To ascertain the socioeconomic impact of diabetes, it is essential to estimate overall costs, including both direct and indirect costs (premature retirements, working hours lost, or sick leaves). This study analyzed indirect costs for temporary disability (TD) due to diabetes and its complications in Spain in 2011 by assessing the related ICD-9 MC codes.
Material and methodFor this purpose, the number of TD processes and their mean duration were recorded. The indirect costs associated to loss of working days were also estimated.
ResultsIn 2011, diabetes and its complications were related to 2567 TD processes, which resulted in the loss of 154,214 days. In terms of costs, this disease represented for Spanish public health administrations an expense of 3,297,095.3 €, with an estimated cost per patient and year of 141 €.
ConclusionsThese data suggest an urgent need to devise plans for prevention and early diagnosis of diabetes and its complications, as well as programs to optimize the available health care resources by creating multidisciplinary teams where occupational medical services assume an important role. A decrease in absenteeism would result in benefits for diabetic patients, society overall, and companies or public institutions.
Para conocer el impacto socioeconómico de la diabetes es indispensable realizar el cálculo de los costes globales, de modo que se incluyan los gastos directos, pero también los indirectos (jubilaciones prematuras por enfermedad, pérdida de horas de trabajo o bajas laborales). El presente trabajo estudió los costes indirectos por incapacidad temporal (IT) derivados de la diabetes y sus complicaciones en España en el año 2011 mediante la evaluación de los códigos CIE-9 MC relacionados con esta patología.
Material y métodoPara ello, se registraron el número de procesos de IT y su duración media. Además, se estimó el coste asociado a la pérdida de días laborales.
ResultadosLa diabetes y sus complicaciones se relacionaron con 2.567 procesos de IT en 2011 que dieron lugar a una pérdida de 154.214 días. Traducido en costes, esta enfermedad supuso para las administraciones públicas de salud en España un gasto de 3.297.095,3 €, siendo el coste por IT estimado por paciente y año de 141€.
ConclusionesEstos datos hacen pensar en la necesidad urgente de planes de prevención y diagnóstico temprano de la diabetes y sus complicaciones, así como programas de optimización de los recursos sanitarios existentes, mediante la formación de equipos multidisciplinares en los que los servicios de medicina del trabajo cobran un papel importante. La disminución del absentismo laboral redundaría en un beneficio para los pacientes diabéticos, la sociedad en general y las empresas e instituciones públicas.
The St. Vincent Declaration, a document that would serve as a basis for the subsequent creation in each country of programs for the prevention and management of diabetes mellitus (DM) was issued in 1989.1 Despite all efforts, two decades later DM is considered to be the greatest worldwide epidemic of the 21st century.2 The most recent data of the International Diabetes Federation estimate an overall prevalence of the disease of 366 million people in 2011, i.e. 8.3% of the world population.2 This represents a dramatic increase from its first publication in 2000, which reported a worldwide prevalence of 151 million people. Changes in the dietary habits and lifestyle of the population (sedentary life, obesity, smoking, high-calorie diets) and increased life expectation are some of the reasons accounting for this increase. Overall prevalence is even higher in Spain, where it is estimated that 13.8% of the population has metabolic changes related to DM. Only 7.8% of the people affected are aware of having the disease.3,4
The socioeconomic impact of diabetes is not only due to its increasing prevalence. Diabetic patients usually experience acute complications. However, in patients with DM, the mortality risk increases due to chronic complications, including diabetic retinopathy, coronary artery disease, kidney disease, neuropathy, stroke, and peripheral vascular disease.5
All of this makes diabetes a very significant problem for health care services. In Spain alone, the direct financial costs derived from diabetes have been estimated to range from 533 to 1585 € per patient, per year.6 Indirect costs such as work time loss, temporary disability (TD) benefits, or early retirement because of the disease (permanent disability), all of them related to a loss of production of goods and services, should also be added. Estimating the indirect costs is complex because they depend, for example, on variables including the occupational sector to which the worker belongs, his/her job, income-tax group, etc. Few studies have estimated the indirect costs of diabetes in Spain, and the resulting range of values is even more variable, from 719 to 2270 € per patient, per year.7–9
This study calculated the indirect costs of TD derived from diabetes and its complications in Spain, for which complete data on workdays lost during 2011 were used.
