Some epidemiological data suggest that there may be an inverse relationship between cholesterol levels and the risk of thyroid cancer in the overall population. The present study was aimed to evaluate the lipid profile specifically in subjects with Bethesda category IV thyroid nodules, and compare whether there were any differences between those with benign and malignant nodules.
MethodsSingle-centre, retrospective study on 204 subjects treated by partial or total thyroidectomy for excision of a Bethesda category IV thyroid nodule, who had undergone a blood lipid profile test in the 12 months prior to surgery. In addition to lipid measures, other demographic, clinical, biochemical and ultrasound data were collected.
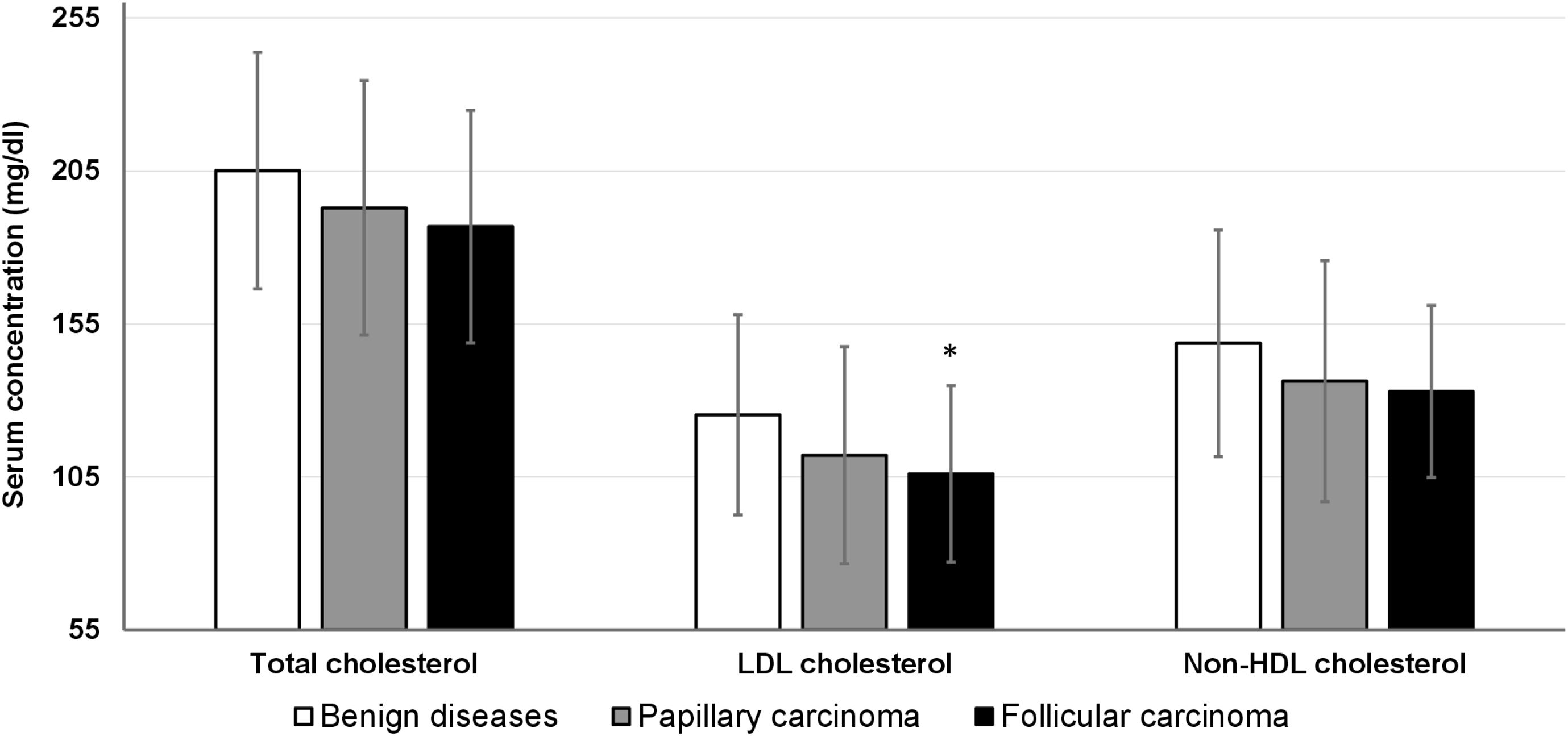
ResultsSeventy-five subjects (36.8%) were diagnosed with thyroid carcinoma in the definitive histopathological examination. Patients with thyroid cancer had lower levels of total cholesterol, LDL-cholesterol and non-HDL-cholesterol than subjects with benign thyroid diseases. There were no differences in HDL-cholesterol, triglycerides or total cholesterol/HDL-cholesterol ratio. There were no differences either between groups in other clinical, biochemical and ultrasound variables, including the use of lipid-lowering drugs. In multivariate analysis, only LDL-cholesterol was independently associated with malignancy. Subjects with follicular carcinoma showed the lowest cholesterol levels, while those with papillary carcinoma had intermediate values between the group with follicular carcinoma and the group with benign thyroid diseases.
