Cervical chyle fistula (CF) is exceptional, and there is no agreement on its treatment. The study objective was to assess the efficacy of conservative and surgical treatment in this condition.
MethodStudy population: Patients undergoing thyroid surgery who experience CF after the procedure. Study groups: (1) Group with conservative treatment: CF with flow rates less than 300cm3/day, late or collected in the neck; and (2) Group with surgical treatment: early CF with flow rates greater than 300cm3/day. Study variables: Cure rates and rate of conversion to surgery were analyzed.
ResultsNine patients experienced CF. Conservative treatment was started in all of them, in 67% (n=6) with curative intent. Fifty percent of treated cases were resolved (n=3). The remaining patients were hospitalized after more than 150 days of treatment to add absolute diet and parenteral nutrition. The condition resolved in one patient, and the other two were referred for surgery.
In the remaining patients (33%, n=3), surgery was indicated as the initial definitive treatment. A cervical approach, with ligature and transfixion stitch of the thoracic duct, was used. In one of the patients, who also had chylothorax, thoracoscopy was also performed. In the two patients where conservative treatment failed, cervicotomy was indicated, identifying in both the lymphatic reflux point. Fistula resolved in all operated patients.
ConclusionsConservative treatment was effective in 66% of low flow CFs. Surgery effectively and rapidly resolves fistulas with a high flow or not responding to conservative treatment.
La fístula quilosa (FQ) cervical es excepcional y no existe consenso sobre su tratamiento. El objetivo es analizar la eficacia de los tratamientos conservador y quirúrgico en esta patología.
MétodoPoblación a estudio constituida por pacientes con cirugía tiroidea que presentan en la evolución posquirúrgica una FQ. Grupos a estudio: 1) Grupo con tratamiento conservador, formado por FQ con débito inferior a 300cm3/día, tardías o coleccionadas en el cuello; y 2) Grupo con tratamiento quirúrgico, formado por FQ precoces con débito superior a 300cm3/día. Variables a estudio: Se analizan los resultados en cuanto a tasas de curación y la tasa de reconversión a tratamiento quirúrgico.
ResultadosNueve pacientes presentaron una FQ. Todos iniciaron tratamiento conservador; de ellos, el 67% (n=6) con intención curativa, resolviéndose el 50% de los casos (n=3). Los restantes, tras más de 150 días de tratamiento, fueron ingresados para añadir dieta absoluta y nutrición parenteral. Uno de ellos se resolvió, siendo los otros 2 casos remitidos a cirugía.
En los casos restantes (33%; n=3) se indicó la cirugía como tratamiento definitivo inicial. El abordaje fue cervical con ligadura y punto transfixivo del conducto torácico. En uno de los pacientes, que asociaba un quilotórax, se asoció una toracoscopia. En los 2 casos en quienes fracasó el tratamiento conservador, se indicó la cirugía mediante cervicotomía, identificando el punto de reflujo linfático. Todos los operados han presentado resolución de la fístula.
ConclusionesEl tratamiento conservador es efectivo en el 66% de las FQ de bajo débito. En las fístulas de débito alto, o donde el tratamiento conservador no es efectivo, la cirugía ofrece una resolución efectiva y rápida del cuadro.
The lymphatic system consists of a large network of capillaries and vessels distributed throughout the body that converge at chest level in the thoracic duct, which in turn drains into the systemic circulation at the left jugular-subclavian venous angle. One of the salient features of lymph is its milky appearance, with a relative density of over 1.012, a high content in fat (total fat between 0.4 and 4g/l), a total protein concentration of >30g/l, a pH >7, a predominance of lymphocytes, and the presence of lipophilic globules that stain with Sudan III dye. Lymph contains components derived from products absorbed in the intestine, as well as lymphocytes from the lymph nodes and lymphatic organs, and has a flow rate of 2–4l every 24h.1
The development of a chyle fistula as a result of damage to the thoracic duct or one of its tributaries following neck dissection and lymphadenectomy is a rare complication,1 and there is no consensus on the most appropriate management approach.
