In Asturias, where iodine deficiency was eradicated in school children by the year 2000, iodine deficiency persisted in pregnant women, who were recommended to use of iodine supplementation. The aim of this study was to determine the iodine nutrition of pregnant women in our area and whether or not iodine supplements are needed.
Material and methodsThroughout May and June 2013 we studied the iodine nutrition and thyroid function during the first trimester of pregnancy in 173 women in the health area of Oviedo.
ResultsThe median urinary iodine was 197μg/L. Iodinated supplements were used by 47% of women, which had a yoduria median higher than those not taking iodinated supplements (247 vs 138μg/L; p<0.001), and also a higher TSH (2.30 vs 1.94mU/L) although not significantly different. Yoduria was also higher in women who took more than two servings of dairy products (median: 230μg/L) than those who took less (median: 191μg/L). Within the group of women who were not taking iodine supplements, those regularly using iodized salt in the kitchen (47%) had a median urinary iodine concentration of 190μg/L indicating iodine sufficiency.
ConclusionsIodinated supplements seem unnecessary nowadays in pregnant women of Oviedo who regularly take iodized salt and our recommendation in these cases should be to continue the use of iodized salt in the recommended amounts during pregnancy and consume at least two daily servings of milk or dairy products.
En Asturias, donde la deficiencia de yodo fue erradicada en los escolares en el año 2000, persistía una deficiencia de yodo en las mujeres embarazadas, por lo que se les recomendaba la utilización de suplementos yodados. El objetivo de este estudio es conocer la nutrición de yodo de las mujeres embarazadas de nuestra área y la necesidad o no de suplementos yodados.
Material y métodosDurante mayo y junio de 2013 hemos estudiado la nutrición de yodo y la función tiroidea en el primer trimestre del embarazo de 173 mujeres del área sanitaria de Oviedo.
ResultadosLa mediana de la yoduria fue 197μg/L. Tomaban suplementos yodados el 47% de las mujeres, con una mediana de yoduria superior a la de las que no tomaban suplementos yodados (247 vs 138μg/L; < 0,001) y también una TSH superior (2,30 vs 1,94mU/L), aunque no significativamente diferente. La yoduria fue también superior en las mujeres que tomaban más de 2 raciones de productos lácteos (mediana: 230μg/L) que en aquellas que tomaban menos de 2 raciones (mediana: 191μg/L). Dentro del grupo de mujeres que no tomaban suplementos yodados, aquellas que utilizaban habitualmente sal yodada en la cocina (47%), tenían una mediana de yoduria de 190μg/L, indicativa de suficiencia de yodo.
ConclusiónEn la actualidad los suplementos yodados serían innecesarios en las mujeres embarazadas de nuestra entorno que consumen de forma habitual sal yodada y la recomendación en estos casos debería ser la de continuar utilizando la sal yodada en la cantidad recomendada en la gestación, así como consumir al menos dos raciones diarias de leche o productos lácteos.
Iodine deficiency (ID) was documented in Asturias in the school population in the 1980s of the past century.1 After marketing of iodinated salt2 and continuous work by the Department of Endocrinology and Nutrition of Hospital Universitario Central de Asturias and the Department of Health of the Asturias government, iodine deficiency was eradicated from the school population in 2000 as the result of a high consumption rate of iodinated salt.3 However, as in other Spanish regions,4,5 iodine intake was inadequate to cover the increased iodine requirements during pregnancy due to the combination of greater renal loss, placental deiodination, and additional thyroxine requirements by the fetus.6 This is the reason why iodide supplementation is recommended in Spain to all women during pregnancy and lactation.
In recent years, however, increased urinary iodine levels have been found in both schoolchildren and adults.7 These are attributed to increased iodine concentrations in milk.8 On the other hand, administration of iodide supplements to pregnant women has not shown a consistent impact on development of their children.9,10 Because of this, some organizations11 have advised against universal iodine supplementation in pregnant and breast-feeding women, and only recommend use of supplements in those at high risk of inadequate iodine intake or thyroid dysfunction development at these stages. Moreover, some studies have found higher TSH levels and lower thyroid hormone levels in women receiving iodine supplements during pregnancy,12,13 and it has therefore been postulated that supplementation with iodine salts may have an effect contrary to the expected in some women.
