Hyponatremia is the most common electrolyte disorder following intracranial surgery. Its aetiology is multifactorial. We present a case of a patient taken to microvascular decompression (Janetta surgery) for the treatment of trigeminal neuralgia who developed a symptomatic magnification of basal hyponatremia in the immediate post-operative period. Cerebral salt wasting syndrome was diagnosed. The management of this condition poses a challenge for physicians involved in postoperative neurosurgical care.
La hiponatremia es el trastorno electrolítico más frecuente después de la cirugía intracraneal. Su etiología es multifactorial. A continuación presentamos un caso de un paciente sometido a una descompresión microvascular (cirugía de Janetta) como tratamiento de la neuralgia del trigémino que en el postoperatorio inmediato desarrolló una magnificación sintomática de su hiponatremia basal. Se diagnosticó un síndrome pierde sal cuyo manejo supone un reto para los médicos implicados en los cuidados neuroquirúrgicos postoperatorios.
Fluid and electrolyte disorders are one of the complications of head injury and neurosurgical procedures, hyponatremia being the most common. Except for excess fluid or drug administration, the most frequent cause of polyuria-associated hyponatremia is cerebral salt wasting syndrome (CSWS).
Clinical caseA 58-year-old patient with trigeminal neuralgia scheduled for microvascular sub-occipital decompression craniotomy, with a history of multiple sclerosis (MS), prior thermocoagulation procedures and home treatment with oxcarbazepine, tryptizol, tapentadol and transcutaneous fentanyl. The surgical procedure was performed under general anaesthesia with the patient in supine recumbent position and cervical rotation for a retromastoid approach. No osmodiuretics were required. The patient was taken to the recovery unit for postoperative neurological monitoring. While in the unit, the patient developed intense headache, difficult-to-control nausea, muscle cramps, and a tendency to polyuria (3ml/kg). The neurosurgeon did not find the need for an urgent CT scan. Follow-up biochemistry tests were requested, with the finding of plasma sodium at 117mEqL−1 (pre-anaesthesia consultation 130mEqL−1 and urine sodium at 170mEqL−1). Volume replacement was initiated using isotonic saline solution, and the fluid and electrolyte imbalance was addressed with 3% hypertonic saline solution. Twenty-four hours later, plasma sodium was at 128mEq−1 and diuresis was at 150mlh−1, with total remission of the clinical picture.
DiscussionTrigeminal neuralgia (TN) consists of electrical paroxysmal discharges in the trigeminal nerve innervation area.1 It may present in isolated form or as a result of major neurological diseases such as MS or benign posterior fossa tumours.1 MS patients have a 20 times higher risk2 of developing TN.1 While the annual incidence of TN in the general population is 0.015%, it is 1.9-4.9% in MS.1 The most probable hypothesis is the irritation caused by the superior cerebellar artery on the root of the Vth cranial nerve.3,4 In cases of TN in MS, there is also a lesion of the trigeminal presynaptic afferent pathway due to the presence of a demyelinating plaque.1,5,6 At present, there are four potential therapies,7 including pharmacological treatment, radiofrequency, thermocoagulation, glycerol or balloon percutaneous rhizotomy, or microvascular decompression (Jannetta procedure).3 This latter technique involves placing a layer of autologous or artificial material between the nerve and the impinging vessel through a retromastoid craniotomy.3
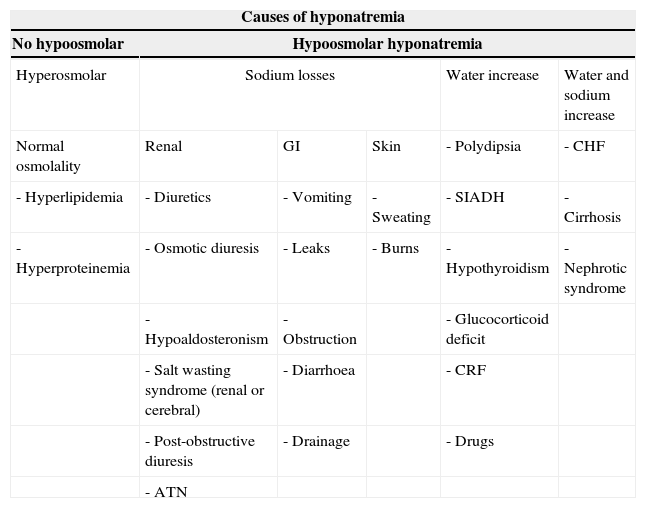