The seriousness of this disorder lies in the local and systemic complications, which expose the patient to high morbidity and mortality if adequate treatment is not provided.2 The therapeutic approaches vary depending on whether fistular output is low or high. In this regard, low output fistulas tend to be treated conservatively, while surgery is the management of choice in high output cases. The conservative management of chyle fistula includes evacuation through thoracocentesis, paracentesis, and the placement of different types of drains. Likewise, long-chain triglycerides (LCTs) in the diet are replaced with medium-chain triglycerides (MCTs) in order to cancel fatty acid entry to the lymph, total parenteral nutrition, and the addition of somatostatin.3–6 When conservative treatment proves ineffective, surgery appears to be the best option, though when it should be indicated may be subject to controversy.
The present study is concerned with the treatment of cervical chyle fistula secondary to surgery for malignant thyroid disease in an endocrinological surgery reference unit, and was carried out with the following objectives: (1) to analyze the efficacy of medical treatment in low output fistulas; (2) to analyze the efficacy of surgical treatment in high output fistulas; and (3) to determine which patients with low output fistulas might benefit from early surgical treatment.
Patients and methodsStudy populationThe study population consisted of patients undergoing surgery in the form of total thyroidectomy, with or without associated cervical lymphadenectomy, and who presented a chyle fistula during the postoperative period. Chyle fistula refers to the presence of a milky (chylous) fluid in the surgical drain bag after thyroidectomy, or (in patients without drainage) the presence of a postoperative cervical collection from which lymph is drawn at puncture. Triglycerides and cholesterol are confirmed in the biochemical study of the drained fluid.
Inclusion criteriaThe inclusion criteria were:
- a)
Cervical thyroid surgery in which minimum surgery consisted of total thyroidectomy.
- b)
Confirmation of the presence of lymphatic fluid in the drain, or accumulated in the surgical bed and obtained through puncture.
- c)
At least one year of follow-up after resolution of the chyle fistula.
The exclusion criteria were:
- a)
Partial thyroid surgery.
- b)
Thyroid surgery at some other centre and without confirmation of the technique used.
- c)
Patient loss to follow-up prior to chyle fistula resolution.
- d)
Patients failing to comply with the treatment indicated for resolution of the chyle fistula.
The treatment indication was based on the timing (early or otherwise) of diagnosis of the fistula and its level of output (low or high).
Conservative chyle fistula management groupInitial conservative management was decided in all patients. Conservative treatment was continued in the case of late fistulas (beyond 48h for our group), fistulas with fluid collection in the neck in the absence of drainage, or fistulas with an output of <300cm3/day.
Treatment consisted of the combination of:
- 1.
The replacement of dietary LCTs by MCTs.
- 2.
Subcutaneous octreotide at doses of 0.1μg/8h.
- 3.
Periodic direct puncture in the case of fistulas with fluid collection in the neck in the absence of drainage.
Treatment was provided on an outpatient basis, except in cases involving drainage or refractory cases, where the patients were admitted to hospital and parenteral nutrition was added.
Surgical chyle fistula management groupSurgery was indicated in patients with fistulas presenting in the first 48h after thyroidectomy and with an output of >300cm3/day. The initial approach was cervical, advantage being taken of the previous incision, so as to detect the location of the leak at thoracic duct level. Once the leak was located, the first option was to ligate the duct, and if this did not prove possible, transfixing sutures were used to leave the zone clear of lymph. In the event of cervical surgical failure or pleural effusion, thoracoscopy was indicated for ligation and sectioning of the thoracic duct at a high thoracic level.
Study variablesThe following variables were studied: (1) the time from thyroid surgery to the appearance of the fistula; (2) daily fistula output; (3) conservative treatment applied (replacement of dietary LCTs by MCTs, total parenteral nutrition [TPN], and periodic direct puncture evacuation); (4) octreotide treatment; (5) surgical indication; (6) surgical particulars in those patients subjected to surgical treatment (surgical approach, incidents, etc.); and (7) the time taken for the resolution of the chyle fistula.
ResultsDescription of the seriesA total of 9 patients with cervical chyle fistula following thyroid surgery were included in the study. All were women, with a mean age of 50±12 years.
All the patients were subjected to surgery for papillary thyroid carcinoma, except one case which corresponded to medullary thyroid carcinoma. All underwent total thyroidectomy and at least one left lateral cervical lymphadenectomy.
