The purpose of our study was to report the results of the implementation of computed tomography colonography in a university hospital setting serving a Brazilian population at high risk of colorectal cancer.
METHODS:After creating a computed tomography colonography service in our institution, 85 patients at high risk of colorectal cancer underwent computed tomography colonography followed by a same-day optical colonoscopy from September 2010 to May 2012. The overall accuracy of computed tomography colonography in the detection of lesions ≥6 mm was compared to that of optical colonoscopy (direct comparison). All colonic segments were evaluated using quality imaging (amount of liquid and solid residual feces and luminal distension). To assess patient acceptance and preference, a questionnaire was completed before and after the computed tomography colonography and optical colonoscopy. Fisher's exact test was used to measure the correlations between colonic distension, discomfort during the exam, exam preference and interpretation confidence.
RESULTS:Thirteen carcinomas and twenty-two lesions ≥6 mm were characterized. The sensitivity, specificity and accuracy of computed tomography colonography were 100%, 98.2% and 98.6%, respectively. Computed tomography colonography was the preferred method of investigation for 85% of patients. The preparation was reported to cause only mild discomfort for 97.6% of patients. According to the questionnaires, there was no significant relationship between colonic distension and discomfort (p>0.05). Most patients (89%) achieved excellent bowel preparation. There was a statistically significant correlation between the confidence perceived in reading the computed tomography colonography and the quality of the preparation in each colonic segment (p≤0.001). The average effective radiation dose per exam was 7.8 mSv.
CONCLUSION:It was possible to institute an efficient computed tomography colonography service at a university hospital that primarily assists patients from the public health system, with high accuracy, good acceptance and effective radiation doses. Our results seem to be comparable to other centers of excellence and fall within acceptable published guidelines, showing that a successful computed tomography colonography program can be reproduced in a South American population screened in a university hospital.
Colorectal cancer (CRC) is the third most common cancer, accounting for the second highest rate of cancer-related mortality in the Western world 1. Accurate pre-operative detection is crucial for planning curative treatment and increasing survival 2,3; however, the best means of diagnosis among the variety of resources and skills available at a given institution remains up for debate 4. A complete examination and colon screening can be achieved by colonoscopy (the current test of choice in many institutions), direct rectal visualization with sigmoidoscopy plus barium enema, or CT colonography (CTC) 5. CTC has improved rapidly since its appearance in the mid-1990s and has been established as an alternative to optical colonoscopy (OC) for colorectal cancer screening, especially for the detection of colonic polyps 6. In addition, CTC has fewer complications than OC, including reduced perforation rates and it can be better tolerated 2,3,7. Still, most of the available data concerning the accuracy of CTC have been taken from the setting of a well-structured CT division with experience in performing CTC studies. Thus, it remains unclear whether the success of evaluating high-risk patients in centers of excellence can be generalized to other places, such as university hospitals of below-average-income countries, since the large studies have been limited to well-developed countries 3,7. Despite the many reports about the technical aspects of CTC, no results have been published on screening CTC in a high-risk South American population.
CTC was introduced in our country in 2003 and, until recently, was only available for patients in the private health system. Since the end of the last decade, several public and university hospitals have become equipped with CT equipment to perform CTCs. Moreover, the number of trained professionals who perform and read CTC exams in diagnostic imaging departments has increased broadly, including at our center. Our ability to offer this exam to our patients has extended this screening to a greater segment of the population that can benefit from a sensitive and well-tolerated approach. In addition, we have instituted a training program for our interns, nurses and technicians. The aim of this study was to show the feasibility of implementing a CTC program at a university hospital that has limited resources and is focused on providing care to patients in the public health system, while obtaining results comparable to those from international institutions 3,6,.
MATERIALS AND METHODSPatientsApproval from the Institutional Review Board was obtained. All patients agreed to join the study and provided their signed consent. From September 2010 to May 2012, CTC followed by same-day OC were prospectively performed in 85 high-risk patients to screen for CRC. According to published guidelines, the criteria for high-risk colorectal cancer were the following: age over 40 years and bright/dark red fecal bleed or unexplained anemia and altered bowel habit/family history of CRC 1,6,11. Subjects were excluded from the study if they had inflammatory bowel disease, history of segmental colectomy or with colostomy, recent optical colonoscopy follow-up within the preceding two years, or any co-morbidity that would make OC unsuitable.