In order to ascertain the current nutritional status of pregnant women in our healthcare area, we conducted a study of urinary iodine levels and thyroid function in a sample of women enrolled in their first visit to the healthcare system for pregnancy.
Patients and methodsThe sample consisted of 173 pregnant women from the healthcare area IV of Asturias consecutively enrolled at their first visit to the midwife of their healthcare center on May and June 2013 and who gave their consent to participate in the study.
All women were collected on the following day a random urine sample to measure urinary iodine levels, and were drawn a blood sample to test TSH, free thyroxine (T4), and thyroid peroxidase antibodies (anti-TPO Ab).
Urinary iodine levels were measured using HPLC-ECD (high-performance ion-pair chromatography coupled to electrochemical detection). TSH (normal range [NR], 0.17–4.15mU/L and coefficient of variation [CV], 0.8–2.9%),14 FT4 (NR, 0.99–1.67ng/mL, and CV, 1.8–3.2%) and anti-TPO antibodies (NR, <20U/L) using a chemiluminescence immunoassay of Roche Diagnostics.
A survey was also conducted on use of iodine supplements, iodinated salt, and dairy products. Iodinated salt consumption was considered to be positive when it occurred regularly from at least one year before the recent pregnancy. To estimate consumption of dairy products, subjects were asked about the daily number of glasses of milk and yoghurts taken and the weekly number of cheese servings. A serving was defined as a glass of milk, 2 yoghurts, or 100g of cheese.
SPSS version 15.0 software was used for statistical processing. A Student's t test was used for differences in quantitative variables, an ANOVA test was used for qualitative variables, and Spearman's correlation coefficient was used for bivariate correlations. A Kolmogorov–Smirnov test was used for non-normally distributed variables.
The study was approved by the clinical research ethics committee of Hospital Universitario Central de Asturias.
ResultsMean urinary iodine level was 229.6±162.3μg/L (17–777), with a median of 197μg/L.
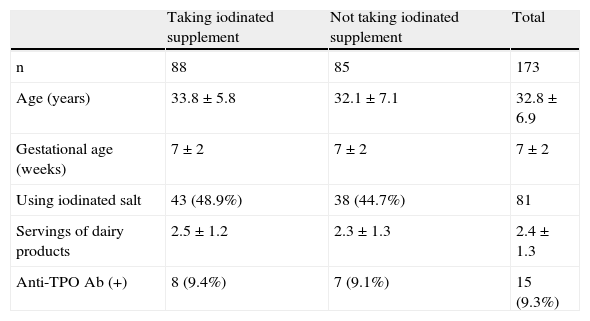
Among the total 173 women, 88 had taken iodinated supplements for at least the past seven days, and 85 were not taking supplements. No differences were seen between the groups in age, presence of anti-TPO Ab, dairy product consumption, or use of iodinated salt (Table 1).
Sample characteristics.
| Taking iodinated supplement | Not taking iodinated supplement | Total | |
| n | 88 | 85 | 173 |
| Age (years) | 33.8±5.8 | 32.1±7.1 | 32.8±6.9 |
| Gestational age (weeks) | 7±2 | 7±2 | 7±2 |
| Using iodinated salt | 43 (48.9%) | 38 (44.7%) | 81 |
| Servings of dairy products | 2.5±1.2 | 2.3±1.3 | 2.4±1.3 |
| Anti-TPO Ab (+) | 8 (9.4%) | 7 (9.1%) | 15 (9.3%) |
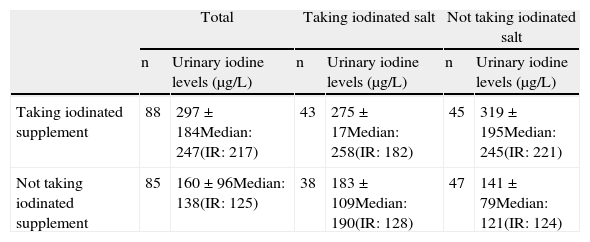
As shown in Table 2, women taking iodinated supplements had significantly higher (p<0.001) urinary iodine levels than those not taking supplements. Median values were 247 and 138μg/L respectively.
