One of the main characteristics of Prader Willi syndrome (PWS) is hyperphagia and obesity. This study sought to evaluate behaviours related to hyperphagia in individuals with PWS under a non-pharmacological transdisciplinary approach.
MethodsThis observational study included PWS patients under a traditional non-pharmacological nutritional approach immersed within a regular transdisciplinary treatment (RTT) and a control group of PWS individuals without RTT. All individuals were evaluated using the Hyperphagia Questionnaire for Clinical Trials (HQ-CT).
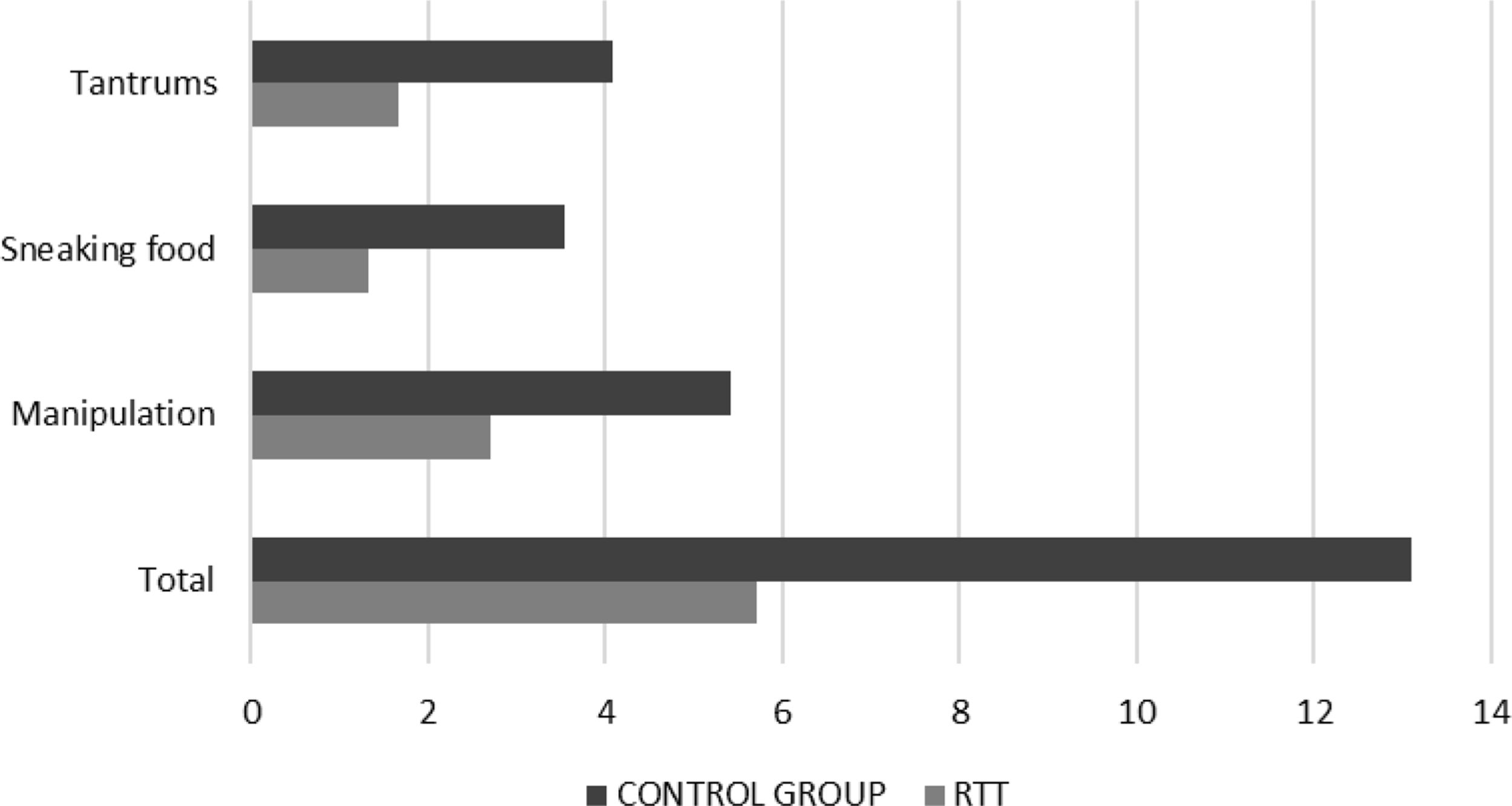
ResultsForty-three individuals were evaluated. The mean age at baseline (treatment onset) was 18.4±8.3 years in the RTT group and 19.1±6.9 years in the control group (p=0.74). Hyperphagia-related behaviours were significantly lower among those under RTT (RTT 5.7±3.7 vs control 13.1±7.5, p<0.0001). This was also identified within the three categories: arguing or manipulating to obtain food (2.71±2.1 vs 5.41±3.2, p=0.003), sneaking food (1.33±1.5 vs 3.55±3.3, p=0.007), and anger or tantrums related to food (1.67±1.8 vs 4.09±2.7, p=0.001). After a mean treatment duration of 41.0 months, the RTT group had a reduction in body mass index (baseline 38.7±17.1kg/m2 vs follow-up 29.2±9.2kg/m2; p<0.0001). A significant association between RTT duration and BMI reduction (p=0.037) was identified.
ConclusionWe observed a positive impact on behaviours related to hyperphagia and a BMI reduction in PWS individuals in a context of a non-pharmacological nutritional approach as part of an RTT.