Bowel preparationThe preparation was composed of two days of a soft diet, two tablets of bisacodyl (Dulcolax®), simethicone (Luftal®), 10 sachets of Muvinlax® (macrogol, sodium bicarbonate, sodium chloride, potassium chloride) diluted in 1.5 L of water and 50 ml of ionic iodinated contrast (Telebrix®) the day before the CTC.
CT colonographyA well-trained CT technician carefully insufflated the colon using a rectal tube and a manual air delivery system. To ensure sufficient colon distension, a CT digital radiograph was acquired. Further insufflations were performed when the colonic distension was not sufficient in both positions (supine and prone). Images were acquired first from the supine and then from the prone position. When necessary, the lateral decubitus position was used to ensure sigmoid and left colon distension. CTC was performed in all patients with a 64-row MDCT (Brilliance 64®, Philips Medical Systems, Best, The Netherlands) without the use of intravenous contrast medium or peristaltic drugs. The imaging parameters for CTC were detector configuration, 64×0.625 mm; pitch, 1.1; gantry rotation time, 0.5 s; slice thickness, 1 mm; reconstruction increment, 0.7 mm; 120 kVp; 50 effective mAs; matrix, 512×512; and a fitting field of view.
The effective radiation dose was obtained from the report produced by the device at the end of each exam. Values are expressed as dose length product (DLP), which represents the radiation dose of a CT section multiplied by the length of the study. To calculate the effective radiation dose, the DLP was multiplied by a correction factor depending on the anatomical region studied. In CT scans of the abdominal region, the correction factor ranges from 0.015 to 0.018 12. In this study, we used a correction factor of 0.015 to estimate the effective dose of radiation. The result of this calculation is not an exact value of estimated radiation but can be used as a benchmark 12.
Optical colonoscopy and gold standardOn the same day, optical colonoscopy (OC) was performed after CTC within a 6-h interval, thereby avoiding the need for a second bowel purge. All patients received intravenous sedation (5 mg of midazolam hydrochloride). Optical colonoscopy examinations were performed by board-certified gastroenterologists. The location, shape and size of all identified polyps were described and the polyp sizes were measured using 8-mm-long biopsy forceps. Specimens for lesions larger than 5 mm were obtained by polypectomy, endoscopic mucosal resection, or biopsy. The endoscopists were unaware of the CTC findings.
Polypectomy was the gold standard for comparing CTC results, as assessed by segment. The colon was divided into six segments per patient (cecum, ascending colon, transverse colon, descending colon, sigmoid and rectum). To match the polyps seen on CTC and OC, two radiologists in consensus analyzed supine and prone CTC images and matched them with the optical colonoscopy findings based on colonic segment, size, shape and anatomical relationship to the haustral folds. For a given lesion to be recorded as a true positive, it had to be located in the same or an adjacent colonic segment; the two recorded sizes had to be the same within a 50% margin of error; and the lesion had to have similar morphology on both examinations. Polyps were categorized by size based on the optical colonoscopy results.
Interpretation of CTCAll CTC tests were analyzed by two radiologists (DAT and ACVA) in consensus. One was a specialist in abdominal radiology with seven years of experience in the interpretation of approximately 100 CTC scans per year (DAT) in a private service. Lesions were classified according to the American College of Radiology's (ACR) polyp classification (C1, smaller than 6 mm; C2, 6–9 mm; C3, 10 mm or larger). All examinations, even with poor preparation or poor distension were included in the analysis.
After CTC was performed, both radiologists evaluated the CTC datasets using the primary 3D method on a dedicated 3D workstation in addition to the 2D images. Electronic cleansing was not done for this interpretation. When a polyp was detected on CTC, the size, shape and location were recorded on a study report sheet. The shape of the polyp was described as flat, sessile, pediculed, ulcerated, or vegetating. Flat lesions were defined as mucosal elevations with a height less than 2 mm 13. Both the radiologists and the endoscopists used the same definition for a flat lesion.