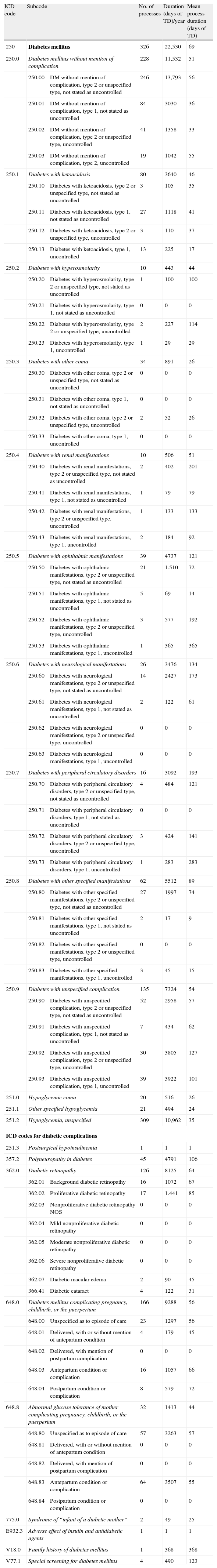
Subjects and methodsFrom January to December 2011, a review was conducted of data from the Ministry of Health and Social Security and from Spanish autonomous communities based on codes from the 9th revision of the International Classification of Diseases (ICD-9-CM) related to DM and its complications (Table 1).10 The following ICD-9 codes were collected: 250, 250.1, 250.2, 250.3, 250.4, 250.5, 250.6, 250.7, 250.8, 250.9, 251.0, 251.1, 251.2, 251.3, 357.2, 362.0, 648.0, 648.8, 775.0, E932.3, V18.0, V77.1.
Diabetes mellitus and complications – ICD codes. Impact on temporary disability in 2011.
| ICD code | Subcode | No. of processes | Duration (days of TD)/year | Mean process duration (days of TD) | |
| 250 | Diabetes mellitus | 326 | 22,530 | 69 | |
| 250.0 | Diabetes mellitus without mention of complication | 228 | 11,532 | 51 | |
| 250.00 | DM without mention of complication, type 2 or unspecified type, not stated as uncontrolled | 246 | 13,793 | 56 | |
| 250.01 | DM without mention of complication, type 1, not stated as uncontrolled | 84 | 3030 | 36 | |
| 250.02 | DM without mention of complication, type 2 or unspecified type, uncontrolled | 41 | 1358 | 33 | |
| 250.03 | DM without mention of complication, type 2, uncontrolled | 19 | 1042 | 55 | |
| 250.1 | Diabetes with ketoacidosis | 80 | 3640 | 46 | |
| 250.10 | Diabetes with ketoacidosis, type 2 or unspecified type, not stated as uncontrolled | 3 | 105 | 35 | |
| 250.11 | Diabetes with ketoacidosis, type 1, not stated as uncontrolled | 27 | 1118 | 41 | |
| 250.12 | Diabetes with ketoacidosis, type 2 or unspecified type, uncontrolled | 3 | 110 | 37 | |
| 250.13 | Diabetes with ketoacidosis, type 1, uncontrolled | 13 | 225 | 17 | |
| 250.2 | Diabetes with hyperosmolarity | 10 | 443 | 44 | |
| 250.20 | Diabetes with hyperosmolarity, type 2 or unspecified type, not stated as uncontrolled | 1 | 100 | 100 | |
| 250.21 | Diabetes with hyperosmolarity, type 1, not stated as uncontrolled | 0 | 0 | 0 | |
| 250.22 | Diabetes with hyperosmolarity, type 2 or unspecified type, uncontrolled | 2 | 227 | 114 | |
| 250.23 | Diabetes with hyperosmolarity, type 1, uncontrolled | 1 | 29 | 29 | |
| 250.3 | Diabetes with other coma | 34 | 891 | 26 | |
| 250.30 | Diabetes with other coma, type 2 or unspecified type, not stated as uncontrolled | 0 | 0 | 0 | |
| 250.31 | Diabetes with other coma, type 1, not stated as uncontrolled | 0 | 0 | 0 | |
| 250.32 | Diabetes with other coma, type 2 or unspecified type, uncontrolled | 2 | 52 | 26 | |
| 250.33 | Diabetes with other coma, type 1, uncontrolled | 0 | 0 | 0 | |
| 250.4 | Diabetes with renal manifestations | 10 | 506 | 51 | |
| 250.40 | Diabetes with renal manifestations, type 2 or unspecified type, not stated as uncontrolled | 2 | 402 | 201 | |
| 250.41 | Diabetes with renal manifestations, type 1, not stated as uncontrolled | 1 | 79 | 79 | |
| 250.42 | Diabetes with renal manifestations, type 2 or unspecified type, uncontrolled | 1 | 133 | 133 | |
