Mentioning microcirculation and endothelial dysfunction to explain the pathophysiology of diseases whose relationship was not well understood is a recent phenomenon. Microcirculation is not only compromised by disease but can be altered by conditions that the anesthesiologist faces (agents and anesthetic techniques). There is significant and increasing evidence that anesthetic agents may alter it. The importance? In a state of hypoperfusion, it can be worsened by other factors (mechanical ventilation, vasoactive medications, sedatives, opioids). In shock's late stage, the support to tissue perfusion given by peripheral circulation is weak and disappears. Therefore, is it beneficial to direct targeted therapies only toward macrovascular goals? Methods for identifying early alteration and direct therapies for restoration are important. The clinical evaluation is rapid and reproducible, and measuring body temperature determines alteration indirectly. There are other methods to determine microcirculation objectively: nowadays, optical evaluation techniques using polarized orthogonal spectral light and sidestream dark-field are the best approach. In hemorrhagic shock the degree of organ dysfunction is determined by microvasculature's alteration. Compensatory mechanisms exist for this purpose, making its measurement and use in perioperative period important. Strategies have been studied to improve tissue perfusion (recruitment of microcirculation). The recentness of the study of microcirculation calls its usefulness into question. It is necessary to determine the clinical impact through controlled clinical trials with protocols on resuscitation strategy, which can complement the current perioperative anesthetic practice.
Es reciente la mención de la microcirculación y disfunción endotelial para explicar la fisiopatología de padecimientos de los cuales no se entendía su interrelación. La microcirculación no solo está comprometida en enfermedad sino que puede alterarse por condiciones a las que se enfrenta el anestesiólogo (agentes y técnicas anestésicas). Existe evidencia importante y creciente de que agentes anestésicos pueden alterarla; ¿su importancia?: en hipoperfusión puede empeorarse por otros factores (ventilación mecánica, vasoactivos, sedantes, opioides). En fase tardía del choque la participación de la circulación periférica soportando la perfusión tisular es débil hasta desaparecer; entonces: ¿es benéfico encaminar las terapias dirigidas por metas sólo macrovasculares? Se hacen importantes métodos que identifiquen su alteración tempranamente y encaminar terapias para su restauración: la evaluación clínica es rápida y reproducible; la medición de temperatura corporal determina indirectamente su alteración; existen otros métodos de evaluación de la microcirculación más objetivos: hoy en día la evaluación óptica mediante técnica con luz polarizada ortogonal espectral y campo oscuro lateral son la mejor aproximación. En choque hemorrágico es la alteración de la microvasculatura la que determina el grado de disfunción multiorgánica; para ello existen mecanismos compensatorios, lo cual reviste la importancia de su medición perioperatoria y uso en anestesia. Se han estudiado estrategias que mejoran la perfusión tisular (reclutamiento de la microcirculación). Por ser reciente su estudio se controvierte su utilidad; es necesario determinar el impacto clínico mediante ensayos clínicos controlados en protocolos de estrategia de reanimación, lo cual puede complementar la práctica anestésica perioperatoria actual.
