“When you can measure what you are speaking about, and express it in numbers, you know something about it; but when you cannot measure it, when you cannot express it in numbers, your knowledge is of a meagre and unsatisfactory kind”.
Since we have often seen ice cubes in a glass of water, we know about the physical properties of icebergs. We know that only one-eighth of the volume of ice lies above the surface. Therefore, while navigators at sea have a limited and biased vision of icebergs, seeing the enormous mass of ice beneath the surface must offer a totally different (and surely more realistic) impression.
As pointed out by Lord Kelvin, the first scientific principle is to be able to quantify the problem at hand. Such numerical information is provided by epidemiological studies of prevalence and incidence. These two terms are not synonymous. Prevalence refers to the existing number of cases in the population at a given point in time, while incidence refers to the appearance of new cases of the disease in a defined group of subjects during a certain period of time. In view of the longitudinal nature of the studies, detecting incidence is comparatively much more complicated, and quality surveys in this field are scarce.
In 1990, the Institute of Medicine defined care quality as “those healthcare services destined to secure the desired degree of wellbeing for both individuals and populations, in consonance with current professional knowledge”.1 In the same way as the clinical act, medical research – characterized by ever increasingly frenetic activity – seeks to improve health. This requires physicians to continuously keep themselves up to date in order to offer patients the latest advances learned from the library, i.e., quality medicine. However, the step from shelf to clinic must always abide by the classical principle: primum non nocere. This principle implies the need to avoid overdiagnosing (in order to preclude overtreatment), as well as to avoid the opposite. This difficult balance, which is central to precision medicine, is crucial in the management of thyroid cancer patients.2
In recent years, and particularly as a consequence of observations made in South Korea, there has been widespread debate about whether we are facing a thyroid cancer “epidemic” or are actually dealing with a clear example of overdiagnosis.3,4 The data from South Korea indicate that almost 95% of the thyroid cancers detected in that country correspond to indolent cases incapable of causing patient harm.4 It is such lazily reached disease diagnoses and the actions taken as a result that is what we mean by overdiagnosis and overtreatment.4,5 Indeed, such “excessive concern” probably brings us closer to nocere than to quality care.
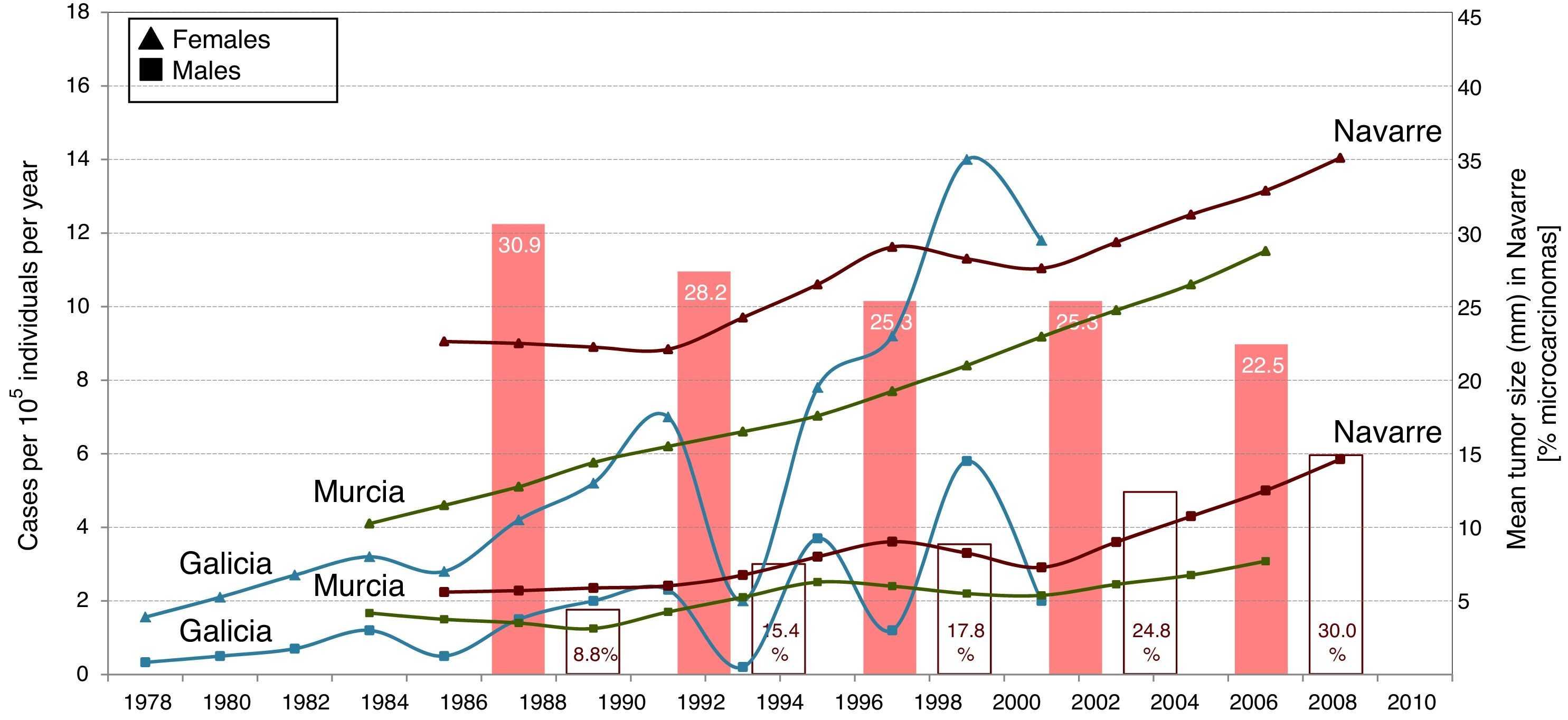
Spain is no exception to this increase in the incidence of thyroid cancer, as evidenced by some studies, of which three deserve specific mention.6–8 Each publication was based on a different method, though to practical effects we can compare the results obtained. Almost 10 years ago, Rego-Iraeta et al. showed the frequency of thyroid cancer to have increased consistently in the region of Galicia in the period 1978–2002.6 Subsequently, Chirlaque et al. obtained similar results in the region of Murcia corresponding to the period 1984–2008.7 Finally, in the present issue of Endocrinología, Diabetes y Nutrición, Rojo et al. describe how the incidence of thyroid cancer increased consistently in the Region of Navarre over a 25 year period (1986–2010).8 The results of these three studies are summarized in Fig. 1. Unfortunately, none of the studies provide data referring to thyroid cancer mortality in their respective regions, which would have allowed us to better know the possible aggressivity of these tumors. Nevertheless, as in most countries, the three Spanish studies coincide in two key aspects. Firstly, the increase in the incidence of thyroid cancer is exclusively attributed to papillary carcinoma; and secondly, the tumors that increase most correspond to microcarcinomas.