Patient preference questionnairePatient acceptance of the CTC was evaluated by means of a semi-structured questionnaire applied before and after the CTC and CO that enabled us to evaluate the tolerance of the patients for the exam preparation, to assess any discomfort and to assess their preferences. The bowel preparation was defined as complete in cases of correct use of all medications by patients and as incomplete in those cases of incorrect use of all medications. Statistical correlations among the colonic distension, discomfort (subjectively informed by patients as “little”, “moderate” or “great”) expected and experienced, and preference for the type of exam (CTC or OC) were measured.
Quality of bowel preparationThe quality of the preparation was evaluated subjectively per segment using the following parameters: the degree of distension of colonic segments, the amount of residual marked feces, the amount of residual fluid and confidence in the diagnostics for each of the six segments of the large bowel. Colonic distension was rated as follows: a) non-distended segment b) proper distension and c) excellent distension 9,12. The amount of residual marked stool was rated as follows: a) no fecal residue b) only residues <5 mm c) residues with one to three particles ≥5 mm and d) residues with more than three particles ≥5 mm 8,10. The amount of residual fluid was rated as follows: a) absent b) occupied <25% of the intestinal lumen c) occupied between 25% and 50% of the lumen and d) occupied >50% of the intestinal lumen 8,10. Confidence in the diagnostic evaluation of each segment was rated as follows: a) not confident b) less confident and c) confident 10. In addition to the overall evaluation by radiologists, the tests were considered excellent (characterizing all lesions >6 mm), partially adequate (only characterizing lesions >10 mm) or inappropriate (not characterizing lesions >10 mm).
The statistical analysis was performed in a descriptive manner. Fisher's exact test was used for inferential analysis to study the associations between patient discomfort, colonic dilatation, patient preference and confidence interpreting the exams. In all findings obtained through the inferential analyses, the significance level α was equal to 5%. The per-lesion sensitivity, PPV, per-patient sensitivity, specificity, PPV and NPV were calculated with data pooled from all the radiologists. The sensitivities were compared per lesion and per patient for polyps ≥6 mm, using the OC as a reference standard for the 56 patients with complete OC exams. Data were entered into Excel 2010 for Windows spreadsheets for data storage. Statistical analyses were performed with the Statistical Package for the Social Sciences (SPSS) software release 19.0 for Windows. A p-value of less than 0.05 indicated statistical significance.
RESULTSEighty-five patients underwent CTC and were included in the study. The average age of the patients was 61 years, ranging from 31 to 88 years with a standard deviation of 13.0 years. Among the patients, 53 (62%) were female and 32 (38%) were male. Of the 85 patients studied, 78 (92%) underwent OC, of which 56 (72%) were complete and 22 (28%) were incomplete (due to CRC in 13/22 (59%) and conflicting colon issues in 4/22 (18%), among other causes).
CTC performanceAmong the seventy-eight patients submitted to OC, 367 colonic segments were evaluated, including 336 segments in 56 patients with complete OC exams (six segments per patient) and 31 segments in 22 patients with incomplete CO exams. Among the fifty-six patients with complete OC, the exams identified 22 lesions ≥6 mm in 19 patients (Tables1 and 2). Considering all 336 of the colonic segments studied and measuring the per-lesion accuracy of the method in detecting polyps greater than or equal to 6 mm and using the complete OC as a gold standard, we achieved an accuracy of 98.6%, sensitivity of 100%, specificity of 98.2%, NPV of 100% and PPV of 94.7%.
-Anatomopathological analysis of lesions ≥6 mm identified in computed tomography colonography and optical colonoscopy.
| Anatomopathological analysis | 6-9 mm [n = 5] | ≥1 cm-<3 cm [n = 11] | ≥3 cm [n = 6] |
|---|---|---|---|
| Adenocarcinoma | - | 3(27) | 3(50) |
| Low grade tubular adenoma | 3(60) | 1(9) | - |
| Inflammatory | 2(40) | - | - |
| Hyperplastic | - | 2(18) | - |
| Low grade tubulovillous adenoma | - | 1(9) | - |
| Villous adenoma | - | - | 1(16) |
| High-grade tubulovillous adenoma | - | - | 1(16) |
| High-grade villous adenoma | - | - | 1(16) |
| Lipoma | - | 2(18) | - |
| Leiomyoma | - | 1(9) | - |
| Chronic Colitis | - | 1(9) | - |
Numbers in parentheses are percentages %.