Recently in medicine, microcirculation and endothelial dysfunction have been mentioned to explain the physiopathology of conditions whose interrelationship was not previously understood. In the complex, integrated response, systems conforming a proinflammatory group and a prothrombotic group interact; the endothelium and microcirculation are the mediators of this interaction. When it is altered, it leads to collapse.1 Microcirculation is compromised in conditions that anesthesiologists face frequently. There is important and growing evidence that anesthetic agents can alter it.2 The advance in imaging techniques allows for its evaluation at the patient's bedside. Since these conditions are associated with a poor prognosis, regardless of the overall hemodynamic variables, evaluating microcirculation is important in anesthesiology to understand how different anesthetic techniques impact microcirculation and its usefulness as a possible perioperative monitor in critical patients.3
Historical perspectiveKnowledge of blood circulation began in ancient Egypt and Greece. Galen of Pergamon (2nd century BCE) proposed that blood was the “vital spirit” that is exhaled by the lungs. Ibn al Nafis (1210–1288) describes pulmonary circulation, stating that between the pulmonary artery and the pulmonary vein “there may be imperceptible passageways”. This is perhaps the first mention of the notion of microcirculation. The idea of the heart as a pump came in 1628 with Sir William Harvey.4
Current knowledgeHypoperfusion is the insufficient transport of nutrients and oxygen necessary for normal cell activity. Microcirculation makes up more than 90% of the endothelium, and is composed of small vessels (<100μm in diameter), arterial capillaries and venules, forming a vascular network that regulates the distribution of blood flow to each organ, exchanging gases, nutrients and products of cell catabolism. It is also involved in the interaction of leukocytes, platelets, and plasmatic components.1
Its importance? Hypoperfusion can worsen do to other factors such as mechanical ventilation, vasoactive drugs, sedatives, and opioids used regularly in anesthetic practice and in critical patients. Some tissues do not have the capacity to self-regulate blood flow, being dependent on mechanisms of sympathetic vasoconstriction. In the initial phase of shock, the compensatory mechanism is vasoconstriction through neurohumoral response; in the late phase, the participation of peripheral circulation supporting tissue perfusion is weak to the point of disappearing.5 From here the question rises, is it beneficial to carry out only macrovascular-oriented goal-directed therapy (GDT)?
Assessment and monitoringMethods that allow for the early identification of alterations in the microvasculature, and to put therapies into effect for its maintenance and recuperation, are important.
Clinical assessment is quick and reproducible. Mottled skin for more than 6h are after resuscitation is a predictor of mortality within 14 days in cases of septic shock.6 Capillary refill time greater than 5s is a predictor of greater multi-organ dysfunction (MOD) and hyperlactatemia.7 Lima et al., in a study in intensive care units, found a correlation index between qualifiers of 0.85 (95% CI 0.82–0.86), attributing a prognostic value to this sign.8
The measurement of body temperature indirectly determines the alteration of microcirculation through the delta of central-skin temperature (dTc-s) or forearm-hand; dTc-s, normally 3–7°C, increases because the central temperature is maintained at the cost of peripheral circulation to ensure perfusion to vital organs. The Tskinn-diff is more viable since both zones are exposed to the same operating room temperature: 0°C shows initial vasoconstriction, −4°C shows severe vasoconstriction.5
More objective methods for assessing microcirculation have been developed: tonometry, indocyanine green elimination, Laser-Doppler flowmetry, spectrophotometry, peripheral perfusion index derived from the photoelectric plethysmographic signal from pulsoximetry, infrared spectroscopy with greater tissue penetrance5; intravital videomiscroscopy and videocapillaroscopy of the nail bed.9