ConclusionsIn subjects with cytologically indeterminate Bethesda category IV thyroid nodules, levels of total cholesterol, non-HDL-cholesterol and, particularly, LDL-cholesterol are lower among those with malignant nodules.
Algunos datos epidemiológicos sugieren que, a nivel de la población general, puede existir una relación inversa entre los niveles de colesterol y el riesgo de cáncer de tiroides. El presente estudio tuvo como objetivo evaluar el perfil lipídico específicamente en sujetos con nódulos tiroideos categoría Bethesda IV, y comparar si existían diferencias entre aquellos con nódulos benignos y malignos.
MétodosEstudio retrospectivo unicéntrico en 204 sujetos tratados mediante tiroidectomía parcial o total para exéresis de un nódulo tiroideo categoría Bethesda IV, a los que se había realizado un análisis del perfil lipídico sanguíneo en los 12 meses previos a la cirugía. Además de las medidas lipídicas, se recogieron otros datos demográficos, clínicos, bioquímicos y ecográficos.
ResultadosSetenta y cinco sujetos (36,8%) fueron diagnosticados de carcinoma tiroideo en el estudio histopatológico definitivo. Los pacientes con cáncer de tiroides tenían niveles más bajos de colesterol total, colesterol-LDL y colesterol no-HDL que los sujetos con enfermedades tiroideas benignas. No hubo diferencias en el colesterol HDL, los triglicéridos o la relación colesterol total/colesterol HDL. Tampoco hubo diferencias entre los grupos en otras variables clínicas, bioquímicas ni ecográficas, incluido el uso de fármacos hipolipemiantes. En el análisis multivariante, solo el colesterol LDL se asoció de forma independiente con la malignidad. Los sujetos con carcinoma folicular mostraron los niveles de colesterol más bajos, mientras que los que presentaban carcinoma papilar tenían valores intermedios entre el grupo con carcinoma folicular y el grupo con enfermedades tiroideas benignas.
ConclusionesEn sujetos con nódulos tiroideos citológicamente indeterminados de categoría Bethesda IV, los niveles de colesterol total, colesterol no-HDL y, particularmente, colesterol-LDL son más bajos entre aquellos con nódulos malignos.
