Recto-urethral fistula formation following radical prostatectomy is an uncommon but potentially devastating event. There is no consensus in the literature regarding the treatment of these fistulas. We present here our experiences treating rectourethral fistulas.
MATERIAL AND METHODSWe analyzed 8 cases of rectourethral fistula treated at our institution in the last seven years. Seven of the patients underwent repair of the fistula using the modified York-Mason procedure.
RESULTSThe causes of the fistula were radical retropubic prostatectomy in five patients, perineal debridement of Fournier's gangrene in one, transvesical prostatectomy in one and transurethral resection of the prostate in the other patient. The most common clinical manifestation was fecaluria, present in 87.5% of the cases. The mean time elapsed between diagnosis and correction of the fistula was 29.6 (7-63) months. One spontaneous closure occurred after five months of delayed catheterization. Urinary and retrograde urethrocystography indicated the site of the fistula in 71.4% of the cases. No patient presented recurrence of the fistula after its correction with the modified York-Mason procedure.
CONCLUSIONThe performance of routine colostomy and cystostomy is unnecessary. The technique described by York-Mason permits easy access, reduces surgical and hospitalization times and presents low complication and morbidity rates when surgically correcting recto-urethral fistulas.
As fístulas reto-uretrais são de acesso difícil e por vezes complexo, sendo seu fechamento espontâneo raro. Com o diagnóstico precoce e aumento do número de intervenções, principalmente a cirurgia por adenocarcinoma da próstata localizado, sua incidência apesar de rara vem crescendo. Nós demonstramos a nossa experiência dos casos de fístulas reto-uretrais entre 2000 a 2006 com uma serie de oito pacientes, sendo que sete realizaram correção da fístula pela Técnica de York Mason modificada.
Material e Método: Nos retrospectivamente analisamos os prontuários de todos os casos de fístulas reto-uretrais tratados no nosso serviço no período de 2000 a 2006. Sete de oito pacientes realizaram reparo da fístula através do procedimento de York Mason modificado.
RESULTADOSCinco pacientes tiveram a fístula como conseqüência da Prostatectomia Radical Retropúbica, sendo os outros três após debridamento devido a Fasceíte de Fournier, Prostatectomia Transvesical e Ressecção Transuretral da Próstata. A fecalúria foi o quadro clínico prevalente em 87,5% dos casos, o tempo médio entre o diagnóstico e a correção da fístula foi de 29,6 (7-63 meses) ocorreu um fechamento espontâneo após cinco meses de sondagem vesical de demora, a Uretrocistografia Retrograda e Miccional demonstrou a localização da fístula em 71,4%. Nenhum paciente apresentou recidiva da fístula após correção pela técnica de York Mason modificada. A colostomia foi realizada em 50% dos casos e não ocorreram casos de incontinência fecal ou estenose anal.
CONCLUÇÃOApós identificação de fístula reto-uretral, não é necessário à realização de colostomia e cistostomia de rotina. Sua correção pela técnica descrita por York Mason modificada nos propicia fácil acesso a sua localização, diminui o tempo cirúrgico e de internação, com baixos índices de complicações e morbidade.
Recto-urinary fistula is a serious and difficult to treat medical problem. About 60% of cases are caused by iatrogenic lesions occurring during surgical procedures (radical prostatectomy, cryosurgery, radiotherapy or brachytherapy of the prostate). Genitourinary trauma and infectious and inflammatory diseases are uncommon causes.1,2 These fistulas increase morbidity and mortality rates, result in longer hospitalization, increase health care costs and impair patients’ quality of life.
The most common clinical manifestations are dysuria and recurring cystitis, which are present in almost all cases. Other irritative symptoms, including pneumaturia and fecaluria, are also common. Gastrointestinal disturbances, such as diarrhea, abdominal pain and nausea, occur in 60% of cases3.
Although the diagnosis of recto-urethral fistula can be suggested through clinical history and physical examination, the correct localization of the fistula tract is extremely difficult. Radiological and/or endoscopic methods, such as tomography, urinary and retrograde urethrocystography, opaque enema, cystoscopy and rectosigmoidoscopy, are usually necessary. The use of cystoscopy is essential in view of its high sensitivity (80 – 100%)4.
The therapeutic approach utilized depends on the cause of the fistula, the patient's clinical condition, the experience of the surgeon and the presence of associated rectal and urinary pathologies. There is no consensus in the literature regarding the treatment of these fistulas. Surgical approaches for their correction include perineal, transanal, transanalsphincteral and combined abdominal and perineal access4.
We present here our experiences treating recto-urethral fistulas.