Laser-Doppler flowmetry measures the flow in a variable volume of tissue, but is not capable of detecting individual vessels, allowing only for an averaged estimate of tissue perfusion, without offering information on morphology, type of vessel, direction of flow, and heterogeneity of the perfusion.9
Intravital videomicroscopy has been considered a classic technique, offering the majority of information obtained at an experimental level, but with little applicability in human beings since it requires large-scale microscopes on tissue pretreated with fluorescent stains. Videocapillaroscopy of the nail bed was the first technique to be used at the patient's bedside. It consists in viewing with an ordinary microscope the border between the cuticle and the nail using a quench medium. It is most useful in studying alterations in microcirculation in chronic diseases like diabetes, vasculitis, and rheumatologic disorders. Its use in patients in a severe condition is limited due to the sensitivity of the area under the nail bed due to factors that alter vascular tone.9
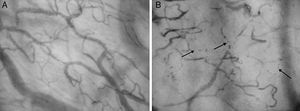
Today, optical assessment with the technique of orthogonal polarized spectral (OPS) light and sidestream dark-field (SDF) are seen to be the best approach.5 OPS is based in the fact that the light reflected by the surface is excluded when it passes through an analyzer located at a right angle to the light source, producing the image of the non-polarized light reflected. The light emitted similarly absorbed by oxy- and deoxyhemoglobin, and so, through backlighting, the red blood cells are captured since they are the ones that absorb the light.9 SDF (Fig. 1) is a technology developed to assess microcirculation non-invasively using a portable videomicroscope. It is based on the same principle for acquiring images as the OPS, but the main difference is the source of light used (LED) in the lateral illumination of the dark-field. This light is absorbed by hemoglobin contained in erythrocytes, independent of their state of oxygenation. In this way, the red blood cells flowing in the microcirculation can be viewed through contrast. These images obtained through SDF are clearer and have better contrast compared with those obtained through OPS. Their advantage is also the possibility of evaluating multiple parameters (density, flow, heterogeneity) and differentiating according to the size of the vessel. This technique is validated and should be used on tissues that are not sensitive to heat or cold (usually the tongue, nail, eyelid, ileostomy, colostomy, rectal or vaginal mucosas) (Fig. 2).9 In general, these two methods provide a direct view of the microcirculation through the videomicroscope; they are not invasive, and can be used in the sublingual region, in ileostomies or colostomies, and rectally. The lack of improvement in blood flow after resuscitation is associated with a greater risk of morbi-mortality. Vincent evaluated the effects of GDT on sublingual microcirculation in sepsis patients in which early increases in flow are associated with lower severity of MOD and demonstrates its usefulness for monitoring in sepsis, congestive heart failure, and non-hospital post-cardiopulmonary resuscitation syndrome.5 Usually, at least three videos (and up to five) of twenty seconds each are taken, mainly of both sides of the frenulum of the tongue since this is easily accessed, has an embryonic origin in common with the intestine and, for this reason, exhibits a good tonometric correlation with gastric PCO2.9
Sidestream dark-field (SDF) system: system for use as a hand microscope in the study of microcirculation at the patient's bedside in real time. Consists of a guide-light surrounded by green light emitting diodes (530nm) that penetrate the tissue, illuminating the microcirculation. The green light is absorbed by the hemoglobin of the red blood cells, and a magnifying glass projects the image on a video camera (Reproduced with permission from Dr. Gustavo Adolfo Ospina Tascón).
Sublingual microcirculation in a health patient and a patient in septic shock through SDF. A. Sublingual microcirculation in a health patient through SDF. B. Sublingual microcirculation in a patient with septic shock, with reduction in capillary density, heterogeneity of flow (detained and intermittent flow) at the level of microcirculation (Reproduced with permission from Dr. Gustavo Adolfo Ospina Tascón).