Ultrasound and echo-guided fine needle aspiration biopsy (FNAB) is the mainstay procedure for diagnostic evaluation of thyroid nodules. In cases where FNAB is performed, the Bethesda System for Reporting Thyroid Cytopathology—first published in 20101—is the most widely used method to assess cytological specimens. This system categorizes thyroid nodules into 6 cytological types (Bethesda categories I–VI), each associated with a different risk of malignancy. Approximately 10% of thyroid nodules are classified into category IV,2,3 labelled with the term “follicular neoplasm” in the latest update of the Bethesda System.4 Category IV is probably the most problematic one since, in these cases, cytology cannot differentiate between malignant (usually follicular carcinoma or follicular variant of papillary carcinoma) and benign lesions. The risk of malignancy of follicular neoplasms is estimated to be approximately 30%,1–5 so it is usually necessary to proceed with a thyroid lobectomy to perform a complete histopathological examination and establish a definitive diagnosis. Although molecular diagnostic techniques have been proposed to refine the risk stratification of malignancy in Bethesda category IV nodules,6 their use is limited by their high cost and they are not available in most centres. Because of this, numerous studies have been directed towards the search for characteristics, mainly ultrasonographic7,8 and cytological9,10 that can help us predict the risk of malignancy among nodules with cytology of undetermined risk. In recent years, the use of artificial intelligence techniques capable of improving the interpretation of ultrasound Images11 and cytology12 has also been incorporated. However, for the time being, the results have not been completely conclusive and it is still necessary to continue searching for markers that can contribute to a better estimation of the risk of malignancy in this type of cases.
The identification of clinical or biochemical risk markers could be very useful since, as a recent study has pointed out, they could be incorporated, together with ultrasound and cytology, in predictive artificial intelligence models based on machine learning.13
Among the potential biochemical markers, the possible association between lipid levels and thyroid cancer has not received much attention, at least until very recently. Some cross-sectional and case-control design studies compared circulating lipid levels between patients with thyroid cancer and subjects with benign thyroid pathology and the overall population, with contradictory results. Recently, however, a large prospective epidemiological study conducted in Sweden14 reported that, during the years prior to diagnosis, patients with thyroid cancer have lower and progressively decreasing levels of total cholesterol and HDL cholesterol vs controls, whose levels remain constant or on the rise. To date, no study has evaluated whether lipid profile could help in the assessment of the risk of malignancy among subjects with thyroid nodules. The present study was conducted to compare the lipid profile of patients with thyroid nodules with Bethesda IV cytology and evaluate whether there are any differences between patients with benign nodules and those with malignant ones.
Material and methodsSubjectsThis study included all patients who underwent partial or total thyroidectomy at the Complejo Hospitalario Universitario Insular Materno Infantil from 2013 to 2022 for excision of a thyroid nodule with Bethesda IV cytology obtained by ultrasound-guided FNAB, in whom a determination of blood lipid profile had been performed before a maximum of 12 months prior to the intervention.
Study variablesSubjects were categorized into 2 groups, with thyroid cancer or with benign thyroid disease, according to the results of the histopathological examination. Patients with noninvasive follicular thyroid neoplasms with papillary-like nuclear features (NIFTP) were included in the benign group. Lipid profile data, including total cholesterol, HDL-cholesterol and triglycerides, were collected for each participant from the laboratory study performed closest to the date of FNAB, prior to the surgery. LDL-cholesterol was calculated using the Friedewald formula, non-HDL-cholesterol as the difference between total cholesterol and HDL-cholesterol, and the total cholesterol/HDL cholesterol ratio (Castelli Index) as the ratio between total cholesterol and HDL cholesterol.15
Other demographic and clinical variables were also collected (age, sex, body mass index, history of diabetes mellitus, hypertension, cardiovascular disease, treatment with lipid-lowering drugs and hypothyroidism), serum levels of fasting glucose, TSH and creatinine, as well as ultrasound characteristics of the nodule with suspicious cytology (anteroposterior, transverse and craniocaudal diameters, volume, calculated using the formula of the elipsoid [length×width×height]×π/6] and ultrasound category according to the Thyroid Imaging Reporting and Data System [TIRADS]16). A diagnosis of diabetes was established in all cases with a previous diagnosis of the disease and/or fasting blood glucose≥126mg/dL. The glomerular filtration rate was estimated using the EPI-CKD formula.
Ethical issuesThis study was performed in full compliance with the principles set forth in the Declaration of Helsinki. The study was approved by the Ethics and Drug Research Committee of the province of Las Palmas. Since all data were obtained retrospectively, the exemption of requesting informed consent from the study subjects was accepted.