| 250.43 | Diabetes with renal manifestations, type 1, uncontrolled | 2 | 184 | 92 | |
| 250.5 | Diabetes with ophthalmic manifestations | 39 | 4737 | 121 | |
| 250.50 | Diabetes with ophthalmic manifestations, type 2 or unspecified type, not stated as uncontrolled | 21 | 1.510 | 72 | |
| 250.51 | Diabetes with ophthalmic manifestations, type 1, not stated as uncontrolled | 5 | 69 | 14 | |
| 250.52 | Diabetes with ophthalmic manifestations, type 2 or unspecified type, uncontrolled | 3 | 577 | 192 | |
| 250.53 | Diabetes with ophthalmic manifestations, type 1, uncontrolled | 1 | 365 | 365 | |
| 250.6 | Diabetes with neurological manifestations | 26 | 3476 | 134 | |
| 250.60 | Diabetes with neurological manifestations, type 2 or unspecified type, not stated as uncontrolled | 14 | 2427 | 173 | |
| 250.61 | Diabetes with neurological manifestations, type 1, not stated as uncontrolled | 2 | 122 | 61 | |
| 250.62 | Diabetes with neurological manifestations, type 2 or unspecified type, uncontrolled | 0 | 0 | 0 | |
| 250.63 | Diabetes with neurological manifestations, type 1, uncontrolled | 0 | 0 | 0 | |
| 250.7 | Diabetes with peripheral circulatory disorders | 16 | 3092 | 193 | |
| 250.70 | Diabetes with peripheral circulatory disorders, type 2 or unspecified type, not stated as uncontrolled | 4 | 484 | 121 | |
| 250.71 | Diabetes with peripheral circulatory disorders, type 1, not stated as uncontrolled | 0 | 0 | 0 | |
| 250.72 | Diabetes with peripheral circulatory disorders, type 2 or unspecified type, uncontrolled | 3 | 424 | 141 | |
| 250.73 | Diabetes with peripheral circulatory disorders, type 1, uncontrolled | 1 | 283 | 283 | |
| 250.8 | Diabetes with other specified manifestations | 62 | 5512 | 89 | |
| 250.80 | Diabetes with other specified manifestations, type 2 or unspecified type, not stated as uncontrolled | 27 | 1997 | 74 | |
| 250.81 | Diabetes with other specified manifestations, type 1, not stated as uncontrolled | 2 | 17 | 9 | |
| 250.82 | Diabetes with other specified manifestations, type 2 or unspecified type, uncontrolled | 0 | 0 | 0 | |
| 250.83 | Diabetes with other specified manifestations, type 1, uncontrolled | 3 | 45 | 15 | |
| 250.9 | Diabetes with unspecified complication | 135 | 7324 | 54 | |
| 250.90 | Diabetes with unspecified complication, type 2 or unspecified type, not stated as uncontrolled | 52 | 2958 | 57 | |
| 250.91 | Diabetes with unspecified complication, type 1, not stated as uncontrolled | 7 | 434 | 62 | |
| 250.92 | Diabetes with unspecified complication, type 2 or unspecified type, uncontrolled | 30 | 3805 | 127 | |
| 250.93 | Diabetes with unspecified complication, type 1, uncontrolled | 39 | 3922 | 101 | |
| 251.0 | Hypoglycemic coma | 20 | 516 | 26 | |
| 251.1 | Other specified hypoglycemia | 21 | 494 | 24 | |
| 251.2 | Hypoglycemia, unspecified | 309 | 10,962 | 35 | |
| ICD codes for diabetic complications | |||||
| 251.3 | Postsurgical hypoinsulinemia | 1 | 1 | 1 | |
| 357.2 | Polyneuropathy in diabetes | 45 | 4791 | 106 | |
| 362.0 | Diabetic retinopathy | 126 | 8125 | 64 | |