Una de las principales características del síndrome de Prader-Willi (SPW) es la hiperfagia y la obesidad. Este estudio buscó evaluar los comportamientos relacionados con la hiperfagia en individuos con SPW bajo un enfoque transdisciplinario no farmacológico.
MétodosEste estudio observacional incluyó a pacientes con SPW bajo un enfoque nutricional no farmacológico regular inmerso en un tratamiento transdisciplinario regular (RTT) y un grupo de control de individuos con SPW sin RTT. Todos los individuos fueron evaluados mediante el Cuestionario de hiperfagia para ensayos clínicos (HQ-CT).
ResultadosSe evaluaron 43 individuos. La edad media al inicio del tratamiento (inicio del tratamiento) fue de 18,4±8,3 años en el grupo de RTT y de 19,1±6,9 años en el grupo de control (p=0,74). Los comportamientos relacionados con la hiperfagia fueron significativamente menores entre los que recibieron RTT (RTT 5,7±3,7 vs. control 13,1±7,5; p<0,0001). Esto también se identificó dentro de las tres categorías: discutir o manipular para obtener comida (2,71±2,1 vs. 5,41±3,2; p=0,003), robo de comida (1,33±1,5 vs. 3,55±3,3; p=0,007) e ira o berrinches relacionadas con la comida (1,67±1,8 vs. 4,09±2,7; p=0,001). Después de una duración media del tratamiento de 41,0 meses, el grupo RTT tuvo una reducción en el índice de masa corporal (valor inicial 38,7±17,1kg/m2 vs. el seguimiento 29,2±9,2kg/m2; p<0,0001). Se identificó una asociación significativa entre la duración del RTT y la reducción del índice de masa corporal (IMC) (p=0,037).
ConclusiónObservamos un impacto positivo en los comportamientos relacionados con la hiperfagia y una reducción del IMC en los individuos con SPW en un contexto de un enfoque nutricional no farmacológico como parte de un RTT.