Statistical analysisCategorical variables are expressed as frequencies and percentages and numerical variables as means (± SD) or medians (interquartile range), depending on whether data followed a normal distribution. Frequencies were compared using the Chi-square test, and numerical variables using the Student's t-test or ANOVA, and by Mann–Whitney or Kruskal–Wallis tests, depending on the distribution of the data and the number of groups compared. The Bonferroni method was used for post hoc comparisons in the ANOVA test. Logistic regression analysis was performed to analyze the independent association between lipid profile variables and malignancy.
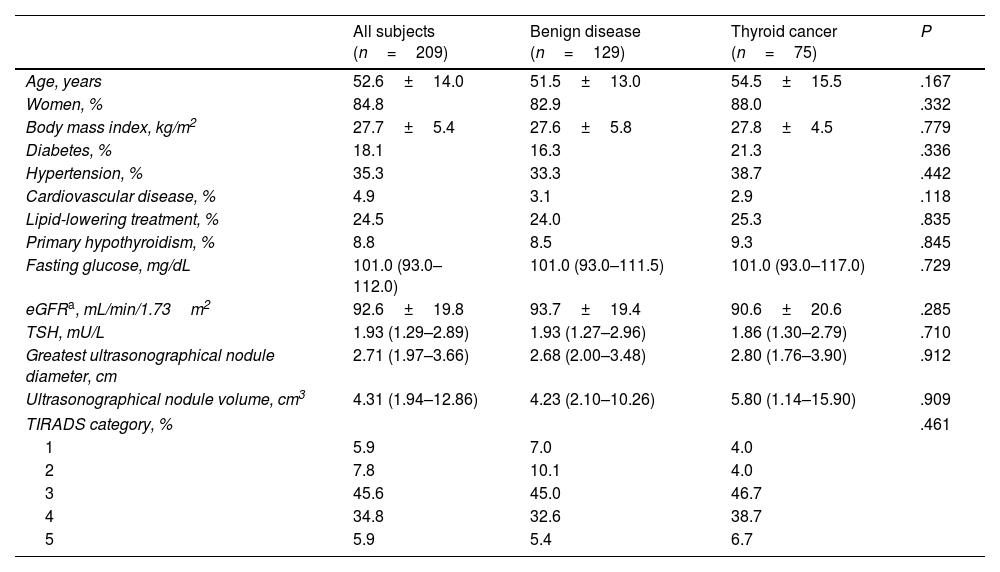
ResultsWe identified a total of 204 patients who met the inclusion criteria, 75 of whom (36.8%) were diagnosed with thyroid cancer on definitive histopathological examination (30 follicular carcinoma, 26 follicular variant of papillary carcinoma, 18 other types of papillary carcinoma and 1 medullary carcinoma), while the remaining 129 had benign thyroid diseases (71 follicular adenoma, 41 follicular nodular hyperplasia, 9 chronic lymphocytic thyroiditis and 8 NIFTP). Table 1 shows the general characteristics of the study population, overall, and by groups with benign and malignant nodules. There were no differences between groups with respect to any demographic, clinical, biochemical or ultrasound characteristics.
Clinical, biochemical and ultrasound characteristics of the participants, overall, and based on the definitive results of the histopathological examination.
