Riedel's thyroiditis (RT) is a fibrosclerotic disease characterised by thyroid parenchyma replacement by fibrosis, which extends to near structures. It usually presents as a firm anterior cervical mass with gradual development of compressive symptoms, and requires differential diagnosis with malignant disease. RT management focuses on symptom control.1,2
We report the case of a 68-year-old woman who presented with acute dyspnoea, stridor and extreme generalised asthenia, while swimming.
Her personal history included rheumatoid arthritis, mitochondrial myopathy, hiatal hernia and glaucoma. She denied previous knowledge of thyroid disease, dysphonia or dyspnoea, but she did mention having the occasional need to cut smaller food portions while eating due to dysphagia for solids.
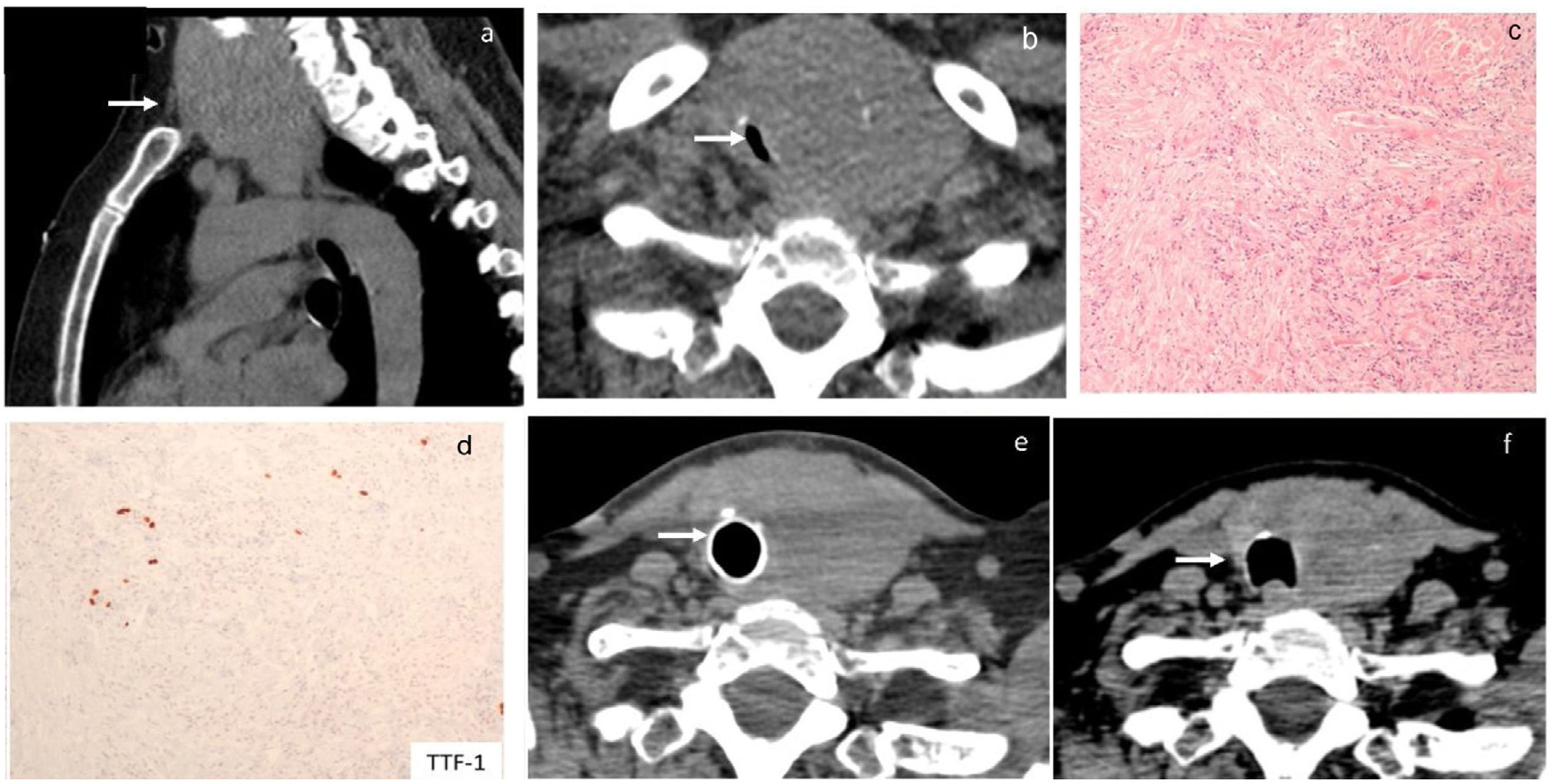
In the emergency department, acute global respiratory failure due to a diffuse goitre, which compromised the tracheal lumen, was identified. She required transient non-invasive ventilation, which restored oxygen saturation, and allowed further oxygen therapy via facial mask. Right tracheal deviation was firstly identified on chest X-ray. A voluminous goitre with intrathoracic extension (Fig. 1a) and a significant reduction in tracheal lumen with a minimal tracheal diameter of 3mm×10mm were identified on a chest computed tomography (CT) scan (Fig. 1b). Surgical treatment was proposed, and an exploratory cervicotomy was performed. During surgery, a fibrous thyroid gland highly adherent to adjacent structures was identified, which suggested a diagnosis of RT. Considering differential diagnosis with anaplastic thyroid carcinoma, intraoperative pathologic examination was performed, which also suggested RT. A decompressive isthmectomy was performed. The histopathologic report described thyroid tissue and surrounding soft tissues with infiltration by spindle cell proliferation, in a stroma with large collagen fibres, moderate lymphoplasmacytic inflammatory infiltrate and low eosinophil count; spindle cells had little nuclear pleomorphism and no mitoses were observed (Fig. 1c). In the immunohistochemistry study, focal positivity was observed for smooth muscle actin; there was negativity for cytokeratins AE1/AE3, TTF-1 (Fig. 1d), thyroglobulin, MDM2, ROS-1, pS100, desmin and CD34; (IgG)4+/IgG+ ratio did not suggest IgG4-associated disease. Analysis by FISH, with probes for detection of structural rearrangements of the ALK gene (Vysis ALK Break Apart FISH Probe Kit) did not reveal the rearrangement of the gene. A diagnosis of IgG4-related thyroid disease was excluded, given the histological and clinical absence of suggestive features. The definitive diagnosis was Riedel's thyroiditis and corticosteroid therapy with intravenous prednisolone (100mg/d) was started. Due to sustained compressive symptoms and oxygen need, a rigid bronchoscopy was performed five days after surgery and documented persistent extrinsic tracheal compression, with 70% lumen reduction. An endotracheal prosthesis restored tracheal lumen calibre and allowed resolution of symptoms. The patient was discharged two days after tracheal prosthesis placement, medicated with prednisolone per os 80mg/d, and did not require oxygen therapy.