In hemorrhagic shock, it is the alteration of the microvasculature which determines the degree of MOD. In compensation, flow is redistributed in accordance with arteriolar and capillary resistance, rheological factors, and the tissue demand for oxygen. “Conformity or cell hibernation” occurs, in which microvascular units with reduced flow adjust their function and energy use to prevent hypoxia. There is control of arteriolar tone and of the area of oxygen exchange, dependent on O2 extraction, capillary recruitment, and rheological factors.5 The reduction of capillary flow, the velocity of erythrocytes, and the capillary density have prognostic value, are associated with the cardiac index and O2 delivery, and are the reason for which some propose fluid therapy associated with transfusion (though not solely) as the best option for improving microcirculation. Nevertheless, the effect of transfusion in this context is variable.2 Some studies exist, such as that of Damiani et al. in Italy, that show that the transfusion of old red blood cells is associated with an increase in free hemoglobin in the plasma of septic patients, which in turn is associated with a reduction in microvascular density.10
In anesthesiaIt is also useful to approach microcirculation in patients that anesthesiologists face, since microcirculation is not only compromised by their conditions but also through the action of anesthetic agents and techniques.2
Intravenous anesthetic agents such as thiopental and ketamine promote vasodilation through the inhibition of L-type calcium channels, etomidate does the same through the production of prostaglandins, and propofol, in addition to inhibiting calcium channels, has an anti-inflammatory effect to preserve hepatosplachnic blood flow and increase nitric oxide and IL-10. Nevertheless, it reduced capillary density by 9% and capillary perfusion by 16%. Volatile agents like desflurane, promote greater intestinal blood flow, and maintain hepatic and intestinal blood flow in balance with the O2 demand while not altering renal flow. Sevoflurane promotes a reduction in cardiac work.2
In pathological conditions, these effects change. In cases of hemorrhaging, a greater degree of constriction of the arterioles, capillaries, and mesenteric venules was observed under anesthesia with propofol/fentanyl when compared to thiopental and ketamine. In sepsis, propofol altered the autonomic regulation of cardiovascular function during endotoxemia, this effect being dependent on dose.2
Thoracic peridural anesthesia improves cardiac and gastrointestinal blood flow through the interruption of sympathetic activity and dose-dependent mesenteric venodilation, and it is related to the length of the block. In splachnic microcirculation, the results are conflicting. Lumbar peridural anesthesia causes vein constriction due to an increase in the sympathetic activity in the splachnic bed.2 During cardiopulmonary bypass, inflammatory response is activated due to the contact between the blood and artificial surfaces, the injury from ischemia-reperfusion derived from the clamping of the aorta. Inflammatory response may also derive from endotoxemia when the intestinal barrier is damaged. Splachnic blood flow does not diminish under hypothermia during bypass, while other studies show a reduction of 19%. Sublingual microcirculation reduces capillary density by 10% upon initiation of the bypass, and it is restored when the bypass is discontinued. Sevoflurane behaves as a cardioprotective and anti-inflammatory agent in this environment.2
Recruitment of microcirculationThese are strategies that improve tissue perfusion: open occluded vessels and keep them in this state, and avoid heterogeneity in the flow.
- •
Hydrocortisone: subtle improvement but consistent improvement one hour after septic shock. The mechanism responsible is still not elucidated.11
- •
Nitroglycerine: Spronk et al. found improvement in arterial pressure with 0.5mg bolus+infusion at 2mg/h. Organ function in survivors that received this treatment was better than in those who did not receive it. The results are contradictory because in other studies no benefit was found and there was even a tendency to increase mortality.12
- •
Vasopressors: during cardiopulmonary bypass, these agents can be deleterious in excess. Noradrenaline showed no improvement in sublingual microcirculation, anion gap, delta pCO2 or O2. Phenylephrine can reduce blood flow in sublingual microcirculation.13
- •
Inotropic drugs: dobutamine at 5μg/kg/m for two hours showed improvement in microcirculation, with changes independent of hemodynamic variables. Levosimendan prevents the reduction of O2 transport and acidosis of the intestinal mucosa in experimental sepsis models.14
- •