MATERIAL AND METHODSWe retrospectively analyzed 8 cases of recto-urethral fistulas treated at our institution in the last seven years. The data analyzed included: age, clinical history, etiology, diagnostic evaluation, treatment and complications. In all cases, the surgical approach for the fistula correction was the same as described by York-Mason5.
York - Mason Procedure5Urine culture and adequate treatment of the urinary infection were carried out. Bowel preparation was performed, and wide spectrum antibiotic therapy was begun 24 hours before the start of the procedure and continued until the seventh post-operative day.
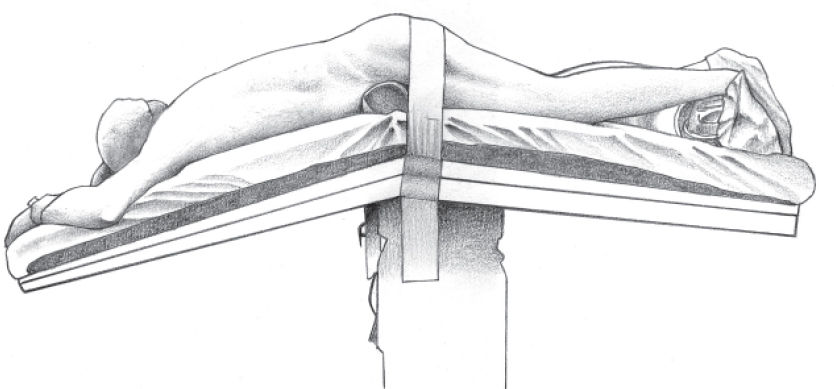
SurgeryThe patient with a previously placed 20-F Foley catheter was given a general anesthetic and placed in a ventral supine position flexed at the level of the femoral thigh joint. The thorax and abdomen were accommodated in such a way as to minimize breathing limitations that result from the position (Figure 1).
Both gluteals were held back with adhesive tape (Figure 2).
The incision was performed at the level of the anal margin rising to the level of the coccyx (a small variation from the York-Mason technique, which describes the incision laterally to the left towards the iliac sacrum)5. After the skin incision, the mucous cutaneous junction was marked to make the later reconstruction easier.
Next, the internal sphincter, the external sphincter and pubo-rectal muscles were incised and marked with sutures in such a way as to make the later closure easier.
At this point, the posterior wall of the rectum was incised from the anal margin to the coccyx (which could be removed if necessary), exposing the anterior wall.
The fistula was identified in the anterior wall through the visible intraurethral Foley catheter (Figure 3).
In the first cases, we excised the entire fistulas tract. In the later cases we simply separated the two rectal wall flaps (cranial and caudal) from the urethra without removing the fistula tract (Figure 4).
Next, the urethra was closed using running sutures of chromed 4 zero catgut. The rectal flaps were sutured both transversally and posteriorly using polygalactine sutures (Figure 5).
Then, the rectal posterior wall was also sutured (Figure 6).
Finally, the threads that marked the muscle layers at the beginning of the procedure (external sphincter and pubo-rectal muscles) were tied off.
The Foley catheter was kept in place for 3 to 4 weeks.
Urethrocystography was performed on the day scheduled for the withdrawal of the catheter, which was then removed only if there was no leakage.
RESULTSThe mean age was 58.1 (53 −71) years. The fistula occurred as a complication of radical retropubic prostatectomy (RRP) stage T1 - T2 in five of the cases (62.5%). In two of these patients, RRP was performed as a rescue procedure after failed prostate radiotherapy. In the three remaining patients, the fistulas arose as a consequence of transurethral resection of the prostate (TURP), Fournier's gangrene debridement or transvesical prostatectomy (TVP). In this last case, the fistula correction was attempted unsuccessfully by an abdominal approach.
The most common clinical manifestation was fecaluria, present in seven of the cases (87.5%), followed by pneumaturia in one case (12.5%). The diagnosis and localization of the fistula were confirmed in 75% of the cases by urinary and retrograde urethrocystography (UCG) and by rectosigmoidoscopy, opaque enema and urethrocystoscopy in the remaining cases.
The mean time that elapsed between the diagnosis and the correction of the fistula was 29.6 (7 – 63) months. Before the definitive treatment of the fistula, 50% of the patients underwent colostomy, and 37.5% underwent cystostomy. Spontaneous closure of the fistula occurred in one patient after five months using a urethral catheter with no need for colostomy.
The York-Mason procedure was performed in seven of the patients (87.5%) with no recurrence of the fistula after a mean follow-up of 17 (3 – 32) months. AlI patients maintained fecal continence without anal stenosis, and just one patient experienced worsening urinary incontinence (Table 1). One patient presented a fecal fistula in the early postoperative period and underwent a colostomy. Intestinal continuity was restored 4 months later without recurrence of the fistula.