Prader Willi syndrome (PWS) is a rare genetic disease caused by a lack of the expression of paternally inherited genes in the chromosome 15q11–q13 region, with an approximate prevalence of 1:15000.1 Nutritional features include generalised hypotonia, slow metabolic rate, lower caloric expenditure, short stature, and hyperphagia.2 Overall, these can promote the development of early obesity, the leading cause of morbidity and mortality.3 The pathophysiology of hyperphagia is not fully elucidated, although it has been related to abnormalities in the hypothalamic satiety centre and its downstream hormones.3,4 Hyperphagia starts at an early age and has different nutritional stages. These have been described according to behaviour, growth, laboratory, and metabolic changes.5 Nutritional treatment must be implemented immediately to prevent obesity since it is closely associated with life expectancy.6 Reports regarding hyperphagia management strategies in individuals with PWS are scarce. Moreover, studies concerning pharmacological approaches have shown suboptimal results. In our institution, the inherent nutritional plan, immersed in a transdisciplinary approach, is non-pharmacological and mainly comprises an environment with limited food access, daily schedule, exercises, and an energy-restricted and well-balanced diet. It also includes food and nutritional re-education for both patients and all their caregivers. Therefore, we sought to evaluate behaviours related to hyperphagia in individuals with PWS under a transdisciplinary non-pharmacological approach.
Materials and methodsThis observational study included individuals with PWS of both genders, regardless of their genetic subtype, weight, height, body mass index (BMI), with or without a therapeutic companion. The study population comprised individuals with PWS under regular transdisciplinary treatment (RTT) in an institution dedicated to rare diseases. RTT is characterised by a transdisciplinary approach that involves, in addition to nutrition, internal medicine, occupational therapy, kinesiology, physiatry, educational psychology, psychology, psychiatry, and speech therapy. The treatment is ambulatory, and patients were not living in the institution. RTT is developed at a pre-established frequency (weekly, biweekly or monthly) by a team of professionals according to the needs and resources of the individuals with PWS and their families. On each visit, the patient and the family stay 4h in the institution.
From a nutritional basis, the non-pharmacological approach was based on implementing a controlled environment through the application of limits to food access (lock on the kitchen door, refrigerator, cupboards, not allowing handling money or food, avoiding shopping, and avoiding staying alone). It also comprised forging a daily structure anticipating changes and clear and enduring limits.7 The nutritional approach of RTT also included an energy-restricted and well-balanced diet, food and nutritional re-education for both individuals with PWS and all their caregivers (families and teachers) and physical activity. The energy-restricted and well-balanced diet is adapted to the patient's clinical picture, nutritional diagnosis, age and comorbidities. Given their slow metabolism, short height and characteristic body composition, the caloric restriction of their diet must be adequately observed. An individual with PWS requires 20–40% fewer calories than a person without the syndrome.8 Besides, the diet must provide complete coverage of essential nutrients and energy requirements and has to be structured to avoid anxiety and uncertainty, occasionally being necessary to evaluate supplementary needs. The rate of weight loss should be monitored and growth and development in children.
The control group comprised individuals with PWS who made occasional contact with our institution (therapeutic assessment) but without initiation of RTT. Individuals with severe intellectual disability, without verbal expression, without gestural communication skills, or whose caregivers did not provide meaningful information were excluded.
The assessment of behaviours related to hyperphagia was performed using the Hyperphagia Questionnaire for Clinical Trials (HQ-CT) questionnaire, which was provided to all the families involved. The Foundation for Prader-Willi Research granted the license for its use. This 9-item questionnaire is a caregiver-reported instrument, and it has Likert-type response options, ranging from 0 to 4 according to frequency, 0 the most favourable answer and 4 the least. The total range of score for HQ-CT is 36. However, threshold values have not been established for this instrument, thus precluding the ability to discriminate results according to severity. Nevertheless, it was considered the most appropriate tool considering it was specifically developed for PWS and is commonly used among these individuals.
The questions were discriminated in three categories: arguing or manipulating to obtain food, anger or tantrums related to food, and sneaking food.
All procedures were performed in accordance with the ethical standards of the Declaration of Helsinki of 1964 and its further amendments.
Continuous variables were reported as means±standard deviation or median (interquartile range) in the case of non-uniform distribution, while categorical variables were reported as counts and percentages. Comparisons between groups were evaluated using paired or independent samples T-tests and nonparametric Mann–Whitney U tests. All analyses were performed using SPSS software, version 22.0 (IBM SPSS Statistics for Windows, Armonk, NY).