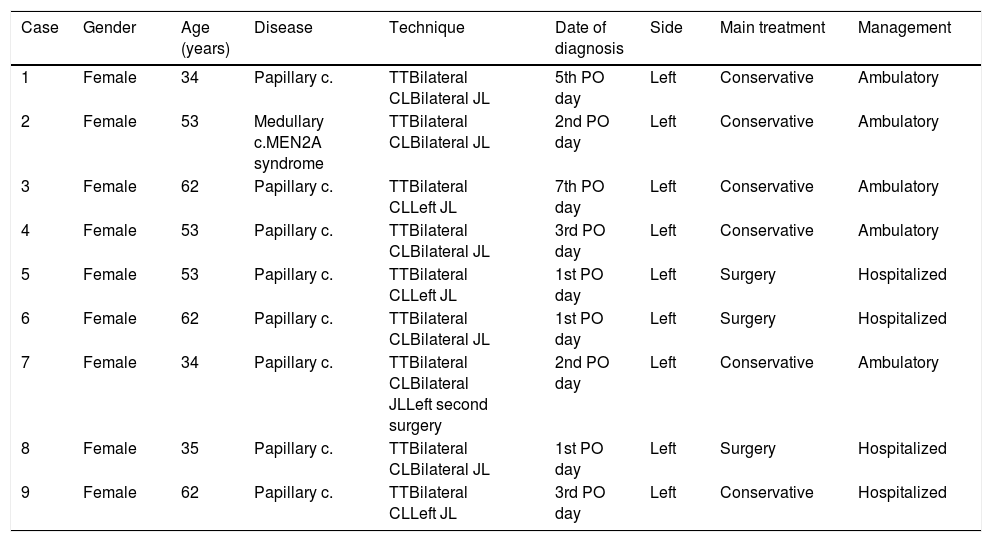
The fistulas were found on the left side in all cases, and all of them were diagnosed in the first 7 days after surgery (Table 1).
Description of the chyle fistula series.
| Case | Gender | Age (years) | Disease | Technique | Date of diagnosis | Side | Main treatment | Management |
|---|---|---|---|---|---|---|---|---|
| 1 | Female | 34 | Papillary c. | TTBilateral CLBilateral JL | 5th PO day | Left | Conservative | Ambulatory |
| 2 | Female | 53 | Medullary c.MEN2A syndrome | TTBilateral CLBilateral JL | 2nd PO day | Left | Conservative | Ambulatory |
| 3 | Female | 62 | Papillary c. | TTBilateral CLLeft JL | 7th PO day | Left | Conservative | Ambulatory |
| 4 | Female | 53 | Papillary c. | TTBilateral CLBilateral JL | 3rd PO day | Left | Conservative | Ambulatory |
| 5 | Female | 53 | Papillary c. | TTBilateral CLLeft JL | 1st PO day | Left | Surgery | Hospitalized |
| 6 | Female | 62 | Papillary c. | TTBilateral CLBilateral JL | 1st PO day | Left | Surgery | Hospitalized |
| 7 | Female | 34 | Papillary c. | TTBilateral CLBilateral JLLeft second surgery | 2nd PO day | Left | Conservative | Ambulatory |
| 8 | Female | 35 | Papillary c. | TTBilateral CLBilateral JL | 1st PO day | Left | Surgery | Hospitalized |
| 9 | Female | 62 | Papillary c. | TTBilateral CLLeft JL | 3rd PO day | Left | Conservative | Hospitalized |
c.: carcinoma; PO: postoperative; TT: thyroidectomy; CL: central lymphadenectomy; JL: lateral jugular lymphadenectomy.
All the patients in the series initially received conservative treatment for the chyle fistula. Of these, 67% (n=6) were treated conservatively with curative intent. Eighty-three percent (n=5) of the cases presented as a sustained fluid collection in the neck, and medical treatment was provided on an ambulatory basis. In the remaining case (17%) the fistula was identified from the neck drain, with a daily output of 200cm3, and treatment was started on an in-hospital basis.
