confounding factors.
Next, logistic regression was used to identify the relationship between the diagnostic groups to the dichotomous measure of treatment adherence, while controlling for significant co-variates. The reference condition in this analysis was individuals with mood disorders alone (MD). In a second analysis, the interaction between the participant's residence (shelter or with family) at the time of program entry and the diagnostic conditions was examined. Finally, a survival analysis of the duration of program participation was conducted as defined above, adjusting for the same potentially confounding covariates.
Data were analyzed with SPSS version 14.0 for Windows (Research on Research Group, Duke University, Durham, North Carolina, USA). A suite of web applications was utilized to facilitate the data analyses (19).
RESULTSA total of 351 children/adolescents participated in the program; 68.09% (n = 239) were male, with a modal age between 12 and 19 years old (65%) (range from 3 to 19 years old, median age: 13 years old). The lifetime prevalence of any psychiatric disorder was 86.3% (n = 303). The most prevalent were SUD (39%, n = 137), MD (37%, n = 130), hyperkinetic disorder (16.2%, n = 57), and anxiety disorder (8.8%, n = 31). More than half of the sample reported a history of physical or sexual abuse (58.4%, n = 205).
There were significant bi-variate differences across diagnostic groups, including gender, age, number of psychiatric diagnoses, and, prior to adjustment, the proportion who met the criteria for adherence (Table 1). There were more males among patients with SUD and OPD than among NPD patients (p = 0.002). Patients with SUD or both MD and SUD were older than patients with MD alone, who were in turn older than OPD and NPD patients (p<0.001). There were more children living in group shelters in the MD group than in the SUD group (p<0.001). The MD with SUD group, as expected from the group definition, had more comorbidities than the other groups (p<0.001). The presence of social stressors was not significantly different among groups. Bivariate analysis revealed that the highest rate of adherence was in the MD group and that the lowest rates of adherence were in the SUD and the MD with SUD groups.
Socio-demographic characteristics of victimized children/adolescents attending a multidisciplinary treatment program (n = 351).
| Variables | MD (n = 88) | SUD (n = 95) | MD + SUD (n = 42) | OPD (n = 78) | NPD (n = 48) | p-valueDF |
|---|---|---|---|---|---|---|
| gender (male, %)a | 67 | 75.8 | 54.8 | 79.5 | 52.1 | .002DF:4 |
| years of age (mean±SD)b | 12.02±3.15 | 14.85±2.24 | 14.14±2.04 | 10.78±3.38 | 9.85±3.61 | <.001DF:4 |
| residence at the time of referral (%)c, dgroup shelterfamily housestreets | 93.26.80 | 72.623.23.2 | 78.614.37.1 | 82.115.42.6 | 83.316.70 | .051DF:12 |
| Number of psychiatric diagnoses other than MD and SUD∗ | 1.68±0.86 | 1.48±0.70 | 2.24±0.58 | 1.44±0.62 | 0.23±0.43 | <.001DF:4 |
| Number of social stressors∗ | 1.90±0.96 | 1.93±1.32 | 1.90±0.94 | 1.86±1.05 | 2.00±0.87 | 0.634DF:4 |
| Patients who adhered to treatment | 79.5 | 40 | 50 | 75.6 | 72.9 | <0.001DF: 4 |
Abbreviations and notes: MD, mood disorder; SUD, substance use disorder; OPD, other psychiatric disorders (not MD or SUD); NPD, no psychiatric diagnoses; DI, delinquent institution. (∗): Kruskal-Wallis; a) SUD = OPD>NPD; b) SUD = MD+SUD>MD>OPD = NPD; c) Living in group shelter: MD>SUD (p<.001, with Bonferroni correction [BC]); d) one patient from the SUD group was living in an institution for delinquents at the time of referral and was not included in the table. DF: degrees of freedom.
After adjustment for significant covariates, patients in the SUD and MD with SUD groups were both significantly less likely to be in adherence than those in the MD group (Table 2). An examination of 95% confidence intervals shows no significant difference between these two groups or between MD and either the OPD or NPD groups.
Multiple logistic regression: odds ratio represents the likelihood of adherence to treatment controlling for potential confounding characteristics, with mood disorders as the reference condition (n = 351).
| Psychiatric Diagnosis | Odds Ratio | 95% Confidence Interval Lower | 95% Confidence Interval Upper |
|---|---|---|---|
| SUD | 0.246b | 0.123 | 0.492 |
| MD+SUD | 0.335a | 0.148 | 0.757 |
| OPD | 0.658 | 0.309 | 1.400 |
| NPD | 0.494 | 0.209 | 1.170 |
Abbreviations and notes: SUD, substance use disorder; OPD, other psychiatric disorders (not MD or SUD); NPD, no psychiatric diagnosis.
a) p<0.01;
b) p<0.001.
There were also no changes in treatment adherence rates after controlling for the total treatment duration (number of days), which was itself significantly associated with greater adherence (p<0.001; data available upon request).