-Correlation between the morphology and dimensions of lesions ≥6 mm identified in computed tomography colonography and complete colonoscopies.
| Lesion morphology | 6-9 mm [n = 5] | ≥1 cm [n = 11] | ≥3 cm [n = 6] |
|---|---|---|---|
| Sessile | 4(80) | 6(55) | - |
| Pedunculated | 1(20) | 5(45) | - |
| Flat Lesion | - | - | 1(17) |
| Ulcerated | - | - | 2(33) |
| Vegetating | - | - | 3(50) |
Numbers in parentheses are percentages %.
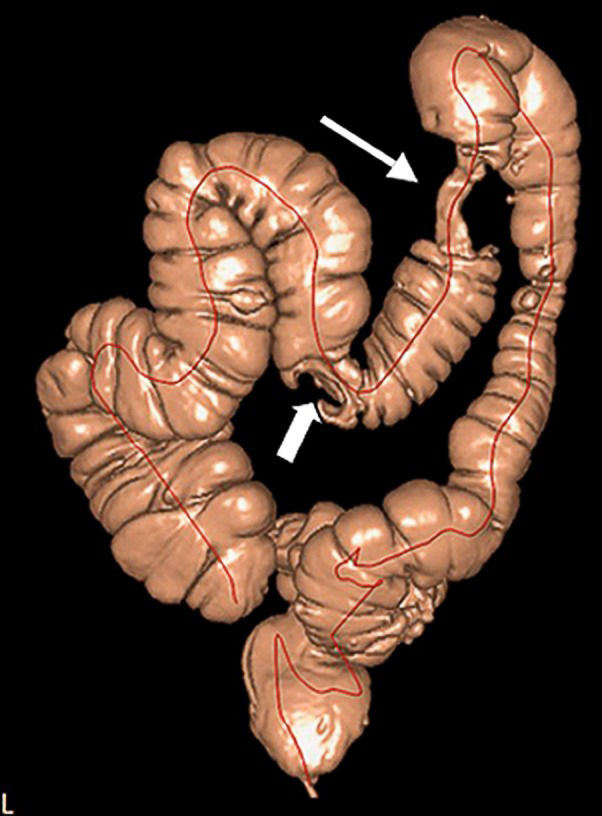
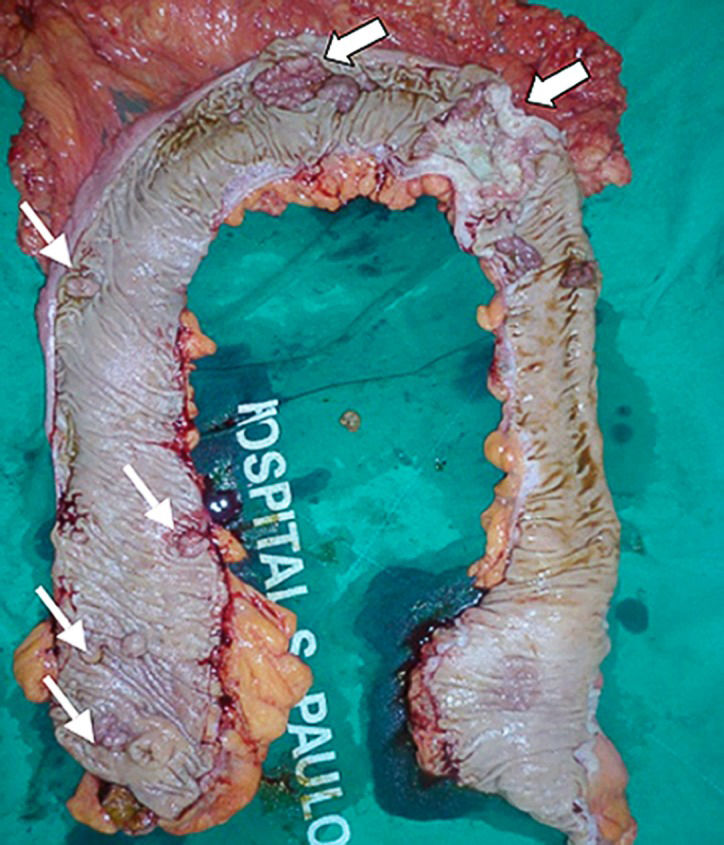
Among the 13 patients with incomplete OC due to CRC,C, CTC the lesion was identified by CTC in all cases. The data contributed to a diagnosis of a synchronous tumor in the transverse colon with extra colonic metastasis in one patient and of eight sessile polyps ≥6 mm that were non-visualized after incomplete colonoscopy in four patients. The anatomopathological analysis after a full colectomy in one of the patients identified three of the polyps as advanced adenomas with a villous component and as villous adenomas (Figures1 and 2).
