Monogenic insulin resistance (IR) syndromes are a group of uncommon conditions associated with lipodystrophy syndromes or hereditary receptor disorders due to mutations of the insulin receptor gene (INS-R), and are often underdiagnosed. These disorders are clinically characterized by hyperinsulinism, IR and altered carbohydrate metabolism. The clinical picture ranges widely from the most serious condition, in the form of Donohue syndrome (DS) or leprechaunism, to milder phenotypes such as Rabson-Mendenhall syndrome (RMS) and type A IR.1,2 The latter is usually diagnosed in adolescence and is characterized by IR, acanthosis nigricans and hyperandrogenism in the absence of obesity or lipodystrophy.3
We report a case of type A IR due to an INS-R mutation that has not been previously described.
A 17-year-old female visited the endocrinology clinic due to gestational diabetes. The family history included a mother with type 2 diabetes mellitus (DM2), as well as a maternal grandmother and three maternal aunts with DM2 and polycystic kidney disease. The patient had been diagnosed with type 1 diabetes (DM1) at 8 years of age on the basis of polyuria, polydipsia and a weight loss of 2kg, with blood glucose 262mg/dl and glycosylated hemoglobin (HbA1c) 10.4%. During childhood she had been admitted on multiple occasions due to poor metabolic control, with a tendency toward poor diet and obesity. Her medical history revealed menarche at age 11, as well as early thelarche, pubarche and axillarche. The laboratory tests showed negative anti-GAD antibodies, and the studies of celiac disease, thyroid hormones, lipid and liver metabolism yielded normal results. The patient was being treated with insulin, and in recent years had presented an HbA1c concentration of 7.6–9.1%. At 14 years and 8 months of age she was admitted due to hypoglycemia (26mg/dl) with clinical signs of dizziness and instability starting two months before, which improved with food intake. Treatment with insulin was therefore discontinued. The physical examination revealed rough skin, hirsutism of the chin, linea alba and buttocks, juvenile acne, and axillary acanthosis. The laboratory tests showed HbA1c: 5.5%; C-peptide: 4.22ng/ml; insulinemia: 45.8μIU/ml (normal range: 2–29.1) and a HOMA index of 10. To complete the study anti-insulin antibodies (which proved negative) and gynecological and renal ultrasound (with normal findings) were requested, together with a genetic study including the HLA system (locus A: A*03, A*24, locus DR: DRB1*11, DRB1*15, DRB3*, DRB5*; locus B: B*07, B*44; locus DQ: DQB1*07(7), DQB1*06 and locus: C*05C*07), normal HNF1 alpha gene and negative MODY panel. The patient continued to experience hypoglycemia episodes without drug treatment and was diagnosed with DM2. At subsequent controls in our pregnancy clinic, she required insulin at high doses from week 9 to the end of pregnancy. After delivery, the patient continued to experience preprandial hypoglycemia episodes together with postprandial hyperglycemia, and signs of hyperandrogenism. With the suspicion of IR syndrome, reinforced by the absence of liver steatosis and lipodystrophy, and with negative insulin receptor antibodies, a genetic study was requested, which detected a mutation in heterozygosis with a c.3831delC deletion in exon 22 of the INSR gene, causing a stop codon. The same mutation was found in her mother. The patient is currently being treated with pioglitazone, after experiencing poor tolerance of the start of metformin, with good glycemic control.
The INS-R gene, located on the short arm of chromosome 19, consists of 22 exons and 21 introns, and is responsible for insulin receptor expression. This surface receptor is composed of two extracellular α subunits and two intracellular β subunits. Any defect in function of the receptor results in IR.1,2
The global prevalence of mutations of the INS-R gene is not known, though the frequency of mutated alleles in the general population of the United States is estimated to be 1:1000–1:2000.4
Despite efforts among investigators to predict the clinical manifestations through structural mutation analysis, no clear genotype-phenotype correlation has been established, and there is diversity in the clinical signs and severity, depending on the residual activity of the INS-R.
Biallelic mutations of the INS-R usually exhibit a recessive hereditary pattern and result in DS (more serious) or RMS (less symptomatic), both conditions being characterized by IR, intrauterine and postnatal growth retardation, and facial dysmorphism. In this context, type A IR syndrome represents the least serious presentation, with considerable clinical diversity. Heterozygous mutations of the subunit or homozygous mutations of the subunit are more severe than heterozygous mutations of the β subunit, which appear to predict a less severe phenotype. Our case was characterized by a heterozygous nonsense mutation located in the β chain, which is associated with a mild phenotype such as that seen in our patient and her first-degree relative.3,5
Patients with type A IR syndrome present normal growth, with no cognitive impairment. The syndrome is usually diagnosed in puberty, and is associated with IR, acanthosis nigricans, hyperinsulinism with fasting hypoglycemia and postprandial hyperglycemia, as well as with hyperandrogenism of variable severity (polycystic ovary syndrome, hirsutism, acne, etc.), which may facilitate its diagnosis in women. Although the clinical picture appears to be mild, a high morbidity should be noted, associated with difficult diabetes control throughout the course of the disorder, and an increased risk of tumor disease.6–9
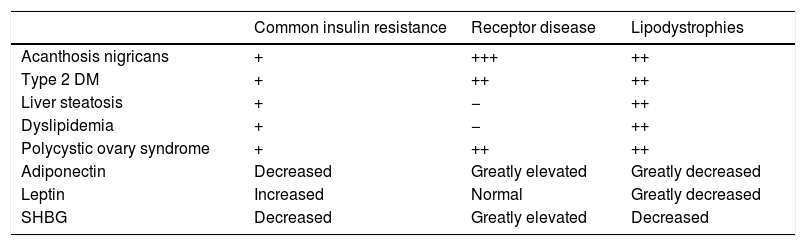
The differential diagnosis versus other forms of IR is sometimes complicated. Initial clinical suspicion is essential, and certain clinical and biochemical differences, such as the absence of dyslipidemia and liver steatosis, and an increase in adiponectin, may be of help8,9 (Table 1).
Differences among common IR, receptor disease and lipodystrophies.
| Common insulin resistance | Receptor disease | Lipodystrophies | |
|---|---|---|---|
| Acanthosis nigricans | + | +++ | ++ |
| Type 2 DM | + | ++ | ++ |
| Liver steatosis | + | − | ++ |
| Dyslipidemia | + | − | ++ |
| Polycystic ovary syndrome | + | ++ | ++ |
| Adiponectin | Decreased | Greatly elevated | Greatly decreased |
| Leptin | Increased | Normal | Greatly decreased |
| SHBG | Decreased | Greatly elevated | Decreased |
DM: diabetes mellitus; IR: insulin resistance; SHBG: sex hormone-binding globulin.
Following the initial suspicion, sequencing of the INS-R gene confirms the final diagnosis.
As regards treatment, most available management options are unable to achieve HbA1c target control. High-dose insulin and oral antidiabetic drugs such as metformin and pioglitazone have been used, though in view of their slight efficacy, new therapies such as metreleptin or IGF-1 have also been evaluated.8
In conclusion, type A IR syndrome is an uncommon condition where, following adequate initial clinical suspicion, it is advisable to confirm the diagnosis through a genetic study. We have described a case associated with a new mutation of the INS-R gene, responsible for the disease. Further studies on these diseases are strongly recommended in order to improve their diagnosis and treatment.
Please cite this article as: López Alaminos ME, Alvarado Rosas KA, Martinez Garcia M, Trincado Aznar P, Alvarez Ballano D. Resistencia a la insulina tipo A, nueva mutación del gen del receptor de la insulina descrita. Endocrinol Diabetes Nutr. 2020;67:611–612.