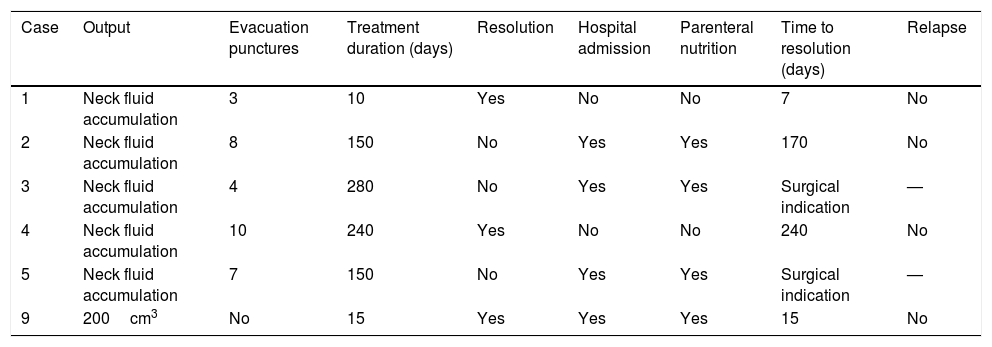
Conservative treatment effectively resolved 50% of the cases (n=3), corresponding to two of the ambulatory treatment patients and the single in-hospital treatment case (Table 2).
Results of conservative management.
| Case | Output | Evacuation punctures | Treatment duration (days) | Resolution | Hospital admission | Parenteral nutrition | Time to resolution (days) | Relapse |
|---|---|---|---|---|---|---|---|---|
| 1 | Neck fluid accumulation | 3 | 10 | Yes | No | No | 7 | No |
| 2 | Neck fluid accumulation | 8 | 150 | No | Yes | Yes | 170 | No |
| 3 | Neck fluid accumulation | 4 | 280 | No | Yes | Yes | Surgical indication | — |
| 4 | Neck fluid accumulation | 10 | 240 | Yes | No | No | 240 | No |
| 5 | Neck fluid accumulation | 7 | 150 | No | Yes | Yes | Surgical indication | — |
| 9 | 200cm3 | No | 15 | Yes | Yes | Yes | 15 | No |
The three cases still unresolved after more than 150 days of ambulatory treatment were admitted to hospital so that medical treatment could be controlled, with no oral intake and the provision of parenteral nutrition. Only one of these cases was resolved (33%), while the remaining two cases were referred to surgery.
No recurrences were recorded in the four cases resolved as a result of medical treatment.
Surgical treatment groupAll patients initially received conservative treatment, after being assigned to one of two subgroups:
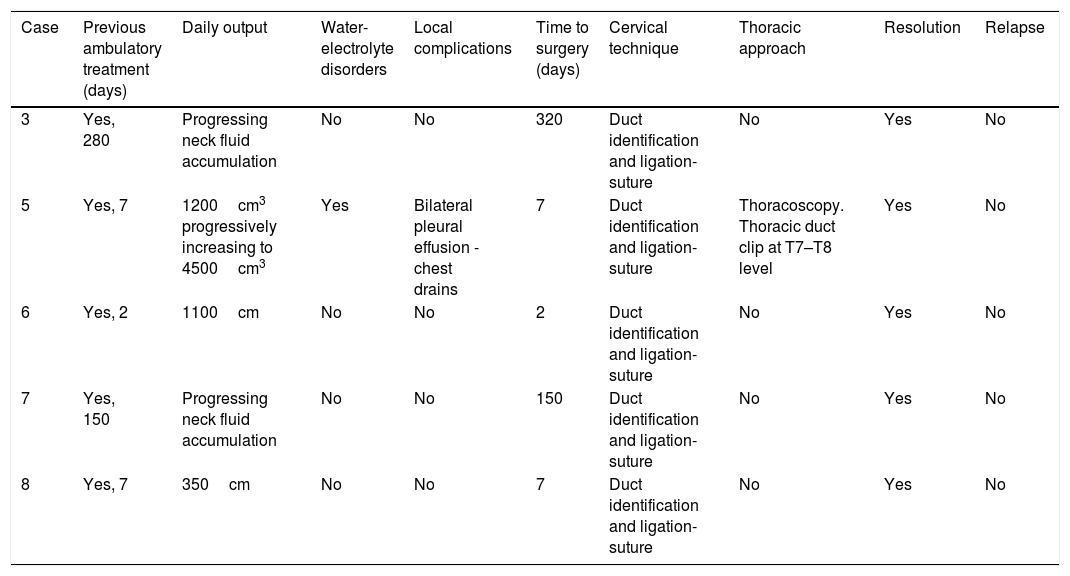
Initial indication of surgical treatmentIn three patients, surgery was indicated as the definitive treatment in the first week after the diagnosis of the chyle fistula. The outputs in these cases were 1200, 1100 and 350cm3 daily, respectively. In all of these patients a cervical approach was adopted, with ligation and transfixing sutures of the thoracic duct. In one of the patients, who presented chylothorax, we performed a thoracoscopy to drain the latter and ligate and section the thoracic duct at the T7–T8 level (Table 3).