The likelihood of adherence among participants who were living with family at entry was also examined as a possible modifier of the likelihood of treatment adherence within the diagnostic groups. SUD patients had a greater likelihood of adherence if they were living with family (p = 0.015), increasing the odds ratio to 0.64, in contrast to 0.25 for the SUD group as a whole compared with the MD group. On the other hand, living with family decreased the likelihood of treatment adherence for those with NPD (p = 0.03, odds ratio = 0.10, compared with 0.49 for the group as a whole compared with the MD group); (data not shown, but available on request).
In the survival analysis conducted to identify predictors of participation duration, older patients showed a greater likelihood of dropping out (p = 0.003), while those who were living in a group shelter at entry were less likely to drop out than those living with their families (p = 0.018).
Figure 1 shows that, after adjusting for potential confounders, patients with MD tended to participate the longest, and SUD patients tended to drop out of treatment earlier than did MD patients (p = 0.083). Patients with both SUD and MD stayed in treatment slightly longer than did patients with SUD alone.
DISCUSSIONIn this study, we examined five diagnostically distinct groups of victimized children from São Paulo, Brazil, mostly formerly homeless, to compare differences in treatment adherence and the duration of program participation. Children/adolescents with MD showed a greater likelihood of treatment adherence and tended to remain in treatment longer, while those with either SUD or both SUD and MD were less likely to adhere to treatment and tended to drop out earlier. Children with SUD who continued to live with their families rather than in a shelter showed better adherence, but there was a reduced likelihood of adherence among children with no psychiatric diagnoses who lived with their families. To our knowledge, this is the first study of the association of psychiatric diagnosis and other factors with treatment adherence and the duration of treatment participation among high-risk children and adolescents (most of whom were formerly homeless) in a low- or middle-income country.
One possible reason why children/adolescents with MD exhibited better treatment adherence and remained in treatment longer than patients in other groups is that depression can be effectively treated with medication, which typically reduces core symptoms in a short period of time (two weeks on average), a potentially important positive factor in the promotion of treatment adherence. Virtually all publications on the adherence to MD treatment in children focus on medication adherence and highlight the importance of extended medication use in improving long-term outcomes (14). It is unlikely that these results were influenced by conduct disorder (CD) or oppositional defiant disorder (ODD). ODD diagnosis is usually made at an early age, generally before the mean age of our SUD patients, so we were confident that the prevalence of ODD in this group was very low. At the same time, a diagnosis of CD is frequently associated with SUD, but the vast majority of the behavioral problems seen in these patients are secondary to substance abuse and may be resolved simply by the cessation of drug abuse (20).
Previous studies have shown that a high dropout rate is one of the major challenges in the treatment of SUD in both adults and adolescents (12,13,21). In our sample, SUD patients also showed poorer adherence to treatment than other patients and dropped out earlier. In addition, there were no differences between patients with SUD only and those with both SUD and MD, even after adjusting for age, gender, and place of residence at the time of referral. These findings are similar to others in the literature, which also indicate that patients with SUD in combination with other psychiatric disorders tend to show less adherence to treatment and to drop out earlier (13). The only other study of adherence to treatment among homeless adolescents with SUD similarly reported that children with a history of sexual abuse and suicide attempts remained in treatment longer than did children with different profiles (22). However, that study had some limitations compared with this study, in that it lacked specific information on the presence of comorbid MD. TEP, with its well-staffed, multidisciplinary clinical team and its commitment to addressing a wide range of needs using an open-door policy and a non-judgmental posture, might have helped to improve adherence for victimized children in general, but apparently not enough to increase treatment adherence in children/adolescents with SUD only.
The treatment of SUD patients is thought to require a long period of monitoring to obtain clinical improvement (23). Residence with family seems to be more important for treatment adherence among SUD patients than other diagnostic groups, suggesting that family support may be especially important, when feasible, in keeping patients engaged and motivated. One possible reason for this finding is that the adverse impact of substance abuse on the family may be greater than that of other psychiatric disorders and may thus increase the family's encouragement of continued treatment, even in a voluntary program. In contrast, children/adolescents who were still living with their families had all been referred to treatment because they had suffered some kind of abuse, albeit to a mild degree. Given that children most often require an adult to bring them to treatment, it was expected that those who were living in dysfunctional families would have more difficulty in coming to treatment and would ultimately drop out during follow-up. Children at high social risk but with no psychiatric disorders who live with their families seem to be less likely to adhere to treatment and are more likely to drop out, even if the family also receives assistance. In this program, the children received transportation vouchers to help them attend the program, but this did not seem to improve adherence. It is likely that these families already face many other problems, like poverty, poor housing conditions and neighborhood violence, and they may not be interested in receiving preventive psychiatric care if their children have not yet shown evidence of a psychiatric disorder, even when they were considered to be at high risk by the juvenile court system.