| 362.01 | Background diabetic retinopathy | 16 | 1072 | 67 | |
| 362.02 | Proliferative diabetic retinopathy | 17 | 1.441 | 85 | |
| 362.03 | Nonproliferative diabetic retinopathy NOS | 0 | 0 | 0 | |
| 362.04 | Mild nonproliferative diabetic retinopathy | 0 | 0 | 0 | |
| 362.05 | Moderate nonproliferative diabetic retinopathy | 0 | 0 | 0 | |
| 362.06 | Severe nonproliferative diabetic retinopathy | 0 | 0 | 0 | |
| 362.07 | Diabetic macular edema | 2 | 90 | 45 | |
| 366.41 | Diabetic cataract | 4 | 122 | 31 | |
| 648.0 | Diabetes mellitus complicating pregnancy, childbirth, or the puerperium | 166 | 9288 | 56 | |
| 648.00 | Unspecified as to episode of care | 23 | 1297 | 56 | |
| 648.01 | Delivered, with or without mention of antepartum condition | 4 | 179 | 45 | |
| 648.02 | Delivered, with mention of postpartum complication | 0 | 0 | 0 | |
| 648.03 | Antepartum condition or complication | 16 | 1057 | 66 | |
| 648.04 | Postpartum condition or complication | 8 | 579 | 72 | |
| 648.8 | Abnormal glucose tolerance of mother complicating pregnancy, childbirth, or the puerperium | 32 | 1413 | 44 | |
| 648.80 | Unspecified as to episode of care | 57 | 3263 | 57 | |
| 648.81 | Delivered, with or without mention of antepartum condition | 0 | 0 | 0 | |
| 648.82 | Delivered, with mention of postpartum complication | 0 | 0 | 0 | |
| 648.83 | Antepartum condition or complication | 64 | 3507 | 55 | |
| 648.84 | Postpartum condition or complication | 0 | 0 | 0 | |
| 775.0 | Syndrome of “infant of a diabetic mother” | 2 | 49 | 25 | |
| E932.3 | Adverse effect of insulin and antidiabetic agents | 1 | 1 | 1 | |
| V18.0 | Family history of diabetes mellitus | 1 | 368 | 368 | |
| V77.1 | Special screening for diabetes mellitus | 4 | 490 | 123 | |
DM: diabetes mellitus; TD: temporary disability.
Information about the number of processes for TD related to the above codes and the mean duration of each process, as well as total days lost, was reviewed. Cost was established using an approximate and minimum calculation based on the cost/day marked by the minimum interprofessional salary (MIS) in Spain. The MIS is published annually by the Spanish Government in a Royal Decree that establishes the minimum amount to be received by a worker for his/her legal workday, regardless of sex and age and of whether they are permanent, casual, or temporary workers. The MIS for 2011 was 641.40 € per month, 21.38 € per day, and 8979.60 € per year, but it should be taken into account that the actual figures will always be higher than the MIS.
To make a comparison with the overall cost, total TD processes whose benefits were incurred by the National Social Security Institute (INSS), according to 2011 data published by the Ministry of Labor, were taken as the basis. To calculate costs in relation to the total, the overall expenses incurred by the INSS and derived from TD for all diseases in the same period were considered. Although contributing companies were excluded, both the expenses directly paid by social security and those paid by employers were included.