ResultsWe evaluated a total of 43 individuals with PWS, of whom 21 comprised patients under RTT and 22 individuals with PWS without RTT (control group). The mean age at baseline (treatment onset) was 18.4±8.3 years (range 3–32 years) in the RTT group and 19.1±6.9 years (range 5–35 years) in the control group (p=0.74). No differences were detected regarding gender (RTT: 33% women, control: 36% women; p=0.84). All caregivers successfully completed the hyperphagia questionnaire.
Hyperphagia-related behaviours, assessed in the RTT group after a median treatment duration of 41 months (interquartile range 11; 88 months), were significantly lower among PWS individuals under RTT compared to the control group (RTT 5.7±3.7 vs control 13.1±7.5, p<0.0001). This was identified independently within the three categories: arguing or manipulating to obtain food (RTT 2.71±2.1 vs control 5.41±3.2, p=0.003), sneaking food (RTT 1.33±1.5 vs control 3.55±3.3, p=0.007), and anger or tantrums related to food (RTT 1.67±1.8 vs control 4.09±2.7, p=0.001) (Fig. 1)
After discrimination according to age, individuals with PWS under 18 years old within the RTT group had greater behaviours related to hyperphagia compared to older subjects, particularly concerning manipulation (<18 years old: 3.82±2.3 vs ≥18 years old: 1.50±1.2, p=0.009) (Table 1).
Mean hyperphagia-related behaviours in a group under regular transdisciplinary treatment (RTT) and a control group without RTT, discriminated by age.
| RTT | Control group | |||||
|---|---|---|---|---|---|---|
| ≥18 years old (n=10) | <18 years old (n=11) | p value | ≥18 years old (n=12) | <18 years old (n=10) | p value | |
| Mean hyperphagia | ||||||
| Total | 4.10±2.2 | 7.18±4.2 | 0.050 | 14.42±8.5 | 11.4±6.0 | 0.34 |
| Manipulation | 1.50±1.2 | 3.82±2.3 | 0.009 | 5.75±3.4 | 5.00±3.1 | 0.60 |
| Sneaking food | 1.60±1.8 | 1.09±1.1 | 0.45 | 4.42±3.5 | 2.50±2.9 | 0.17 |
| Tantrums | 1.00±0.9 | 2.27±2.1 | 0.10 | 4.25±2.8 | 3.90±2.7 | 0.35 |
| Differences between age groups (p values RTT vs control) | ||||||
| Total | 0.001 | 0.077 | ||||
| Manipulation | 0.001 | 0.33 | ||||
| Sneaking food | 0.032 | 0.15 | ||||
| Tantrums | 0.002 | 0.14 | ||||
Differences between groups were evaluated using independent samples T-tests.
We did not identify significant gender-related differences in hyperphagia-related behaviours in neither group (RTT: total, p=0.54; manipulation, p=0.53; sneaking food, p=0.11; tantrums, p=0.17; Control: total, p=0.34; manipulation, p=0.87; food sneaking, p=0.34; tantrums, p=0.23).
The baseline BMI of the RTT group was 38.7±17.1kg/m2 [median 35.5kg/m2 (interquartile range 26.2; 52.0)], compared to 37.7±12.3kg/m2 in the control group (RTT 38.7±17.1kg/m2 vs control 37.7±12.3kg/m2, p=0.83). After a mean treatment period of 41.0 months (interquartile range 10.5–88.0), the RTT group had a significant reduction in BMI (baseline 38.7±17.1kg/m2 vs follow-up 29.2±9.2kg/m2; p<0.0001). Since the control group was not followed up, the BMI of the control group after 41 months is unknown.
A significant association was identified between RTT duration and BMI reduction, with, more significant BMI reductions in individuals with PWS who attended to RTT for a period longer than the median RTT duration (ΔBMI (%) −13.8±11.7 vs −4.7±5.4, p=0.037) (Table 2).