The picture of severe symptomatic hyponatremia that developed in this patient may be explained on the basis of multiple factors that need to be analysed and identified correctly. Hyponatremia is the most common electrolyte disorder in hospitalized patients.8 It is defined as sodium plasma levels below 135mmolL−1. The severity of the clinical picture depends on whether it is acute (less than 48hours) or chronic (more than 48h) and on the intensity (severe if 115mmolL−1), the aetiology being variable (Table 1). The most frequent symptoms are somnolence, apathy, anorexia, muscle cramps, headache, nausea, vomiting and stupor, which may progress to Cheyne–Stokes breathing, seizures, coma and death. Perioperatively, diuretics, ACE inhibitors and carbamazepine,9 normally used in TN, are the most frequent pharmacological causes of hyponatremia. Oxcarbazepine9 used as monotherapy or in combination with other drugs, may lead to what is known as oxcarbazepine-induced hyponatremia, a dose dependent and usually asymptomatic condition with an incidence ranging from 23 to 73%.9 Aetiological mechanisms are varied, but the most commonly accepted hypothesis is the inadequate release and/or greater sensitivity of tubular vasopressin10 as well as increased water with secondary sodium loss. The picture of oxcarbazepine-induced hyponatremia is usually mild and asymptomatic, secondary to a process of neuronal hyperhydration,11 and severity is associated with how fast the absolute drop in plasma sodium occurs, with numbers under 125mmolL−1 being clinically significant. The association between the use of carbamazepine and its derivatives and the inappropriate secretion of antidiuretic hormone (SIADH) has been widely described in the literature.12
Causes of hyponatremia (ATN: acute tubular necrosis; SIADH: inappropriate ADH secretion; CRF: chronic renal failure; CHF: congestive heart failure).
| Causes of hyponatremia | |||||
|---|---|---|---|---|---|
| No hypoosmolar | Hypoosmolar hyponatremia | ||||
| Hyperosmolar | Sodium losses | Water increase | Water and sodium increase | ||
| Normal osmolality | Renal | GI | Skin | - Polydipsia | - CHF |
| - Hyperlipidemia | - Diuretics | - Vomiting | - Sweating | - SIADH | - Cirrhosis |
| - Hyperproteinemia | - Osmotic diuresis | - Leaks | - Burns | - Hypothyroidism | - Nephrotic syndrome |
| - Hypoaldosteronism | - Obstruction | - Glucocorticoid deficit | |||
| - Salt wasting syndrome (renal or cerebral) | - Diarrhoea | - CRF | |||
| - Post-obstructive diuresis | - Drainage | - Drugs | |||
| - ATN | |||||
Drugs related with the development of hyponatremia: Diuretics (especially thiazides), antipsychotics (phenothiazine and haloperidol), antidepressants (SSRIs, tricyclic antidepressants and MAOIs), antiepileptic drugs (lamotrigine, carbamazepine, oxcarbazepine, valproic acid), antibiotics, antiarrhythmic drugs (amiodarone), antihypertensive drugs (ACE inhibitors, ARA II, amlodipine), antineoplastic agents and others (NSAIDs, PPIs, etc.).
There are very limited data in the literature on severe symptomatic oxcarbazepine-induced hyponatremia.9 It may be fatal when associated with other frequent complications found in neurosurgical patients, including polyuria and hyponatremia.
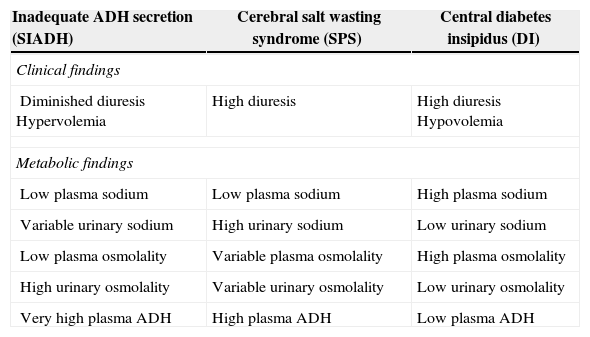
The two conditions most frequently associated with polyuria in the neurosurgical patient are diabetes insipidus (DI) and salt wasting syndrome (SWS), while those associated with hyponatremia are SWS and SIADH13, both of which determine a picture of hypotonic hyponatremia with elevated natriuresis8. Both DI and SWS share some clinical findings with SIADH such as hyponatremia or a history of brain injury, whereas other concomitant findings help establish a clear difference (Table 2), as is the case with hypovolemia, excess uresis and significant natriuresis, with normal anti-diuretic hormone levels.14
Clinical and metabolic differential diagnosis between central diabetes insipidus (DI), inadequate ADH secretion (SIADH) and salt wasting syndrome (SWS).