Macroscopic evaluation of the total colectomy product from the same patient as shown in Figure1, a surgical specimen with synchronous tumors (large arrows) and several scattered polyps (thin arrows).
Eighty-three patients (97.6%) developed no adverse events as a consequence of the bowel preparation and only two patients (2.4%) had mild reactions, which were characterized by vomiting in one patient and palpitations after the ingestion of iodinated media contrast in another patient. Seventy-five patients (88.2%) expected a “moderate” or “great” level of discomfort and ten patients (11.8%) expected “little” discomfort before the exam. On the other hand, after the CTC exam had been performed, 83 patients (97.6%) reported only mild discomfort and 63.5% of patients experienced less discomfort than originally expected. The results showed that, for all segments, the colonic distension was not associated with the level of discomfort reported by patients (p>0.05). When asked about their examination preference, 85% of the 78 patients submitted to both exams preferred the CTC.
Bowel preparation and overall evaluationSeventy-five patients (88.2%) underwent a complete preparation and ten (11.8%) an incomplete preparation due to inadequate intake of iodinated contrast in eight patients and of Muvinlax® in two patients. On average, for each colonic segment, the preparation used achieved 94.1% of the colonic segments with no fecal residue and 71.7% of segments with <25% residual liquid; 71.8% of patients had an excellent distension; and the confidence level in the overall diagnoses was rated as 86% (Table3). The physicians' confidence in their interpretation of CTC was strongly correlated with the amounts of residual fluid, fecal residue and colonic distension in the respective colonic segments (p≤0.001 for each). Therefore, a greater distension combined with less residual fluid and fecal residue promoted greater confidence in the interpretation of the CTC exam. Regarding the overall evaluation by radiologists, 89% of patients had an excellent bowel preparation, 6.4% an inadequate preparation and 4.6% a partial preparation. The average effective radiation dose in the eighty-five CTC examinations was 7.8 mSv (3.8-12.0 mSv; DP = ±2.0).
-Quality percentages calculated in preparation and confidence in the diagnostic evaluation of each colonic segment.
| COLONIC SEGMENT | PARAMETER | |||
|---|---|---|---|---|
| Cecum | Colonic distention | Residual marked | Residual fluid | Confidence |
| a | 9.4% | 91.7% | 7.1% | 11.7% |
| b | 16.5% | 2.4% | 70.5% | 3.5% |
| c | 74.1% | 2.4% | 16.5% | 84.8% |
| d | ——— | 3.5% | 5.9% | ——— |
| Ascending colon | ||||
| a | 2.4% | 89.4% | 12.9% | 11.7% |
| b | 25.9% | 2.4% | 68.2% | 2.3% |
| c | 71.7% | 3.5% | 16.5% | 86% |
| d | ——— | 4.7% | 2.4% | ——— |
| Transverse colon | ||||
| a | 1.2% | 88.2% | 11.8% | 11.7% |
| b | 30.6% | 2.4% | 71.8% | 2.3% |
| c | 68.2% | 4.7% | 12.9% | 86% |
| d | ——— | 4.7% | 3.5% | ——— |
| Descending colon | ||||
| a | 8.2% | 88.2% | 16.5% | 10.5% |
| b | 25.9% | 5.9% | 76.4% | 3.5% |
| c | 65.9% | 3.5% | 4.7% | 86% |
| d | ——— | 2.4% | 2.4% | ——— |
| Sigmoid colon | ||||
| a | 13% | 91.7% | 23.5% | 10.5% |
| b | 18.8% | 2.4% | 71.7% | 3.5% |
| c | 68.2% | 3.5% | 2.4% | 86% |
| d | ——— | 2.4% | 2.4% | ——— |
| Rectum | ||||
| a | 8.2% | 94.1% | 23.5% | 10.5% |
| b | 20.0% | ——— | 71.7% | 3.5% |
| c | 71.8% | 2.4% | 2.4% | 85.8% |
| d | ——— | 3.5% | 2.4% | ——— |
| On average | 71.8% | 94.1% | 71.7% | 86% |
Colonic distention: a) non-distended segment. b) proper distention. and c) excellent distention. Residual marked: a) no fecal residue. b) only residues <5 mm. c) residues with one to three particles ≥5 mm. d) residues with more than three particles ≥5 mm. Residual fluid: a) absent. b) occupied <25% of the intestinal lumen. c) occupied between 25% and 50% of the lumen. d) occupied>50% of the intestinal lumen. Confidence: a) not confident. b) less confident. c) confident.