Intravenous liquids: the anesthesiologist should identify and maintain the intravascular volume that guarantees an adequate tissue perfusion and relationship between oxygen supply and consumption. In septic patients in which this is not achieved, it will determine splachnic hypoperfusion and hypoxia that can imply postoperative complications. There is an association between the reduction in microvascular blood flow and anastomotic leaking. Hiltebrand et al. show that GDT to achieve SvmO2 greater than 60% with colloids improves intestinal microcirculation and the O2 pressure in tissues. It is not so with crystalloids.15 Ospina-Tascon et al. studied the effects of early or late fluid therapy with Ringer's lactate solution or 4% albumin; the perfusion of sublingual microcirculation increase only in the early phase (24h), and the effect was independent of macrohemodynamic variables and the type of solution used.3 The use of hydroxyethyl starch (HES) 130/0.04 improves the resuscitation of microcirculation.16 Nevertheless, Anders et al. published a randomized clinical trial in which resuscitation fluids, 6% hydroxyethyl starch 130/0.4 (HES) or Ringer's acetate were compared in 804 patients with severe sepsis in the ICU. Patients treated with HES had greater mortality after 90 days, presenting with kidney failure and severe hemorrhaging more frequently with significant results.17
- •
Red blood cell transfusion: its effect is variable; Sakr et al., with a sample of 35 patients with severe sepsis requiring a transfusion, show that microvascular perfusion did not change in those with no alteration in the base capillary perfusion, but that it may improve in those who present with altered base capillary perfusion.18 Some studies have described an improvement in microcirculatory perfusion in patients with sepsis and serious basal alterations.9 In heart surgery, the availability of hemoglobin and SO2 improves due to greater functional capillary density and a reduction in diffusion distances. Transfusions of non-leukoreduced red blood cells and of cells that were not stored for more than three weeks are effective in surgical patients due to the increase in perfused microvessels.18 However, the threshold for transfusion is debated, though currently liberal therapy tends to be avoided; perioperative anemia in the elderly population is associated with adverse events. Nonetheless, it results in an increase in transfusions that can also have collateral effects. Low levels of hemoglobin in young patients do not reduce the oxygenation of subcutaneous tissue (this leads us to think of reducing the transfusion threshold in these populations).19 Another aspect to take into account is the age of the red blood cells to be transfused: Risbano et al. in their study demonstrate that with cells infused after 6 weeks of storage (the cold storage limit approved by the FDA), endothelial function deteriorates because of a reduction in the capacity for response to acetylcholine.20
- •
Drotrecogin: De Backer et al, in patients with severe sepsis that received activated protein C, found that the perfused capillaries increased in treated group, but not in the control group; microvascular perfusion diminished temporarily at the end of the infusion,21 due to lower adhesion of leukocytes and platelets, preservation of the glycocalyx, and greater vascular reactivity.22 Its use in current practice is debated after the review by Martí-Carvajal et al. in Cochrane 2012. Here, the author challenges the evidence since it seems to be associated with higher rates of bleeding.23
Controversies are diverse in terms of assessment, monitoring and restoration of microcirculation, as well as feasibility and ease of integration to anesthetic monitoring. The interpretation is operator-dependent. Costs limit routine use, just like the fact that the goals and interventions that act selectively on microcirculation have not been validated on a large scale. Nevertheless, assessing microcirculation is ever more important: microcirculation is compromised in conditions that anesthesiologists face and anesthetics can alter it. Vigilance complementary to the current methods of perioperative monitoring may be valuable, since overall variables like heart rate, arterial pressure, and pulsoximetry may not change in early stages of critical pathologies. Thus complementary vigilance may offer anesthesiologists greater information and tools, which may be important markers of prognosis and severity.
ConclusionsThe assessment and restoration of microcirculation is important because of its alteration in adult and pediatric critical patients in an early phase that is related to the prognosis in severe conditions. Assessing microcirculation at the patient's bedside is possible and gives immediate results, which allows for taking action quickly. The effects of anesthetic medications on microcirculation differ and some cannot be viewed due to macrohemodynamic changes, but it may guide the selection of anesthetic techniques and agents. The study of microcirculation opens a window to hemodynamic monitoring, identifying its dysfunction and response to the maneuvers of microcirculation recruitment, which can be initiated in emergencies, operating rooms, or intensive care units. It is necessary to determine the clinical impact through controlled clinical trials with protocols of restoration strategies that would support the results obtained up to this point from the experimental studies. This may complement current perioperative practice.
Conflicts of interestNone decalred.
FundingNone declared.
Please cite this article as: Ñáñez-Varona DP, Tróchez-Zuleta AL, Vargas-Garzón WA. Reanimando a la microcirculación en anestesia: impacto, utilidades y controversias. Rev Colomb Anestesiol. 2016;44:140–145.