Estimate per patient and year was made by taking into account the official population figures resulting from the review of local censuses as of January 1st 2011 by the National Statistics Institute,11 which found that the Spanish population was 47,190,473. Based on the known 8% prevalence of diabetes in the population, it was estimated that 3,775,238 people were suffering from diabetes in Spain in 2011. The cost per patient and year was calculated in order to compare the result of this study to the three studies available in the literature.7–9
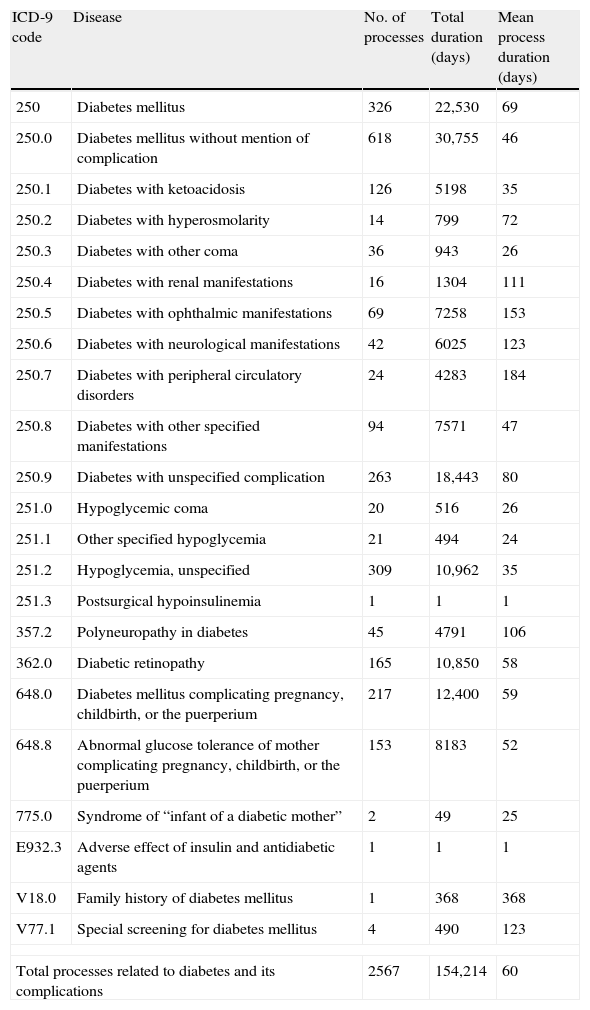
ResultsA total of 22 codes and 58 subcodes of the ICD-9 related to DM and its complications were selected. Table 2 shows the impact on TD of each ICD code selected. Overall, DM and its complications resulted in 2567 TD processes during 2011, with a total loss of 154,214 workdays and a mean duration of 60 days/process.
Impact of temporary disability derived from diabetes and its complications in Spain during 2011.
| ICD-9 code | Disease | No. of processes | Total duration (days) | Mean process duration (days) |
| 250 | Diabetes mellitus | 326 | 22,530 | 69 |
| 250.0 | Diabetes mellitus without mention of complication | 618 | 30,755 | 46 |
| 250.1 | Diabetes with ketoacidosis | 126 | 5198 | 35 |
| 250.2 | Diabetes with hyperosmolarity | 14 | 799 | 72 |
| 250.3 | Diabetes with other coma | 36 | 943 | 26 |
| 250.4 | Diabetes with renal manifestations | 16 | 1304 | 111 |
| 250.5 | Diabetes with ophthalmic manifestations | 69 | 7258 | 153 |
| 250.6 | Diabetes with neurological manifestations | 42 | 6025 | 123 |
