Ganglioneuroma is a benign neoplasm derived from the neural crest that is mainly located in the mediastinal and peritoneal sympathetic ganglia1,2 and, very occasionally, in the adrenal gland.3,4 It usually occurs in children or adolescents, causes no or highly nonspecific symptoms, and is typically a non-secreting tumor.5,6 Among the neuroblastic tumors, ganglioneuroma is the most uncommon, the one with the greatest histological differentiation, and the most benign.
An atypical case of adrenal ganglioneuroma is reported below.
A 60-year-old female patient with high blood pressure attended the gastroenterology department for left abdominal pain irradiating to the back and because of a bitter taste in her mouth. No abnormalities were found in the clinical history, physical examination, and routine laboratory tests. Examination by echoendoscopy revealed a solid mass in the left adrenal gland with ill-defined, irregular contour and hyperechogenic points inside, showing no cystic component and no evident vascularization. No perilesional adenopathies were seen in the celiac trunk, hepatic hilum, or mediastinum. The material collected from two needle passages was not representative of the adrenal gland. A computed tomography (CT) scan of the abdomen showed an apparently solid mass dependent on the left adrenal gland taking up contrast, slightly heterogeneous, and approximately 4.5cm in diameter.
The patient was referred to the department of endocrinology and nutrition, where a full hormone profile and a battery of imaging tests intended to reveal an adrenal incidentaloma were requested.
Endocrine work-up was intended to determine whether the adrenal mass was functioning or not.7,8 Screening was performed for hypercorticoidism, hyperaldosteronism, and pheochromocytoma.3,9 Laboratory measurements included total and 24-hour urinary free cortisol, ACTH, renin, aldosterone, VIP, C-peptide, somatomedin C, LH, FSH, DHEA-s, total and free testosterone, prolactin, catecholamines and their metabolites in plasma and urine, chromogranin A, gastrin, glucagon, and vanillylmandelic acid (VMA). High levels were found of normetanephrine (593; N<444mcg/24h) and dopamine in urine (487; N<390mcg/24h), chromogranin A (279.5; N 19.4–98.1ng/mL), gastrin (459; N<100pg/mL), and VMA (13.9; N 2–9mg/24h). These results were confirmed by subsequent tests. The patient therefore had subclinical hormonal hyperproduction of normetanephrine and dopamine in the urine, chromogranin A and VMA, while all other tested parameters were normal.
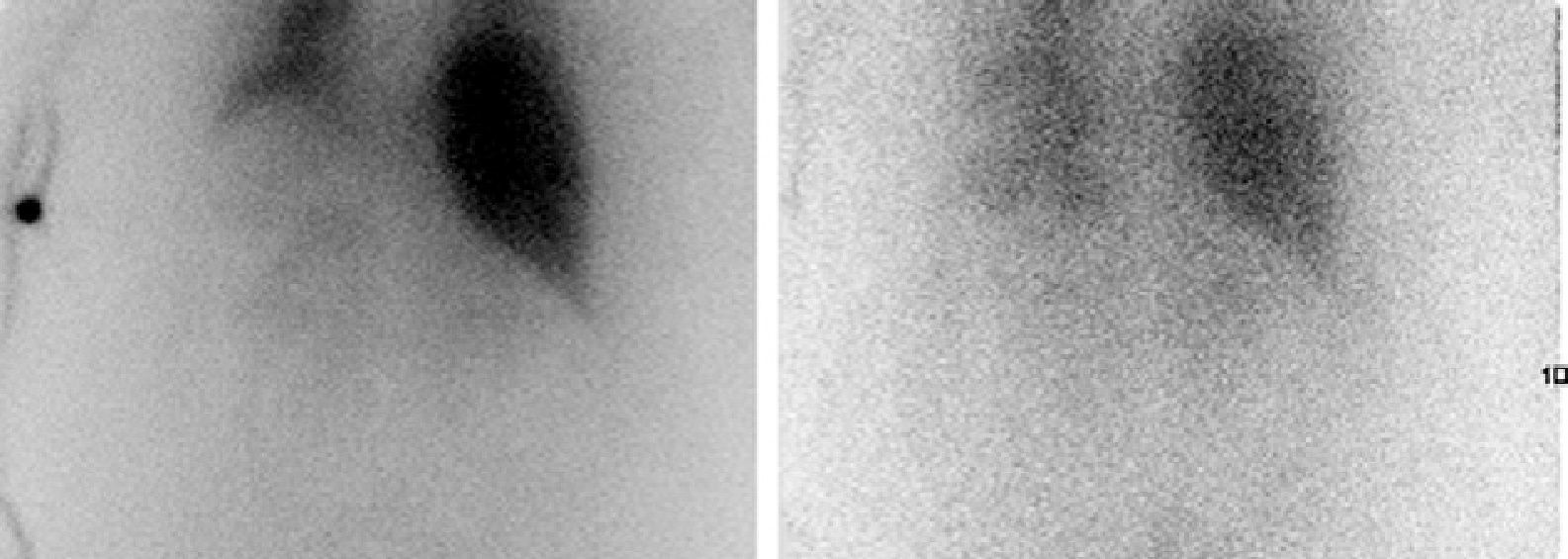
Imaging tests performed to characterize the incidentaloma7 included the following: magnetic resonance imaging, which showed a 4cm lesion in the left adrenal gland with partially defined margins and heterogeneous signal, and with fatty foci inside suggesting the benign nature of the lesion; a characterization study by CT with and without contrast which confirmed a homogeneous adrenal nodule in sections without contrast that was enhanced to 51 HU with an approximate size of 4.3cm×4cm and a relatively homogeneous density, but provided no reliable radiographic data to ascertain its etiology; iodine-131-metaiodobezylguandine scintigraphy, in which focal and pathological radiotracer deposits were not seen in the left adrenal region in the early control, but appeared in the late control, where intense uptake was noted in the above described lesion in the left adrenal region, suggesting adrenergic overexpression in that location (Fig. 1).