Urinary iodine levels as a function of intake of iodinated supplements and routine use of iodinated salt.
| Total | Taking iodinated salt | Not taking iodinated salt | ||||
| n | Urinary iodine levels (μg/L) | n | Urinary iodine levels (μg/L) | n | Urinary iodine levels (μg/L) | |
| Taking iodinated supplement | 88 | 297±184Median: 247(IR: 217) | 43 | 275±17Median: 258(IR: 182) | 45 | 319±195Median: 245(IR: 221) |
| Not taking iodinated supplement | 85 | 160±96Median: 138(IR: 125) | 38 | 183±109Median: 190(IR: 128) | 47 | 141±79Median: 121(IR: 124) |
IR: interquartile range.
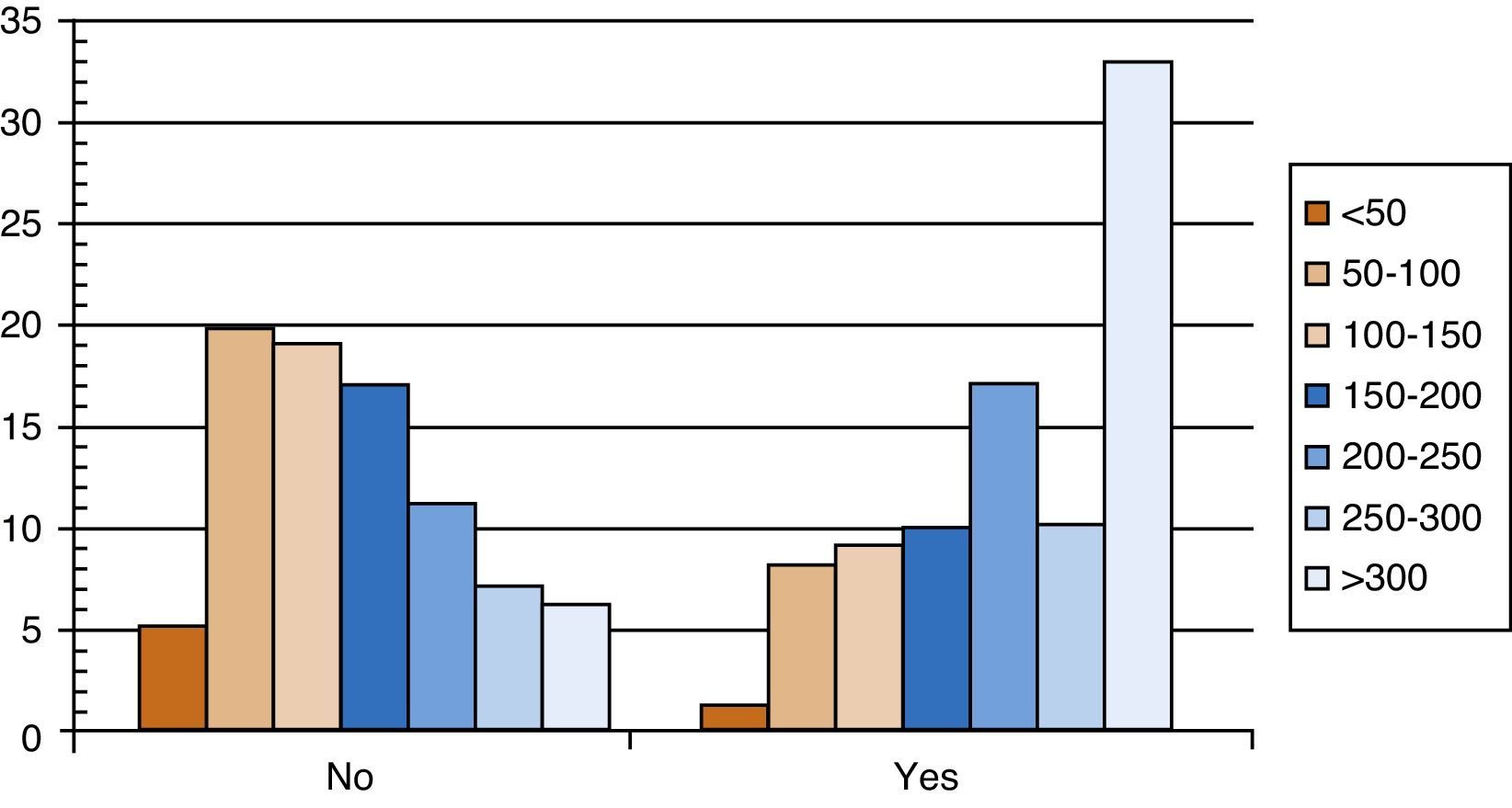
Fig. 1 shows distribution of urinary iodine levels in both groups. It may be seen that, among women taking iodinated supplements, 33 (37.5%) had urinary iodine levels higher than 300μg/L and 12 (13.6%) had levels higher than 500μg/L. Inadequate urinary iodine levels (less than 150μg/L) were found in 20.5% of women taking supplements and in 51.8% of those who did not take them.