| 250.7 | Diabetes with peripheral circulatory disorders | 24 | 4283 | 184 |
| 250.8 | Diabetes with other specified manifestations | 94 | 7571 | 47 |
| 250.9 | Diabetes with unspecified complication | 263 | 18,443 | 80 |
| 251.0 | Hypoglycemic coma | 20 | 516 | 26 |
| 251.1 | Other specified hypoglycemia | 21 | 494 | 24 |
| 251.2 | Hypoglycemia, unspecified | 309 | 10,962 | 35 |
| 251.3 | Postsurgical hypoinsulinemia | 1 | 1 | 1 |
| 357.2 | Polyneuropathy in diabetes | 45 | 4791 | 106 |
| 362.0 | Diabetic retinopathy | 165 | 10,850 | 58 |
| 648.0 | Diabetes mellitus complicating pregnancy, childbirth, or the puerperium | 217 | 12,400 | 59 |
| 648.8 | Abnormal glucose tolerance of mother complicating pregnancy, childbirth, or the puerperium | 153 | 8183 | 52 |
| 775.0 | Syndrome of “infant of a diabetic mother” | 2 | 49 | 25 |
| E932.3 | Adverse effect of insulin and antidiabetic agents | 1 | 1 | 1 |
| V18.0 | Family history of diabetes mellitus | 1 | 368 | 368 |
| V77.1 | Special screening for diabetes mellitus | 4 | 490 | 123 |
| Total processes related to diabetes and its complications | 2567 | 154,214 | 60 | |
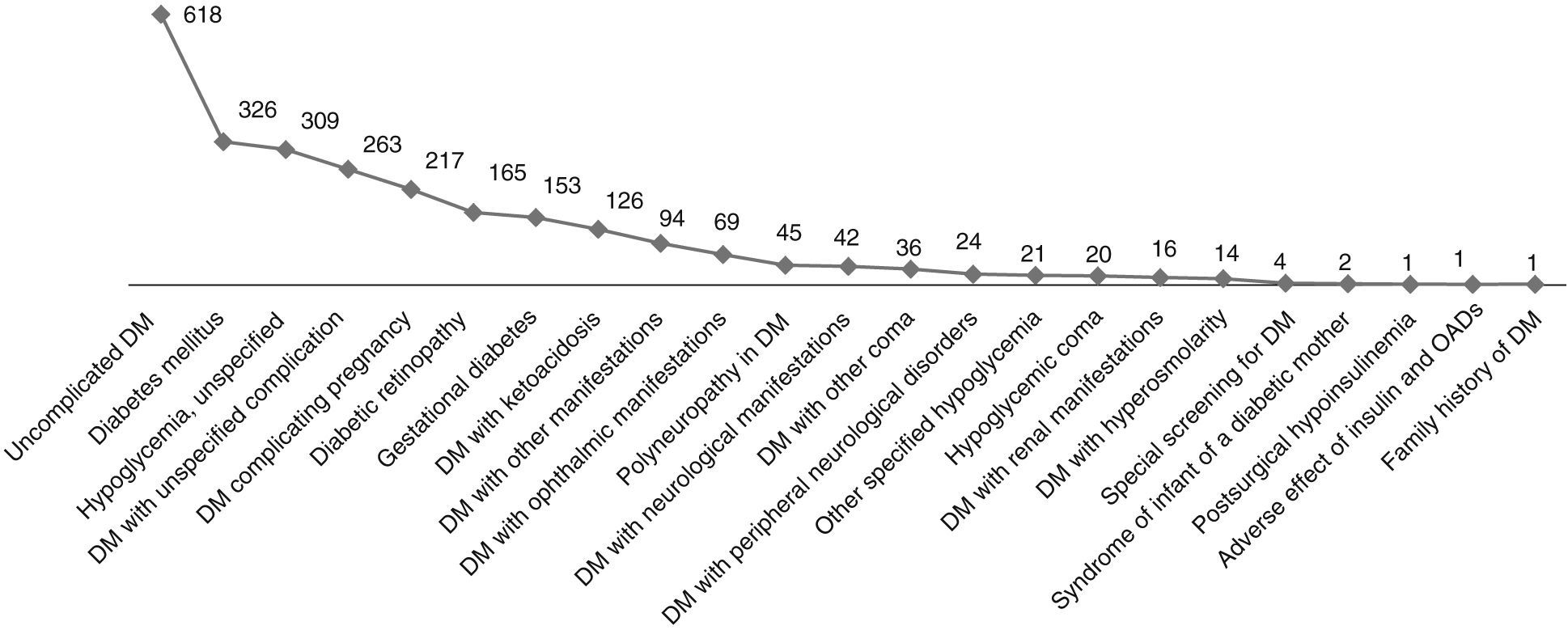
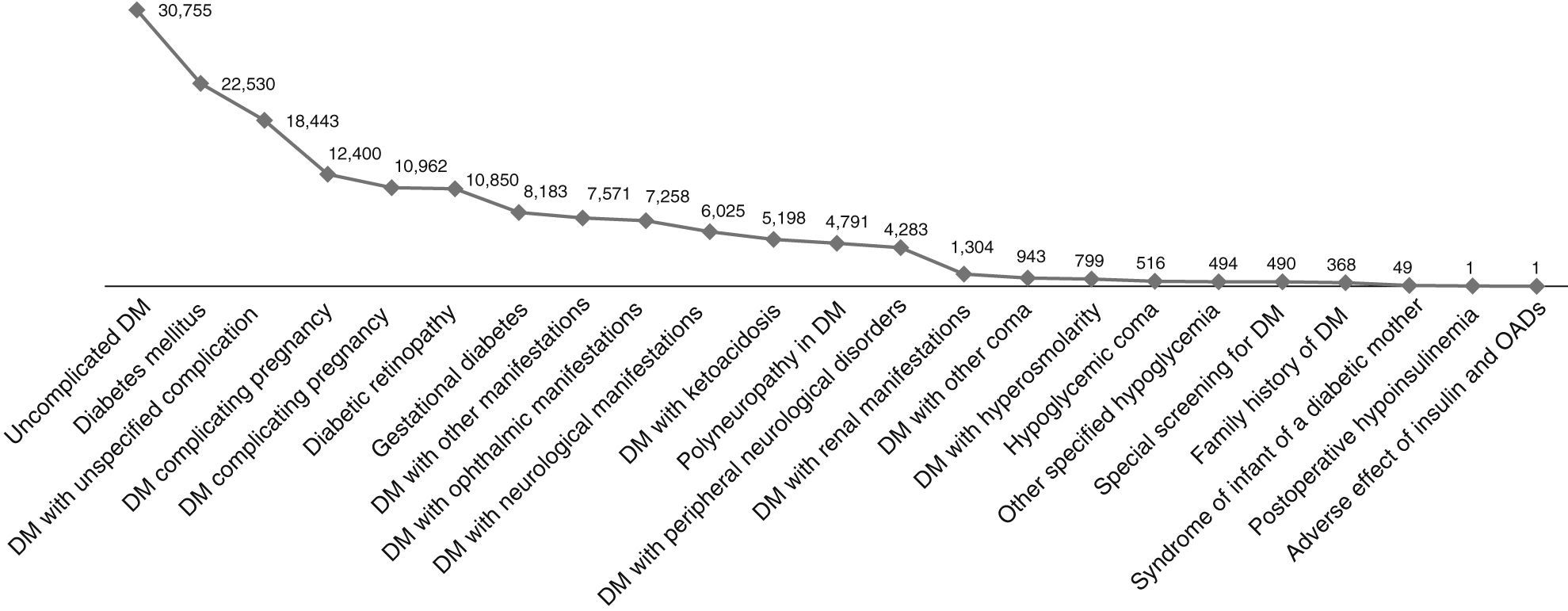
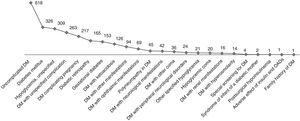
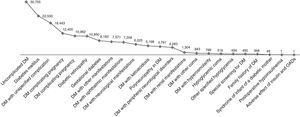
The codes which referred to diabetes without mention of complication, diabetes proper, and non-specific hypoglycemic episodes were the three most common causes of TD, with respectively 618, 326, and 309 processes during 2011 (Fig. 1). As regards the total duration of the processes, uncomplicated diabetes and DM proper ranked first and second with 