Results of surgical treatment.
| Case | Previous ambulatory treatment (days) | Daily output | Water-electrolyte disorders | Local complications | Time to surgery (days) | Cervical technique | Thoracic approach | Resolution | Relapse |
|---|---|---|---|---|---|---|---|---|---|
| 3 | Yes, 280 | Progressing neck fluid accumulation | No | No | 320 | Duct identification and ligation-suture | No | Yes | No |
| 5 | Yes, 7 | 1200cm3 progressively increasing to 4500cm3 | Yes | Bilateral pleural effusion - chest drains | 7 | Duct identification and ligation-suture | Thoracoscopy. Thoracic duct clip at T7–T8 level | Yes | No |
| 6 | Yes, 2 | 1100cm | No | No | 2 | Duct identification and ligation-suture | No | Yes | No |
| 7 | Yes, 150 | Progressing neck fluid accumulation | No | No | 150 | Duct identification and ligation-suture | No | Yes | No |
| 8 | Yes, 7 | 350cm | No | No | 7 | Duct identification and ligation-suture | No | Yes | No |
In all three cases, the resolution proved immediate and no recurrences were observed.
Indication of surgical treatment after the failure of prolonged conservative managementSurgery was indicated in the two patients where conservative treatment failed after 150 and 280 days, respectively. A cervicotomy was performed, with identification in both cases of the point of lymphatic reflux, followed by ligation and transfixing sutures (Table 3).
In both cases the resolution proved immediate and no recurrences were observed.
DiscussionThe presence of a chyle fistula in the postoperative period of neck surgery is usually associated with extensive dissections of the neck region.1–11 The considerable anatomical variation of the cervical thoracic duct exposes it to inadvertent damage, which tends to manifest as the output of a milky-like fluid through the surgical drain in the days following the operation, or as a fluid accumulation after the removal of the drain, as was seen in most of our cases. Chyle fistula usually manifests on the left side, since the thoracic duct drains on that side, though right-side fistulas have also been reported.1,9,10 No right-side chyle fistulas were recorded in our series, however.
Initial treatment consists of drainage of the cavities occupied by lymph, hence the need for periodic puncture evacuation, except in patients with a surgical drain. A diet based on medium chain triglycerides (MCTs) is used because these fats are absorbed directly at portal vein level, thereby reducing the lymphatic flow. In hospitalized patients, total parenteral nutrition reinforces this effect, in addition to correcting the nutritional and metabolic defects secondary to the loss of lymph. Lastly, somatostatin is a polypeptide with neuromodulating action upon the central nervous system that reduces the intestinal absorption of fats, lowers triglyceride concentration in the thoracic duct, and reduces the flow of lymph in the main lymphatic ducts. Moreover, it inhibits gastric, pancreatic and intestinal secretions, as well as bowel motor activity, intestinal absorption and splanchnic blood flow, which favours the healing of the fistula.3,6,12 The mechanism by which somatostatin reduces lymphatic fistula output is not fully clear, though it is probably associated with its inhibitory action upon intestinal motor activity, secretion and absorption, thereby contributing to decreased lymph production.3 Somatostatin analogs such as octreotide are now available and have been shown to be effective in managing chyle fistulas, with the advantage of having a comparatively much longer half life, with no need for continuous intravenous perfusion.3,6,12
The conservative management of chyle fistula comprises all the above measures, which should be introduced in a progressive and stepwise manner. The duration of treatment until either success or failure can be confirmed is highly variable. At present, some authors consider that surgery should be considered if there is no improvement after two weeks of conservative treatment.4,5 Our group takes a more conservative approach. Thus, healing time has ranged from one week to up to 8 months. This latter figure may represent too long a waiting period. However, it should be taken into account that gradual improvement occurs in most cases, and this tends to encourage clinicians to put off surgery. However, it should also be noted that such improvement sometimes does not imply healing, and after a very long and “uncomfortable” treatment period, surgery finally becomes necessary as was shown in our series (Table 3).