Incidence of differentiated thyroid cancer in Spain. The lines (the scale on the left) reflect the increase in incidence (cases per 105individualsyear) in the regions of Galicia,6 Murcia7 and Navarre,8 in both males (□) and females (▵), over one-third of a century. A sustained increase can be observed that, moreover, overlaps among the three studies. The solid columns (the scale on the right) show the mean tumor size (in mm) detected in each 5-year period in the study from Navarre,8 which is seen to gradually decrease. On the other hand, the hollow columns show the percentage of microcarcinomas detected in the same study8 during the same periods of time, and which are seen to gradually increase.
These findings in turn raise a series of questions, including the following three: 1) What is the cause of the increase?; 2) Where will this take us?; and 3) How can we deal with this “epidemic”?
It is admittedly not easy to answer the first question, as there is probably no single explanation. A large and recent study in the United States has shown for the first time that the increase in the incidence of papillary carcinoma is associated with an increase in mortality.9 This implies the existence of new and still little known carcinogenic factors (probably of an environmental nature). However, it is also undoubtedly true that many “occult” indolent cases are being identified which in the past would have gone undetected with the more rudimentary diagnostic tools available at the time (overdiagnosis). We know that thyroid microcarcinomas are identified in 22% of all necropsy studies secondary to death due to any cause.10 The data published by Rojo et al. indicate that the percentage of microcarcinomas with respect to the total cases of thyroid cancer diagnosed in Navarre tripled (from 9% to 30%) between the period 1986–1990 and 2006–2010.8 Returning to the idea of our iceberg, these data suggest that in the past we only saw the part above the surface (one-eighth), but are now seeing something more of what lies below the surface. But obviously we have not yet seen it all. This leads us to our second question, which could also be stated as follows: How much “occult” thyroid cancer is there? How big is the iceberg? The data currently available indicate that with existing diagnostic techniques, the cumulative incidence over a period of 80 years (a human lifetime) suggests a diagnosis of thyroid cancer in approximately one individual out of every 100 (i.e., 1%). This is still far from the 22% found in the necropsy studies. In other words, we still have a wide margin when it comes to incrementing cancer incidence if we insist on diagnosing all that lies occult. And this paves the way to our answering the third question: What is to be done?
On the one hand, much research effort is required to identify and counter the potential carcinogens. On the other hand, it must be admitted that we are currently overdiagnosing thyroid carcinoma. This in turn often leads us to overtreatment. An example of what may constitute an advisable approach comes from the series of 1235 microcarcinomas prospectively subjected to active monitoring (without surgery after diagnosis) in the hospital of Kuma (Japan). In this series, only 5% of the tumors were found to grow more than 3mm; 2% developed locoregional disease; and none gave rise to distant spread.11 These findings are certainly consistent with universal experience, which indicates that over 95% of all microcarcinomas remain for a long time in a quiescent state (as is also evidenced from necropsy studies). The above considerations have recently caused a group of experts to propose a change in how we deal with papillary microcarcinoma: active monitoring (with some conditions) is advised, rather than surgical treatment.12 This daring proposal has been received with some reluctance by other experts, for a number of reasons. Firstly, the outcomes of common practice are very satisfactory. Furthermore, it remains to be established whether the Japanese model is universally applicable. Lastly, we are currently unable to firmly differentiate between indolent and aggressive disease. Indeed, this is possibly the greatest difficulty we face in the management of thyroid cancer. The need for further progress in the field of precision medicine is once again made evident.2
This dilemma is also present in other fields in Oncology. In effect, a similar problem is found in relation to prostate cancer.13 In this case we even distinguish between active monitoring and monitored waiting (observation). The latter entails less intensive follow-up. Over time we will probably also establish distinctions of this kind in the follow-up of thyroid cancer. For the time being, and until we are able to clearly differentiate between indolent and aggressive tumors, we feel the safest strategy to be intelligent adherence to leading guides such as those of the American Thyroid Association,14 the British Thyroid Association,15 or the Sociedad Española de Endocrinología y Nutrición.16
To sum up, there is no problem in thyroid ultrasound explorations being performed as a screening strategy for nodular disease. However, until precision medicine is able to offer improved knowledge regarding the aggressivity of a concrete thyroid nodule, and in order to avoid nocere and improve quality, our recommendation is to limit biopsies to supra-centimeter nodules.
Please cite this article as: Galofré JC. Incidencia de cáncer de tiroides: el descubrimiento del iceberg oculto. Endocrinol Diabetes Nutr. 2017;64:285–287.