Imaging and endocrine work-up revealed the presence of a solid, functioning, large left adrenal mass with possible pheochromocytoma. Because of the size of the lesion, resection of the mass was considered to be indicated, and the patient was referred to the surgical department for surgery.
A left adrenalectomy specimen 7cm×5cm×3cm in size and 75g in weight was sent for histopathological study. Upon sectioning, a partially encapsulated, grayish white tumor lesion of hard consistency and spindle-shaped appearance that occupied 90% of the surface in section and appeared to infiltrate the capsule and pericapsular adipose tissue was identified. The remaining gland parenchyma, orange yellow in color and corresponding to the cortex, which had no gross changes, was pushed away and peripheral to the tumor.
Microscopic examination identified a tumor consisting of aggregates of mature ganglion cells and Schwann cell bundles with occasional lobes of mature adipose tissue located in the periphery of the tumor. The histopathological findings reported were consistent with ganglioneuroma.
Ganglioneuromas are well known neoplasms arising in primary sympathetic neurons of the neural crests which are rarely considered in differential diagnosis of adrenal incidentaloma because they are uncommon in adults.6
Ganglioneuromas are fully differentiated benign tumors that do not contain immature elements and consist of mature ganglion cells and Schwann cells in a fibrous stroma.4,9 They are most commonly located in the sympathetic trunk in the posterior mediastinum and retroperitoneal regions, and only 20–30% occur in the adrenal gland. Other potential sites include the heart, bowel, bone, and parapharyngeal region. Typically, ganglioneuromas do not secrete catecholamines or steroid hormones, and are therefore clinically silent, slow growing lesions3 which are incidentally detected during imaging tests performed for unrelated reasons. Symptoms, depending on the location of the mass, may occasionally occur, including chest pain, difficult breathing, tracheal compression (mediastinum), abdominal pain, distention (retroperitoneal space), or hormone secretion changes4: diarrhea, sweating, high blood pressure, and virilization. Ganglioneuromas may occur at any age, but mostly appear under 20 years of age. While they are benign tumors, malignant transformation and metastasis have been reported in some cases. They may also occur associated with pheochromocytoma. There is no agreement on the surgical indication for adrenal masses, which will depend on lesion size, radiographic characteristics, and functionality. Prognosis after surgery appears to be excellent, and no further therapy is needed.1,3
Although the presentation of this case, i.e. nonspecific symptoms and the incidental finding of a mass in imaging tests performed for another reason, is the most commonly reported in the literature, this was an atypical case of ganglioneuroma. Its atypical features included its location, because only 20–30% of cases occur in the adrenal gland9,10; age at presentation, as these are tumors that may occur in any age group, but more than 80% are reported in patients under 40 years of age, and more than half of these are younger than 20 years; and functionality, because only 30% of ganglioneuromas secrete plasma and urinary catecholamines, and symptoms related to hormone hypersecretion rarely occur in such cases.5 In this case, endocrine tests showed high levels of chromogranin A, VMA, normetanephrine, and dopamine in the urine. Adrenal mass biopsy should not be performed at the least suspicion of pheochromocytoma or without previously ruling out high catecholamine levels, considerations which were transmitted to the gastroenterology department. Imaging tests were inconclusive and so provided no reliable data for establishing the etiology. Only scintigraphy showed in the late control a strong uptake by the mass suggesting adrenergic overexpression.
In this case, hormone and imaging tests not only did not allow us to discriminate between incidentally found adrenal lesions or to make a firm diagnosis, but they also suggested a wrong diagnosis (pheochromocytoma). Pathological examination of the surgical specimen established the final diagnosis of ganglioneuroma.
Please, cite this article as: Alramadan M, et al. Ganglioneuroma suprarrenal: un reto diagnóstico. Endocrinol Nutr. 2013;60:272-3.