30,755 and 22,530 days respectively, while DM with unspecified complication ranked third with 18,443 days/year (Fig. 2). Episodes of unspecified hypoglycemia (code 251.2) were associated with the loss of 10,962 workdays per year. The longest mean duration of the process was seen for ICD-9 codes V18.0 and 250.7, family history of diabetes mellitus and diabetes with peripheral circulatory disorders, with 368 and 184 days respectively.
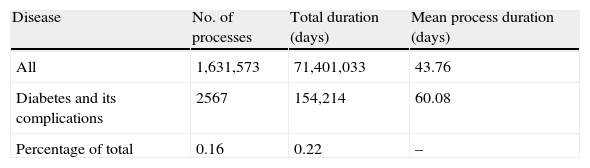
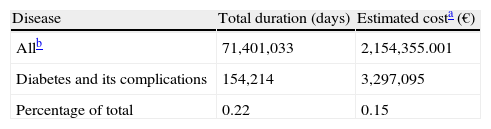
In 2011, a total of 1,631,573 TD processes for all diseases were recorded in Spain, causing the loss of 71,401,033 workdays. TD resulting from DM and its complications accounted for 0.16% of all processes and for 0.22% of workdays lost (Table 3). If these data are translated into costs based on the MIS for 2011 (21.38 €/day), the estimated indirect expenses for the INSS for workdays lost related to TD caused by all diseases amounted to 2,154,355,000.78 €, with DM and its complications accounting for 0.15% of the total cost of TD processes in Spain in 2011 (Table 4). Based on the prevalence of diabetes in Spain in 2011 (3,775,238 patients), the cost of the disease was 141 €/year per patient.
Impact of temporary disability due to diabetes and its complications as compared to all diseases in Spain during 2011].
| Disease | No. of processes | Total duration (days) | Mean process duration (days) |
| All | 1,631,573 | 71,401,033 | 43.76 |
| Diabetes and its complications | 2567 | 154,214 | 60.08 |
| Percentage of total | 0.16 | 0.22 | – |
*Data from processes with discharge occurring during 2011.