In recent decades, CTC/virtual colonoscopy has emerged as an alternative to OC, not only for the screening of CRC 1-2 but also as an alternative test for investigating symptomatic patients or those at high risk of developing CRC. Its speed, efficiency (usually lasting less than ten minutes), reproducibility, high level of accuracy, high level of toleration by patients, minimal invasiveness and cost-effectiveness all contribute to the superiority of CTC compared to no screening. For these reasons, the development of new CTC services for the investigation of symptomatic and/or high-risk patients is highly desirable. The demand for CTC in a particular country or region is determined by several factors: a) a general demand for colonic investigation; b) OC waiting lists; c) CT scanner capacity; d) the availability of trained radiologists; and e) the unit cost per investigated patient 14,15. In our country, an analysis of these factors has indicated a demand for CTC propagation. In addition, the actual unit cost per CTC is substantially lower in some countries compared to the estimated costs used in previous cost-effectiveness analyses 15, supporting the adoption of this modality in CRC screening programs, even in the context of lower monetary resources. Furthermore, as many hospitals already have CT scanners that can perform CTC (multi-detector row scanners), the implementation of CTC requires little, if any, additional investment 16.
Although CTC has been widely accepted as a screening tool for colorectal cancer, even in the United States fewer than 20% of hospitals have adopted this service 16. The use of CTC programs at US hospitals has grown over the last 5 years, increasing from 13% in 2005 to 17% in 2008. The main factors motivating the adoption of CTC include a desire to provide an alternative screening option for elderly patients and for those with failed OC, as well as the often long wait times for OC and strong evidence supporting the use of CTC in the peer-reviewed literature 16. In Brazil, CTC scans are offered in only some private practices and scarce published data are currently available 17,18,19.
Several studies have suggested that most patients prefer CTC to OC or barium enema 5,6. These studies demonstrate a preference for CTC in 72% of patients versus OC and in 97% of patients versus barium enema 5. Similar results were observed in our study, which showed a preference for CTC in 85% of the patients. On the other hand, the prospects of sedation, unconsciousness, discomfort and not witnessing the exam were the reasons given by the six patients who preferred the OC.
CTC and OC can effectively identify the adenomatous polyps that are the precursors of CRC 6. However, these methods require the cleaning of the colon with cathartic agents to minimize or eliminate the negative effects of stool or fecal residues on the interpretation of the exam 8. Patients usually report an aversion to laxative preparations, which represents an obstacle for performing these exams and contributes to the relatively low rate of colon cancer screening 9. The ideal cathartic agent for CTC has not been standardized, but phosphor-soda, magnesium citrate and polyethylene glycol (PEG), which was used in the current study, are among the most commonly used agents. PEG is an osmotically balanced wash solution that can be used safely in most patients, unlike phosphor-soda or magnesium citrate, which are sometimes contraindicated 10. Our selected preparation with PEG was rated excellent in 89% of cases and was accepted by most patients. There was a statistically significant correlation between our level of confidence interpreting the CTC and the residual fluid, fecal residues, and distension in the respective colonic segments that reflected the efficiency of the PEG in the CTC exams performed. Inadequate (6.4%) or partial (4.6%) preparations were due to incorrect use of drugs. The preparation adopted in our study was quite safe, with only two patients experiencing self-controlled sided-effects, such as palpitations and mild vomiting, after ingesting iodinated contrast.