| All subjects (n=209) | Benign disease (n=129) | Thyroid cancer (n=75) | P | |
|---|---|---|---|---|
| Age, years | 52.6±14.0 | 51.5±13.0 | 54.5±15.5 | .167 |
| Women, % | 84.8 | 82.9 | 88.0 | .332 |
| Body mass index, kg/m2 | 27.7±5.4 | 27.6±5.8 | 27.8±4.5 | .779 |
| Diabetes, % | 18.1 | 16.3 | 21.3 | .336 |
| Hypertension, % | 35.3 | 33.3 | 38.7 | .442 |
| Cardiovascular disease, % | 4.9 | 3.1 | 2.9 | .118 |
| Lipid-lowering treatment, % | 24.5 | 24.0 | 25.3 | .835 |
| Primary hypothyroidism, % | 8.8 | 8.5 | 9.3 | .845 |
| Fasting glucose, mg/dL | 101.0 (93.0–112.0) | 101.0 (93.0–111.5) | 101.0 (93.0–117.0) | .729 |
| eGFRa, mL/min/1.73m2 | 92.6±19.8 | 93.7±19.4 | 90.6±20.6 | .285 |
| TSH, mU/L | 1.93 (1.29–2.89) | 1.93 (1.27–2.96) | 1.86 (1.30–2.79) | .710 |
| Greatest ultrasonographical nodule diameter, cm | 2.71 (1.97–3.66) | 2.68 (2.00–3.48) | 2.80 (1.76–3.90) | .912 |
| Ultrasonographical nodule volume, cm3 | 4.31 (1.94–12.86) | 4.23 (2.10–10.26) | 5.80 (1.14–15.90) | .909 |
| TIRADS category, % | .461 | |||
| 1 | 5.9 | 7.0 | 4.0 | |
| 2 | 7.8 | 10.1 | 4.0 | |
| 3 | 45.6 | 45.0 | 46.7 | |
| 4 | 34.8 | 32.6 | 38.7 | |
| 5 | 5.9 | 5.4 | 6.7 | |
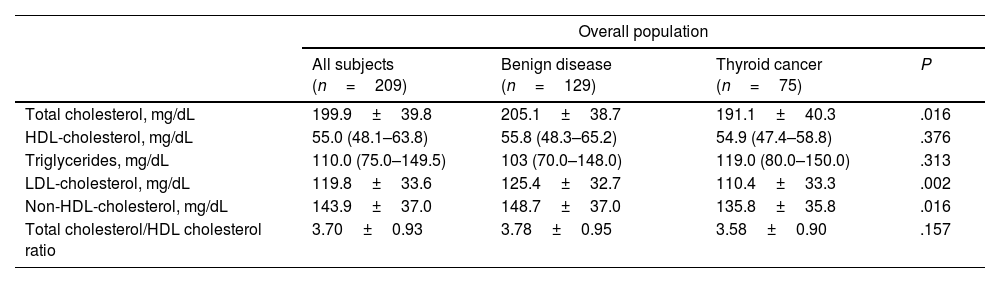
Table 2 shows lipid levels in subjects with benign and malignant diseases. Patients with thyroid cancer had lower levels of total cholesterol, LDL-cholesterol and non-HDL-cholesterol than those with benign nodules. There were no differences between the 2 groups with respect to HDL-cholesterol or triglyceride values, or in the total cholesterol/HDL-cholesterol ratio. Although the percentage of patients using lipid-lowering drugs was similar between subjects with and without cancer, for a better evaluation of the interference of lipid-lowering treatment on lipid levels, Table 2 also shows the lipid values among the 152 subjects not using any lipid-lowering therapies. Also in this subgroup, the concentrations of total cholesterol, LDL cholesterol and non-HDL cholesterol were lower among the cancer patients, although the differences did not reach statistical significance. However, the total cholesterol/HDL cholesterol ratio was lower among patients with malignant disease than among those with benign disease.
Lipid profile of all participants and of those who did not follow lipid-lowering treatment based on the final results of the histopathological examination.