Most women (70%) were taking two or more daily servings of dairy products. Dairy product consumption did not correlate with urinary iodine levels, which were however lower (p<0.05) in those taking two or less daily servings (208±145μg/L; median, 191μg/L) as compared to those taking more than two daily servings (250±175μg/L; median, 230μg/L).
After excluding women with anti-TPO Ab, mean TSH levels were 2.13±1.16 mU/L; a trend to higher TSH levels was seen in the group taking supplements, but the difference was not significant (2.30±1.26 vs 1.94±1.04). There was no difference in plasma free T4 levels between the groups (1.18±0.15 vs 1.16±0.15). Among women taking iodinated supplements, 42.5% had TSH levels higher than 2.5mU/L, as compared to only 26.5% of women not taking supplements (p<0.05).
In women not taking iodinated supplements but who routinely used iodinated salt, mean urinary iodine level was 183.1±109.2μg/L, with a median of 190μg/L. Mean urinary iodine level in women using iodinated salt was 140.7±79.2μg/L, with a median of 121μg/L. There was no difference in dairy product consumption between the groups (2.4±1.3 vs 2.2±1.2 servings).
DiscussionIodine is indispensable for formation of thyroid hormones, thyroxine (T4) and triiodothyronine (T3), which are essential for maturation and development of the central nervous system of the fetus.15
Iodine requirements increase by more than 50% during pregnancy because of increased renal iodine clearance and increased needs for thyroid hormone synthesis to cover fetal requirements. Iodine requirements have been estimated at 250μg daily.16 Because of this, even women living in areas with iodine sufficiency are at risk of experiencing iodine deficiency during pregnancy.17,18
Severe iodine deficiency in pregnancy is associated to cretinism, impaired mental development, and other neurocognitive changes in children.19,20 When iodine deficiency is mild or moderate, it has a milder and more subtle impact, but several studies conducted in recent years have reported poorer results in different neurocognitive and school achievement tests in children born to mothers with inadequate iodine nutrition during their pregnancies.21,22
Spain is considered by the World Health Organization (WHO) as a country with no iodine deficiency since 10 years ago.23 Iodine intake was however not sufficient to guarantee adequate iodine nutrition in pregnant women, as shown by the results of studies conducted both in Asturias4 and in other Spanish regions. Median urinary iodine levels were in all these cases lower than 150μg/L, suggesting inadequate iodine intake, except in the mountain area of Catalonia.24 Because of this evidence, the Ministry of Health approved in 2005 marketing of potassium iodide supplements for prophylaxis of iodine deficiency in pregnant women, which were reimbursable by the National Health System,25 and both the Spanish Society of Endocrinology and Nutrition (SEEN) and other scientific societies recommend use of iodinated supplements in pregnant women.