Interventions for foster children who have been victimized and homeless can be either narrowly symptom-focused or broadly system-focused (24). The few specific interventions designed for this population have not been well-analyzed because this population is particularly difficult to treat or evaluate (25). Pam and collaborators identified five main challenges in providing care for these children: 1) the complexity of their clinical needs; 2) understaffing that leaves caregivers little time for each child; 3) poor integration between the social welfare, criminal justice, educational, and health care systems; 4) the precarious nature of the social supports available to these children and adolescents; and 5) the frequent interruptions to follow-up treatment efforts due to high levels of staff turnover (26). The results of this study suggest that, in spite of these difficulties, an intensive treatment program coupled with group shelter can yield high levels of treatment adherence and longer stays for victimized children/adolescents if the treatment is focused on the broad range of needs, uses problem-specific interventions, and works in a network with other service providers, such as the educational and welfare systems. However, these efforts may not be sufficient for many victimized children/adolescents, especially those with SUD.
Several limitations of this study should be noted. First, it must be acknowledged that measures of treatment adherence and participation duration are, at best, proxy measures for clinical outcomes and program effectiveness. True outcome assessment is extremely difficult in studies with victimized children, especially in large cities like São Paulo where extreme poverty is common. Second, there may be a bias due to the sample recruitment method. We evaluated children/adolescents referred to our service from the juvenile court system, and although the treatment was not mandatory, it is possible that our sample over-represents at-risk youth with psychiatric disorders whom the court thought could benefit from treatment. Another potential limitation is that the K-SADS, the tool used to establish the diagnoses, has not been validated specifically for homeless victimized populations, and their high levels of environmental stress may complicate formal diagnostic assessment. However, other studies of children in group shelters or foster care that have attempted to assess mental health and behavioral function have based their diagnostic assessments on much more rudimentary methods, often relying on just a few global questions in far smaller samples. Thus, this study represents substantial progress over previous reports and includes the largest sample studied thus far of highly victimized, formerly homeless children and adolescents in a low- or middle-income country.
Because this study focuses on individuals whose neurocognitive capacities are still developing, neurocognitive function should be a focus of future research, along with neuroimaging and genetic vulnerability (27). Above all, future studies should evaluate the efficacy of specific interventions and their cost effectiveness. These children are likely to present high social costs in the future, and effective treatment may lower these costs, especially in the long term. This is especially important in developing countries with limited financial resources.
This observational study found that MD and SUD were strong predictive factors of treatment adherence and duration, albeit in opposite directions. Living with family seems to have a negative influence on treatment adherence and duration for children with no psychiatric disorders but a positive influence for children with SUD. Further studies should consider not only the psychiatric disorders of victimized children, but also family structure and dynamics. Brazil, like other low- and middle-income countries, is seeking to expand and improve its mental health services. Programs and public policies for victimized children and adolescents, especially those with substance abuse disorders, are needed especially urgently.
This study was partially funded by the Fundação Faculdade de Medicina (FFM), the National Institute for Developmental Psychiatry (INPD – supported by CNPq n° 573974/2008-0) and the São Paulo Municipality. The funding agencies had no influence on the design and conduct of the study; collection, management, analysis, and interpretation of the data; or the preparation, review, or approval of the manuscript. Ricardo Pietrobon and the "Research on Research" team supervised the literature matrix, manuscript templates and interpretation of statistical output (Duke University Health System, http://researchonresearch.duhs.duke.edu/site/). We would also like to thank Dr. Euripedes C. Miguel (INPD), Guilherme V. Polanczyk (INPD), and CEAPESQ-IPq for statistics support; FAPESP (Grant number 2010/15786-1 to Dr. Geraldo Busatto Filho; number 2010/15604-0 to Dr. Paulo Jannuzzi Cunha; and number 2010/18374-6 to Dr. Sandra Scivoletto), as well as the individuals at the São Paulo City Hall, public schools, foster centers and justice system who have worked together with The Equilibrium Project (TEP) and the University of São Paulo (USP).
Conflicts of interest:
Dr. Robert A. Rosenheck has received research support from Eli Lilly, Janssen Pharmaceutica, Astra-Zeneca and Wyeth Pharmaceuticals. He has been a consultant to GlaxoSmithKline, Bristol Myers Squibb, Organon and Janssen Pharmaceutica. He provided expert testimony for the plaintiffs in the UFCW Local 1776 and the Participating Employers Health and Welfare Fund, et al. vs. Eli Lilly and Company; for the respondent in Eli Lilly Canada Inc. vs. Novapharm Ltd. and the Minister of Health, and for the Patent Medicines Prices Review Board. He has also provided expert testimony for Canada in the matter of Janssen Ortho Inc. and “Risperdal Consta”. The other authors have received no funds from drug companies and have no conflicts of interest.
Scivoletto S conceived and designed the study, drafted the article, analyzed and interpreted the data, critically revised the article for important intellectual content, and approved the final version of the manuscript. Silva TF, Cunha PJ and Rosenheck RA drafted the manuscript, analyzed and interpreted the data and critically revised the manuscript regarding important intellectual content.