| Overall population | ||||
|---|---|---|---|---|
| All subjects (n=209) | Benign disease (n=129) | Thyroid cancer (n=75) | P | |
| Total cholesterol, mg/dL | 199.9±39.8 | 205.1±38.7 | 191.1±40.3 | .016 |
| HDL-cholesterol, mg/dL | 55.0 (48.1–63.8) | 55.8 (48.3–65.2) | 54.9 (47.4–58.8) | .376 |
| Triglycerides, mg/dL | 110.0 (75.0–149.5) | 103 (70.0–148.0) | 119.0 (80.0–150.0) | .313 |
| LDL-cholesterol, mg/dL | 119.8±33.6 | 125.4±32.7 | 110.4±33.3 | .002 |
| Non-HDL-cholesterol, mg/dL | 143.9±37.0 | 148.7±37.0 | 135.8±35.8 | .016 |
| Total cholesterol/HDL cholesterol ratio | 3.70±0.93 | 3.78±0.95 | 3.58±0.90 | .157 |
| Population not treated with lipid-lowering drugs | ||||
|---|---|---|---|---|
| All subjects (n=152) | Benign disease (n=96) | Thyroid cancer (n=56) | P | |
| Total cholesterol, mg/dL | 202.1±37.0 | 204.6±37.2 | 197.9±36.5 | .282 |
| HDL-cholesterol, mg/dL | 55.3 (48.9–64.4) | 54.2 (48.4–64.4) | 55.3 (49.3–64.1) | .426 |
| Triglycerides, mg/dL | 95 (70.0–143.0) | 91 (68.2–144.7) | 99 (73.0–141.0) | .607 |
| LDL-cholesterol, mg/dL | 123.8±31.3 | 127.2±31.2 | 117.8±30.6 | .076 |
| Non-HDL-cholesterol, mg/dL | 145.5±35.6 | 148.8±36.6 | 139.8±33.5 | .136 |
| Total cholesterol/HDL cholesterol ratio | 3.7±0.9 | 3.8±1.0 | 3.5±0.7 | .034 |
Analyzing patients with follicular carcinoma and papillary carcinoma (of any type) separately, and excluding the one case with medullary carcinoma, the follicular carcinoma group showed the lowest cholesterol levels, while the papillary carcinoma group showed intermediate values between follicular carcinoma and benign diseases groups (Fig. 1). Overall, the ANOVA test showed statistically significant differences between groups for both LDL cholesterol and total and non-HDL cholesterol, although multiple comparisons between groups only detected significant differences for LDL cholesterol levels between the group with benign diseases and the group with follicular carcinoma (125.3±32.7 vs 106.0±28.9mg/dL) (Fig. 1).
In the multiple logistic regression analysis, including all 3 cholesterol measures that were significantly associated with malignancy in univariate analyses (total, LDL and non-HDL), only LDL cholesterol was inversely and independently associated with thyroid cancer (OR, 0.98, [95%CI, 0.97–0.99]; P=.049).
DiscussionThe possible role of lipid homeostasis in the development and progression of cancer has been and remains controversial.17 Regarding thyroid cancer, several cross-sectional and case-control design studies observed that serum concentrations of total cholesterol or LDL cholesterol are not associated with thyroid cancer risk,18–21 but some have shown a positive correlation22,23 and others an inverse one.24,25 The association between low cholesterol levels and an increased risk of cancer has been explained for other types of malignant neoplasms as an inverse causal relationship.26 Therefore, through different pathways, which could include the disease per se, malnutrition or unhealthy lifestyle habits, such as excessive alcohol intake or smoking, serum cholesterol levels could be lower in people who develop cancer. However, some very long-term prospective studies have observed that this inverse association persists even up to more than 10 years before cancer diagnosis,27 which could not be entirely attributed to a preclinical effect of undiagnosed cancer. Recently, along the same lines, and in relation to thyroid cancer, the study based on the cohort recruited for the AMORIS trial (Apolipoprotein-Related Mortality Risk), which followed a total of 561,388 individuals from the general Swedish population for more than 30 years, showed that, compared to the control population, individuals who developed thyroid cancer had consistently lower levels of total cholesterol and HDL-cholesterol during the decades prior to diagnosis and that, in the 10 years prior to diagnosis, thyroid cancer patients showed decreasing cholesterol levels, while controls showed stable or increasing levels.14 These findings also call into question an inverse causal relationship between cancer and cholesterol levels, even more so in the case of thyroid cancer, in which most tumours are located exclusively within the thyroid gland, have a good prognosis and do not affect the general condition. In any case, beyond the possible causal mechanism, the AMORIS trial highlights that, at the time of diagnosis, patients with thyroid cancer tend to have lower serum cholesterol concentrations and suggests, therefore, that the determination of lipid levels could assist in the preoperative diagnosis of the disease, particularly in those cases in which the usual diagnostic procedures, mainly cytology obtained by echo-guided FNAB, are inconclusive.