At hospital admission, a chest CT scan revealed an exuberant diving goitre (a) with noticeable tracheal lumen reduction to 3mm×10mm (b). The histopathologic report described thyroid tissue and surrounding soft tissues with infiltration by spindle cell proliferation, in a stroma with large collagen fibres and moderate lymphoplasmacytic inflammatory infiltrate; spindle cells have little nuclear pleomorphism and no mitoses are observed (c, d). After 4 months of follow-up endotracheal prosthesis still provided airway safety (e). After 10 months of prednisolone treatment, thyroid size reduction allowed tracheal prosthesis to be safely removed (f).
After one month of follow-up, thyroid parenchyma replacement by fibrosis led to hypothyroidism, which was successfully treated with levothyroxine. Glucocorticoid-induced diabetes was treated with insulin.
At four months of follow-up in the endocrinology clinic, she remained asymptomatic, had good response to thyroid hormone replacement with levothyroxine, and no phosphocalcic metabolism disorders were present. Prednisolone was gradually reduced to 20mg/d. Tracheal prosthesis warranting airway safety and a reduction in thyroid size were documented by CT scan (Fig. 1e). After 10 months of diagnosis and glucocorticoid treatment, further thyroid size involution allowed tracheal prosthesis removal (Fig. 1f) without recurrence of symptoms.
Riedel's thyroiditis was first described in 1896 as a thyroid inflammatory disorder. Incidence is higher in women and in adults aged 30–50 years old, and is estimated to be 1.6 per 100,000 people/year.1,2 Until 2019, 212 cases were reported.3
The pathophysiology of RT remains unclear. Sporadic cases, as well as those associated with multifocal fibrosclerotic disorders or autoimmune diseases such as IgG4-related thyroid diseases, were described.1,4 Clinically, RT usually has an insidious presentation. Patients complain of an anterior cervical mass, which is usually firm with progressive growth, and may be gradually accompanied by compressive symptoms such as dysphagia, hoarseness and dyspnoea.2 Differential diagnoses include anaplastic thyroid carcinoma, primary thyroid lymphoma and fibrosing variant of Hashimoto thyroiditis.1,2
Regarding diagnosis, the following histological criteria are considered2–4: 1. Partial or total fibroinflammatory process of the thyroid; 2. Extension into adjacent tissues; 3. Infiltrates of inflammatory cells, excluding oncocytes, giant cells, lymphoid follicles or granulomas; 4. Occlusive phlebitis; 5. Absence of neoplastic cells.
Despite the majority of patients being euthyroid at diagnosis, 30–40% develop hypothyroidism due to fibrotic infiltration. If the disease extends to the parathyroid glands, hypoparathyroidism may also occur.1,2,4
RT management focuses on symptom control, and glucocorticoids (GC) are the first-line medical treatment. In addition to reducing thyroid size and softening consistency, GC may delay disease progression. Prednisolone is the most used option, with an initial dose between 10 and 100mg/d.3,5
Rituximab may be useful in IgG4-related thyroid diseases.5
Surgical debulking to relieve obstruction and also obtain samples for histological evaluation has been proposed. However, there is a lack of consensus regarding the best intervention. Less extensive surgical approaches, such as isthmectomy, may carry lower risk of iatrogenic hypoparathyroidism and vocal cord palsy.2,3
During follow-up of RT, symptoms, thyroid function and phosphocalcic metabolism should be monitored. One third of patients may develop other fibrosclerotic disorders.5
The reported case is notable for the extremely rare clinical presentation of RT with acute dyspnoea and urgent need to restore the airway. Besides, the need of tracheal prosthesis to achieve symptom control, in addition to the decompressive surgery and corticosteroid treatment, had not been previously reported to our knowledge.
Considering the present case, a therapeutic triad with GC, decompressive surgery and tracheal prosthesis may be a lifesaving approach to consider in RT presenting with acute dyspnoea and significantly compromised airway.
In conclusion, RT is a rare condition which may present with acute dyspnoea and respiratory failure, instead of the usually described progressive growth of cervical mass. Challenges in diagnosis, airway management and symptom control may arise, particularly when the tracheal lumen is significantly compromised.
Ethical approvalEthical approval was granted by the local Ethics Committee.
Informed consentInformed consent was obtained from the patient included in this article.
FundingThis research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of interestNone.