After marketing of iodinated supplements, results of most new studies conducted at different Spanish areas have shown that median urinary iodine levels in the first trimester of pregnancy, although higher than the previous levels, continued to be inadequate26,27; by contrast, iodine sufficiency was already seen in other areas such as Guipuzcoa28 due to high use of iodide supplements. In Asturias, data from 2008 also showed iodine sufficiency, with median urinary iodine levels of 155.7μg/L. Seventy-seven percent of pregnant women reported use of iodinated supplements.29 However, a study conducted in 2010 on women of childbearing age who took no supplements already showed a median urinary iodine level of 169μg/L, only slightly lower than that found in schoolchildren aged 6–14 years, in whom the value was 181μg/L.30
In the current study, conducted during May and June 2013 on women in the Oviedo area during their first trimester of pregnancy, median urinary iodine level seen was 197μg/L, clearly higher than 150μg/L; this was due to the fact that 51% were taking iodinated supplements, and also probably to increased intake of iodine from milk and dairy products, which have been shown in recent years to have a high iodine content in several countries,31 and also in Spain,8 including Asturias.
An analysis of women in this group who took iodinated supplements revealed that a significant proportion had urinary iodine levels higher than 300μg/L, an excessive level according to WHO criteria32; this may be the origin of another finding made in our study: that this group of women had higher TSH levels than those not taking supplements, a fact already reported in other observational studies conducted in Spain33 and Italy.13 In the latter study, authors attributed the finding to a transient phenomenon of thyroid gland stunning, and therefore advised against iodinated supplementation, and recommended that supplementation is started instead several months before pregnancy to avoid a sharp increase in iodine provision during pregnancy.
After dividing the study sample into two groups based on whether or not they were previously taking iodinated supplements, women not taking supplements were seen to have median urinary iodine levels of 121μg/L, lower than recommended. However, women not taking iodinated supplements but routinely using iodinated salt had median urinary iodine levels within the recommended limits (190μg/L); we therefore think that these women would not require iodinated supplements, and a recommendation to continue using iodinated salt would suffice. Iodinated salt used in Spain is among the salts with the greatest iodine contents in Europe, 60ppm, so that adequate iodine intake may be achieved with 3g daily.2 Although no correlation was seen in our study between dairy product consumption and urinary iodine levels, most women were taking two or more servings daily, which is the amount recommended for all pregnant women,34 taking into account that organic milks are poor in iodine.35
The fact that pregnant women who routinely use iodinated salt have an adequate iodine intake should not lead us to forget that only 47% of women in our study used that salt, similarly to what occurs in other Spanish regions.28,36 Public health measures should therefore be implemented to achieve at least 90% consumption of iodinated salt, as recommended by the ICCD-WHO,32 because it is advisable to ensure adequate replenishment of thyroid iodine deposits before pregnancy.
On the other hand, and as recommended by the working group of SEEN,37 epidemiological monitoring of iodine nutrition is indispensable in women of childbearing age because of potential inadvertent changes in iodine contents in diet. Increased urinary iodine levels seen in the current study were due to an inadvertent increase in iodine intake, probably caused by its increased concentration in dairy products during recent years as the result of changes in cattle feed composition. An inadvertent public health success has occurred, similar to that reported in the United Kingdom some years ago.38
It should also be taken into account that some countries which have been considered iodine-sufficient for many years, such as the USA,39–41 Australia,42 or the United Kingdom,43 currently have lower than recommended median urinary iodine levels in pregnant women.
As a conclusion, we think that iodinated supplements would currently be unnecessary in pregnant women in our environment who have routinely used iodinated salt, because their iodine intake with usual diet would be adequate. These women should be advised to continue to use iodinated salt in the amount recommended for pregnancy, and to take at least two daily servings of milk or dairy products (Fig. 1).
Health authorities are obliged to continue to promote use of iodinated salt in diet in order to achieve that all women reach pregnancy under optimal iodine nutrition conditions.
Conflicts of interestThe authors state that they have no conflicts of interest.
Please cite this article as: Menéndez Torre E, Delgado Alvarez E, Rabal Artal A, Suárez Gutiérrez L, Rodríguez Caballero MG, Ares Blanco J, et al. Nutrición de yodo en mujeres embarazadas del área de Oviedo. ¿Es necesaria la suplementación con yodo? Endocrinol Nutr. 2014;61:404–409.