The benefits of CTC screening every 5 years from ages 50 to 80 far exceeded the risks inherent to the exposure to ionizing radiation 20. The American Council and ACR estimate an average recommended dose of radiation for CTC exams of approximately 7 mSv 21. In our study, the CTC exams were performed with a low-dose radiation protocol at a mean effective dose of 7.8 mSv, ranging between 3.8 mSv and 12 mSv, depending on the body types of the patients and the need to change positions to better characterize the entire colon.
That the overall accuracy for detecting polyps larger than 5 mm is above 90% in many studies 22,23 has been used to justify the selection of CTC as a first-option exam in CRC screening, as reinforced by PPVs exceeding 90% for lesions larger than 6 mm, even in high-risk patients 11,24. Our study produced similar results to those previously described, with a sensitivity and specificity above 95% for CTC after standard bowel preparation. This was likely due to the expertise of the readers, one of whom had interpreted more than 600 CTC examinations. An expert radiologist can be defined as a radiologist who has interpreted at least 500 CTC scans 25. In daily practice, greater experience with CTC is often associated with over-sensitivity of polyp detection.
The population included in our study is considered at high risk for the development of CRC. Colorectal cancer occurs in 90% of cases in subjects over 50 years of age. The mid-life risk of 5% 26 increases to 30% in high-risk patients (those with family or personal history, inflammatory disease, or polypoid or non-polypoid syndromes) 27. It is estimated that the medium prevalence of ≥6 mm polyps is equal to 13-16% and that the finding of an advanced neoplasia in polyp varies from 3.3-7.1% of patients 28. In our study group of high-risk patients, including fifty-six patients with complete OC, we found ≥6 mm polyps in 19 patients (34%); of those patients, ten (18% or 10/56) presented with advanced neoplasia (adenocarcinoma, high degree carcinoma and villous component), a slightly higher frequency than is typically seen in this group of patients. In fact, it is estimated that, among high-risk patients, 10% of polyps larger than 5 mm are advanced adenomas or carcinomas 29; 0.9% of the 6 to 9 mm polyps are adenocarcinomas; and 10% of the 10 to 20 mm polyps constitute CRC 30. The strategies used to approach high-risk patients are often similar to those for medium-risk patients but should ideally be more careful in nature. In this context, the CTC plays an important role as a method of screening for CRC, generating benefits relevant to clinical, socio-economic and even emotional issues 31.
Another factor to consider when choosing a procedure is the possibility of an incomplete OC. An incomplete OC rate (i.e., the cecum is not reached) is considered acceptable in 10% of cases in daily clinical practice and in 5% of cases for CRC screening 25. However, an incomplete OC can occur in up to 25-30% of patients, especially when infiltrative and stenotic lesions are present. In these cases, it is important to complete further evaluations of the colon. Up to 6.3% of polyps and 4.3% of advanced lesions may be missed if a full assessment of the colon is not performed 32-33. In such cases, CTC has an indisputable role. In our study, for example, CTC proved useful for the pre-operative evaluation of a patient diagnosed with left colon carcinoma and incomplete OC, finding a synchronous tumor of the transverse colon that affected the subsequent planned surgery.
The present study has some limitations. Because this prospective clinical investigation was performed amid the daily practice of a general hospital, the sample was small and heterogeneous. The preparation quality was assessed subjectively and without any comparison to the other types of preparations available and described in the literature. The patients were mostly referred by gastroenterologists, increasing the likelihood of true positive findings by CTC. Additionally, the analysis of the images by consensus and the knowledge on the part of radiologists that patients would undergo OC on the same day as the CTC may have increased the sensitivity and specificity of their approach. Many may have accordingly increased their efforts to characterize all possible lesions. Inter-observer agreement was not calculated to determine the reproducibility of CTC in the detection of colonic lesions, which could have contributed to a more comprehensive evaluation of the method at hand, although such data have been previously reported 34.