Despite the importance of conservative management, it should be borne in mind that the inclusion of somatostatin analogs revolutionized patient care, and that most authors opted for such treatment.13 However, caution is required, and early surgery should be indicated in cases of high fistular output with associated chylothorax, in order to avoid water-electrolyte disorders and respiratory failure.2 Thus, in case 5 of our series (Tables 1 and 3), output progressively increased to 4500cm3, with severe water-electrolyte disorders. Earlier surgery would have prevented such a clinical deterioration of the patient.
Considering the above, surgery should be considered in those fistulas that present high daily outputs despite adequate conservative management (there is no consensus regarding the magnitude of this output, though practically no authors are prepared to wait in the presence of outputs >600cm3), water-electrolyte disorders or complications, whether local (chylothorax, etc.) or systemic (respiratory failure, etc.).
In all cases, octreotide was used and LCTs were replaced by MCTs. Three patients required hospital admission to have parenteral nutrition added, and 66% of the cases healed with conservative treatment.
The prognosis of chyle fistula mainly depends on the mechanical, nutritional and immune disorders resulting from lymph leakage, as well as on complications such as peritonitis or sepsis. A proper therapeutic approach is essential in order to avoid these complications.
In cases where neck surgery is unable to locate the leakage point or the thoracic duct cannot be ligated or sutured, thoracoscopy may prove useful for accessing the thoracic duct.14–16 In our series, thoracoscopy was used in the patient with chylothorax, with the dual aim of draining the latter and ligating the thoracic duct. This strategy proved very effective. However, since neck surgery was involved, it is difficult to know whether the condition was resolved thanks to thoracoscopy or neck surgery, or to both.
A growing number of authors corroborate the observations of our study, demonstrating that the optimum therapeutic approach should be personalized, with a combination of conservative management and surgery adapted to the clinical course of the patient.10,12,17,18 Interventional radiological embolization and sealing of the thoracic duct appears promising, and offers rapid and effective results, though larger series of patients are needed to confirm whether it is truly useful or not.17,19
Lastly, it should be noted that the best preventive measure is careful initial surgery in order to avoid the development of the fistula.11,17 Nevertheless, once chyle fistula has occurred, it should be evaluated and treated in reference units with access to complex medical therapies, interventional radiology, endocrine surgery units experienced in second surgeries of the neck, and thoracic surgery units experienced in thoracoscopy and thoracic duct treatment.11,17
The most controversial scenario, and one where it is difficult to make the right decision, is when chyle fistula persists at neck level as a small fluid accumulation after more than 15–30 days of conservative treatment. Such cases imply long-term management and an uncertain prognosis.10 In these patients, more aggressive options such as surgery or (currently) interventional radiology should be considered. Some authors even advocate other options such as radiotherapy20 or the placement of a continuous negative pressure aspiration system,21 and although the results are encouraging, the experience to date is very limited. Above all, care must be taken with strategies such as radiotherapy, which may cause medium to long term sequelae.22
In conclusion, conservative management proved effective in 66% of the low output chyle fistulas. In high output fistulas, or where conservative treatment is not effective, surgery allows for the effective and rapid resolution of the problem in endocrine surgery units.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: Ríos A, Rodríguez JM, Torregrosa NM, Hernández AM, Parrilla P. Fístula quilosa como complicación de la cirugía tiroidea en patología maligna. Endocrinol Diabetes Nutr. 2019;66:247–253.