| Inadequate ADH secretion (SIADH) | Cerebral salt wasting syndrome (SPS) | Central diabetes insipidus (DI) |
|---|---|---|
| Clinical findings | ||
| Diminished diuresis Hypervolemia | High diuresis | High diuresis Hypovolemia |
| Metabolic findings | ||
| Low plasma sodium | Low plasma sodium | High plasma sodium |
| Variable urinary sodium | High urinary sodium | Low urinary sodium |
| Low plasma osmolality | Variable plasma osmolality | High plasma osmolality |
| High urinary osmolality | Variable urinary osmolality | Low urinary osmolality |
| Very high plasma ADH | High plasma ADH | Low plasma ADH |
The distinction between the three clinical pictures is critical because they each require different management and need to be dealt with quickly by means of fluid replacement in DI and SWS, and fluid restriction in SIADH. On the other hand, in SWS, DI and SIADH sodium, vasopressin and diuretics must be given, respectively.13 Analytical determinations confirmed our suspicion of SWS: high hourly diuresis, low plasma sodium, high urinary sodium and low plasma osmolality which exacerbated the underlying picture of oxcarbazepine-induced hyponatremia (preoperative plasma sodium of 130mEqL−1), which progressed to severe symptomatic subsidiary hyponatremia following ionic correction.
The salt wasting syndrome was initially described by Peters et al. in 1950.13 The mechanism by which a cerebral condition causes SWS is not well known,8 although several hypotheses have been described, such as lower adrenocorticotropic hormone secretion.13 The most accepted mechanism at the present time is excess release of atrial natriuretic peptide (ANP) and brain natriuretic peptide (BNP)15,16 which directly inhibit sodium reabsorption in the proximal tubule and increase natriuresis indirectly through the inhibition of the renin–angiotensin–aldosterone axis,8 decreasing effective vascular volume and sympathetic tone.8,13 Primarily produced in the cardiac ventricles and the hypothalamus, the BNP is most frequently implicated in the development of SWS.8 This condition presents as a clinical picture consisting of polyuria and polydipsia with hypernatriuria, hypernatremia, diminished plasma osmolality and variable urine osmolality.13 The difference between SWS and SIADH, both of which determine a hyponatremic state,16 is the presence of lower extracellular volume and polyuria in SWS, while extracellular volume is increased and there is oliguria in SIADH. The treatment of SWS is replacement of intravascular volume using isotonic saline solution, slow oral or parenteral sodium replacement on the basis of the severity of the clinical picture (no more than 8-10mEqL−1 in 24h) in order to avoid central pontine myelinolysis, and the administration of fludrocortisone which may reduce natriuresis because of its potential mineralocorticoid effect.8
Hyponatremia is the most common fluid and electrolyte disorder in neurosurgical patients, SWS being the most frequent in this subgroup.17
It is critical to determine the aetiology and institute early treatment in order to avoid permanent neurological impairment. In many cases, the aetiology of this disorder is multifactorial and it is influenced by previous pharmacological treatment such as diuretics and anticonvulsants, as well as by syndromes accompanied by hyponatremia, SWS and SIADH. Considering that management is completely different, misidentification of the entity responsible for this disorder may give rise to catastrophic consequences.
Patient perspectiveThe patient perceived the anaesthetic management as the most beneficial, given the nature of the surgical intervention and the associated anaesthetic risks.
Informed consentThe informed consent was obtained.
FundingOur work has not received any funding.
Conflict of interestThere are no conflicts of interest.
Ethics committeeWe received the approval of the ethics committee.
Data identificationPatient data have been masked.
Please cite this article as: Guerrero-Domínguez R, González-González G, Acosta-Martínez J, Rubio-Romero R, Jiménez I. Síndrome pierde sal en el postoperatorio de cirugía de fosa posterior: reporte de caso. Rev Colomb Anestesiol. 2015;43:61–64.