When we began this project four years ago, the CTC exam was not offered at our institution or at any other university or public hospital in our country. We specified the use of an adjusted MDCT device for these exams, recruited a radiologist with great experience from private institutions and developed a work plan with the desire of founding a CRC screening service using CTC (offering this diagnostic tool to a destitute population). In this sense, various phases of the study were planned and performed on a continuum, which helped to build the entire care process by producing multiple articles that disseminated the experience gained by the group 18,19. The work plan included: (1) the establishment of a training program for the technicians and nurses of the department; (2) the development of a protocol for bowel preparation that could be understood and accomplished by the patients without interfering in the OC exam; (3) the creation of a standard procedure to perform the CTC; (4) the notification of the gastroenterology department about the CTC exam, with the aim of recruiting them to join the study; (5) the establishment of a method for data interpretation and reporting; and (6) the creation of a hands-on training protocol for CTC data interpretation that could be incorporated into the radiology residency program. Currently, CTC training is included within the teaching program of the institution's radiology residents, providing 16 hours of annual hands-on coursework in the work setting to facilitate the better assimilation of the method, ensuring the permanent inclusion of CTC in the routine CT scans of our department.
However, in this project, we encountered a number of difficulties inherent to the construction of a new care process. Perhaps the greatest barriers were related to the inertia of the system and the lack of familiarity with the screening method on the part the majority of those involved. The persistent pro-active attitude and creativity of the group in overcoming these difficulties were crucial to the success of the project, although we still have not completed the number of exams originally planned. We are currently involved in a study seeking to establish the reasons for the limited number of exam requests and assessing the views of specialists (radiologists, clinicians and surgeons) regarding the value of CTC in our department. The feasibility of implementing the CTC program is undeniable in the setting of genuine interest and appropriate equipment availability. The low cost of the required medical devices (gloves, rectal probe and anesthetic gel) combined with the speed (approximately 10 min) and simplicity of the procedure certainly promote adherence to the CTC examination procedure. In addition, we interfered minimally in the department's routine.
It is important to observe that the costs of the examination were minimized by using manual insufflation with ambient air (which was met with good acceptance by patients), thereby avoiding the expenses inherent to the use of mechanical CO2 insufflators. Further, by not using endovenous antispasmodics, we reduced the costs, made the exam minimally invasive and maintained similar acceptance results with those of other studies 5,8. For a CTC examination performed with iodinated contrast tagging and manual insufflation, the estimated costs (medical devices, drugs and contrast media), including laxative agents taken directly by the patients, were approximately US$ 14.0 per examination. This variable cost per CTC exam is very competitive when considering alternative investigative modalities and the fact that other expensive equipment-investment costs, such as the CT scanner itself, can be minimized by the large quantity of CT exams performed for multiple indications, amounting in our practice to approximately 12,000-15,000 exams per year, per piece of equipment. On the other hand, we did not evaluate costs associated with human resources (considering CTC reading and reporting time) or other variables, such as poor bowel cleansing, inadequate tagging, artifacts and poor colon distension. All of these factors may directly or indirectly increase the costs of the examination and should be investigated rigorously. In short, we can claim that the CTC exam is regularly available for those patients treated at our institution and candidates for the screening of CRC.
In conclusion, it was possible to include the CTC among the routine exams performed at a university hospital and to focus on the patients serviced in the public health system at a level of safety, acceptance and effectiveness similar to international standards. In most cases, patients preferred the CTC over the optical colonoscopy. Bowel preparation with PEG provides excellent results and is well accepted by patients. CTC is a fundamental tool in the evaluation of the colon in patients experiencing incomplete optical colonoscopy, especially when the presence of CRC prevents the progression of the device. These data could be beneficial to public health policymakers and managers, as they consider both a variety of strategies for increasing CRC screening rates and the role that CTC should play in the investigation of high-risk and symptomatic patients.
AUTHOR CONTRIBUTIONSvon Atzingen AC conceived and designed the study, was responsible for literature research, clinical examinations, experiments/data analysis, statistical analysis, preparation and editing of the manuscript. Tiferes DA conceived and designed the study, was responsible for clinical examinations, experiments/data analysis and statistical analysis. Deak E was responsible for clinical examinations. Matos D conceived and designed the study, was responsible for clinical examinations and data analysis. D′Ippolito G conceived and designed the study, was responsible for the manuscript preparation, clinical examinations, experiments/data analysis, manuscript editing and statistical analysis.
No potential conflict of interest was reported.