This is the first study aimed at evaluating lipid levels specifically in subjects with Bethesda category IV thyroid nodules and comparing to see whether there are differences between those with benign and malignant nodules. The results showed that, in this type of patients with indeterminate nodules, the levels of total cholesterol, non-HDL cholesterol and, above all, LDL cholesterol were lower among those with malignant nodules.
Cholesterol is an essential component for the maintenance and function of cell membranes and it has been proposed that neoplastic cells, which are highly proliferative, can capture and retain greater amounts of macronutrients, including cholesterol, due to the greater need for lipids for the synthesis of new membranes.28 It has been shown that several types of cancer overexpress the LDL receptor (LDLR), and that upregulation of LDLR expression constitutes a mechanism of tumour progression in more aggressive cancers.29 In this regard, Revilla et al.30 demonstrated increased LDLR expression in more aggressive thyroid carcinomas (high-risk and dedifferentiated papillary carcinomas and anaplastic carcinomas), compared to low- or intermediate-risk papillary carcinomas and benign thyroid lesions. Interestingly, although these authors analyzed a very small group of patients, those with more aggressive tumours also had lower serum levels of total cholesterol, LDL cholesterol and apolipoprotein B than those with benign lesions.30 A larger study conducted in China25 similarly observed that patients with metastatic papillary carcinoma had lower levels of total cholesterol and various serum apo and lipoproteins (LDL-cholesterol, HDL-cholesterol, lipoprotein(a), apolipoprotein B and apolipoprotein A1) than patients without extrathyroidal extension. This trend was also seen for patients with follicular carcinomas, but the differences did not reach statistically significant differences. However, the subgroup of patients with metastatic follicular carcinoma had the lowest total cholesterol and LDL-cholesterol values of all the groups studied. Also in the present study, patients with follicular carcinoma were those with the lowest concentrations of total, LDL- and non-HDL-cholesterol, while patients with papillary carcinoma showed intermediate levels between those with follicular carcinoma and those with benign thyroid lesions. These findings are consistent in pointing out that the most aggressive thyroid neoplasms are those associated with lower circulating cholesterol values.
One of the main limitations of this study is the small size of the population studied. Therefore, further studies are needed to check whether its results are replicable in other populations. On the other side, cholesterol levels are subject to different variables that may change their results, mainly the use of statins, which are used by approximately one quarter of the European population.31 If it is eventually confirmed that cholesterol levels are lower in patients with malignant nodules with indeterminate cytology, it would be important to clarify the degree of interference that lipid-lowering therapy may exert on the potential use of cholesterol levels as a risk marker of malignancy. In our study, the differences in total cholesterol, LDL cholesterol, and non-HDL cholesterol levels did not reach statistical significance between subjects that were not taking lipid-lowering drugs, yet this could have been solely due to the loss of statistical power with the decrease in population size. Indeed, among subjects not treated with hypolipidemic drugs, the differences in LDL cholesterol were close to statistical significance, and the total cholesterol/HDL cholesterol ratio was lower among those with malignant nodules.
Our results showed a high degree of overlap between the cholesterol values observed between patients with benign and malignant nodules. It is, therefore, highly unlikely that cutoff points for lipid levels can be identified to be used individually to reliably estimate the risk of malignancy in patients with thyroid nodules with Bethesda IV cytology. However, the results of this study suggest that cholesterol has a greater discriminatory capacity than other clinical, biochemical or ultrasound data for the identification of patients with thyroid cancer and that, therefore, and especially with the advent of the use of artificial intelligence, it should be considered as a variable of interest for the design of mathematical models aimed at estimating the risk of malignancy in this type of patients.
Authors’ contributionsMB conceived and designed the work and the statistical analyses. BMM compiled the data and collaborated in the analysis of the results. YLP, DMA and CARP conducted the ultrasound and FNBA studies, and were the main clinical managers of the participants. The first draft of the manuscript was written by MB and BMM. All authors participated in the manuscript revision and approved its final version.
FundingNone declared.
Conflicts of interestNone declared.