– Demographic data.
| Age | Etiology | Clinical Picture | Diagnosis | Colostomy | Cistostomy | Time before surgery (months) |
|---|---|---|---|---|---|---|
| 68 | TURP | Facalúria | Enema | Yes | No | 60 |
| 65 | RRP | Fecalúria | UCG | No | No | 7 |
| 66 | RRP | Fecalúria | UCG | No | No | 5* |
| 62 | Debridement after Fournier | Fecalúria | UCG | Yes | Yes | 20 |
| 53 | RRP | Fecalúria | Urethrocystoscopy | Yes | Yes | 19 |
| 71 | RRP | Fecalúria | Rectosigmoidoscopy | No | No | 18 |
| 66 | RRP | Pneumatúria | UCG | No | No | 20 |
| 70 | TVP | Fecalúria | UCG | Yes | Yes | 63 |
RRP was responsible for 62.5% of the recto-urethral fistulas in our study, which is similar to previous reports1. The time elapsed between injury and the correction of the fistula was 29.57 months. This period is longer than the six months usually recommended, probably because of a delay in diagnosing and referring patients to our Referral Center.
Fecal deviation before definitive correction of the fistula is a debatable subject. ln our study, 50% of the patients already had a colostomy upon admission to our institution. We usually do not perform fecal deviation before the definitive treatment. We observed that fecal deviation does not apparently affect the success of the York-Mason procedure. Stephenson and Middleton6 performed colostomies in seven of 13 fistula repairs and showed that this procedure is not necessary. Patients who did not undergo colostomy had a better quality of life while awaiting fistula correction. However, Al- Ali et al.7 performed routine in both procedures, cystotomy and colostomy, before correcting the fistula and observed the spontaneous closing of the fistula in 46.5% of their cases after six months. More than 70% the fistulas were traumatic in this study, which may explain the disparity between the two studies.
According to the literature, urethrocystoscopy is a highly sensitive technique to diagnose and localize the fistula when it is used routinely6. In our study, the UCG identified the fistula in 75% of the patients. Urethrocystoscopy should be performed if there is any doubt about the site of the fistula tract.
The incidence of rectal lesions during RRP varies from zero to 8.2% (Table 2). A study of a series of 2,212 patients who underwent RRP at the Mayo Clinic between 1996 and 1998 showed that the shorter the interval between the biopsy and the RRP, the greater the risk of lesion, and recommended waiting at least one month before undergoing surgery. Further, 37% of the patients who had a rectal lesion had undergone TURP previously, and 11.1 % had undergone radiotherapy8.
When rectal perforation is suspected during TURP, a conservative procedure may be adopted with prolonged urinary bypass, whether by the urethral or suprapubic route13. If the lesion occurs during RRP, its identification and suturing may avoid a future fistula. Couvalaire and Cukier14 defend suturing the lesion, interrupting the surgery and draining; Kuss et aI15 suggest completing the RRP, suturing the lesion and either performing a colostomy or introducing a high-absorption diet. Smith and Veenema16 did not observe any case of recto-urinary fistula in 15 cases of RRP with rectal lesion when colostomy was carried out. However, four of the 11 cases without colostomy developed a fistula. We believe that if rigorous hemostasis, visible suturing and draining are undertaken, then colostomy is unnecessary.
When conservative treatment of the fistula fails, surgical treatment becomes necessary. Munoz et aI17 described more than 40 different techniques that may be grouped as transabdominal, perineal, transanal or combined routes. The advantages of the transabdominal technique include the possibility of placing structures with omentum or peritoneum between the sutures, with the disadvantages of longer surgical time and longer hospitalization15.
The peritoneal approach described by Weyrauch18 and Young Stone19 and the transanal or transphincteric approach (the York-Mason technique) have the advantage of being less invasive, with minimal complications and low post-operative morbidity rates.
No cases of fecal incontinence after the York-Mason procedure were observed in our study, which agrees with previous reports.1,20–23 The correct identification and closure of the perineal muscle layers is probably crucial to avoid this complication.
In recent years, we observed an increase in the number and complexity of recto-urinary fistulas in our institution. Some of these fistulas deserve individualized treatment. For example, for patients with intrinsic sphincter deficiency, urethral stenosis and decreased bladder compliance, the best treatment option may be the closure of the bladder neck, augmentation cystoplasty and urinary continent diversion.
CONCLUSIONAfter identifying a recto-urethral fistula, routine colostomy and cystostomy are usually unnecessary. Prolonged urethral catheterization can promote spontaneous closure of the fistula in selected cases. When conservative treatment fails, fistula correction using the technique described by York-Mason makes the approach to the fistula tract site easier, reduces surgical and hospitalization times and presents low complication and morbidity rates.