Mean body mass index (BMI) and hyperphagia-related behaviours discriminated by the duration of the regular transdisciplinary treatment (RTT).
| RTT duration | p value | |||
|---|---|---|---|---|
| Total (n=21) | <41 months (n=10) | ≥41 months (n=11) | ||
| Baseline BMI | 38.7±17.1 | |||
| ΔBMI (kg/m2) | −9.5±10.1 | −4.7±5.4 | −13.8±11.7 | 0.037 |
| ΔBMI (%) | −18.6±18.0 | −10.7±14.5 | −25.7±18.4 | 0.052 |
| Hyperphagia (total) | 5.7±3.7 | 6.8±4.1 | 4.7±3.1 | 0.205 |
| Manipulation | 2.7±2.1 | 3.9±2.3 | 1.6±1.3 | 0.012 |
| Sneaking food | 1.3±1.4 | 0.9±1.1 | 1.7±1.7 | 0.202 |
| Tantrums | 1.7±1.8 | 2.0±1.8 | 1.4±1.7 | 0.425 |
Differences between groups were evaluated using independent samples T-tests.
Individuals with PSW require close monitoring by their caregivers, leading to overload and, in some cases, burnout. The quality of life of these subjects and their families is compromised, and the search for interventions to reduce behaviours related to hyperphagia is considered highly appreciated. ueRegarding pharmacotherapy, whilst many advances have been made, studies using different agents such as GLP-1 receptor antagonists, potassium channel activators, and unacylated ghrelin analogues have been preliminary reported inconclusive findings in terms of safety and clinical effectiveness.8,9,11
Early intervention of behaviours related to hyperphagia should comprise weight control, preventing the development of overweight or obesity, or reversing it. The effect of RTT, based on a controlled environment, limits to food access, well-balanced diet, a forged daily structure, and nutritional education for individuals with PWS and caregivers, was reflected in a significant decrease in the BMI. It is noteworthy that such an approach was implemented among all the frequent places where individuals with PWS carry out their activities.
It is noteworthy that despite identifying a significant reduction in BMI and hyperphagia behaviours among patients immersed in an RTT after a median treatment of 41 months, causality cannot be fully established given the lack of longitudinal assessment of patients in the control group.
Concern for food and unrestricted access leads to disruptive behaviours (tantrums, anger) that can be mitigated by applying these strategies.8 Moreover, nutritional treatment must be accompanied by physical activity; and strict supervision and food re-education for families and individuals with PWS should be part of the approach.10
Our findings underscore the importance of nutritional intervention for managing hyperphagia-related behaviours. However, it should be acknowledged that since it was immersed within a transdisciplinary approach, our study does not offer accurate estimations regarding the discriminated impact of each therapeutic area involved. Moreover, despite the demonstration of a positive impact on behaviours related to hyperphagia and a significant reduction in BMI, a causal relationship cannot be fully established, given the retrospective nature of our study. On the other hand, although the sample size might be regarded as relatively small and therefore lead to selection bias, it should be emphasised that this study involved a rare disease. Besides, we did not analyse the relationship between hyperphagia-related behaviours and the genetic subtype, although we acknowledge that this issue warrants specific consideration in future studies.
ConclusionsIn this study, including individuals with PWS, a non-pharmacological nutritional approach immersed in a transdisciplinary treatment was related to a positive impact on behaviours related to hyperphagia and a significant reduction in BMI.
FundingNone declared.
Conflict of interestNone of the authors has conflicts of interest to declare related to the manuscript's content. All authors had access to the data and a role in writing the manuscript.
We would also like to thank Gaston Rodríguez Granillo, María Mercedes Orzi, Tomas Capeluto, Yohanna González Ruiz, Anabela Galiana, Alejandro Gerónimo, and Pablo Cabrera for this paper and the research behind. It would not have been possible without their exceptional support.