Cost estimation is indispensable in order to assess the true dimension of a health problem. Goetzel et al. listed the most costly medical conditions in the United States in 2003. In their list, DM ranked third after angina pectoris and hypertension.12 When speaking about medical costs, most studies focus on the direct costs derived from health care and drug purchase, but the evidence shows that direct costs represent only a small fraction of total health-related costs.12–15
As previously stated, the calculation of indirect costs is complex because the factors affecting the results are multiple and very difficult to assess, and the literature available on studies estimating indirect costs derived from diabetes is scarce, and even less data are available about the TD costs incurred by social security.7–9
However, we think that even assuming some calculation bias that may decrease the reliability of the results, the study of the indirect costs from TD may be important in order to appreciate the socioeconomic impact of this disease. We therefore conducted a prevalence study to estimate TD costs from diabetes and its complications based on data recorded by the INSS in Spain in 2011. This type of study, although difficult to apply to economic evaluation, can serve as a guide for decision making because it allows for the quantification of the total resources invested in disease management.
According to our results, in 2011 there were 2567 TD processes for diabetes and its complications, resulting in a total loss of 154,214 workdays per year. The total cost of TD calculated for diabetes was 3,297,095.3 €/year, or 141 €/year per patient. These data agreed with the results of the Ballesta et al. study, which reported a cost of 156 €/year per patient, although their study only quantified patients with type 2 DM.8 According to these authors, the total indirect costs of type 2 diabetes amounted to 1843 €/year per patient.8 Another study reported a much lower total indirect cost of type 2 DM, 571 €/year, of which only 54 €/year per patient were attributed to costs due to work time loss.7 This study was based on data for 1999 collected in the autonomous community of Andalusia only, which may explain the substantial difference. The indirect cost estimated for type 1 DM was 1258 €/year per patient,9 but this study did not break down the costs corresponding to early retirement, workdays lost, or sick leave, and we cannot therefore match it with our data.
Special attention must be paid to the fact that one of the main reasons for TD is hypoglycemic episodes, of which 309 were recorded in 2011. One of the biggest challenges in the management of diabetic patients is to achieve the prevention of this common adverse effect, which may result in decreased treatment compliance.16,17 Some organizations therefore recommend that clinicians place special emphasis on the prevention of these events.18 According to the literature available, hypoglycemic episodes were associated with an indirect cost per patient ranging from 132 to 876 €/year according to the study.17,19,20
Bearing in mind these data, it might be interesting to study the most important causes of TD associated with DM, as well as their relationship with certain impact factors such as social, occupational, or economic changes and to watch their changes over a period of time.
In recent years, European agencies have shown increasing concern about health inequalities between the different socioeconomic groups. The most disadvantaged population usually has poorer living and working conditions and health habits, and is therefore exposed to higher morbidity and mortality risks.21 The impact on health is added to the social factor, because the measurement of the prevalence of some chronic diseases, including diabetes, shows much higher rates in the populations with the lowest economic levels.22 The overall economic impact of health inequality in Europe has been estimated at 141 billion euros.22
The results show an evident need for reinforcing the schemes for the prevention and management of diabetes and its complications. In 2007, the Spanish Ministry of Health issued a document, Strategy for Diabetes in the National Health System, which discussed the different strategic lines of action for the countrywide coordination of health prevention and promotion plans, for adequate diagnostic means for the early detection of diabetes, and for effective treatments of the disease.23 One of the mainstays is the education of the population on healthy lifestyle habits.
On the other hand, the early detection and treatment of diabetes require agreed protocols and clinical and care collaboration by the different health care professionals. Increasing emphasis is being placed on the optimization of the health care resources available in order to cope with the economic costs of diabetes. One option would be to include the occupational medicine team in the multidisciplinary team. These specialists have access to a wide population encompassing most socioeconomic groups and are also trained to promote the occupational adaptation of the workers to their workplaces while living with the disease.
In conclusion, in order to decrease the financial burden of this disease and to achieve a general social benefit and a particular benefit for diabetic patients, it is necessary that population-wide prevention programs be implemented, with special emphasis being placed on the most socioeconomically disadvantaged groups, which have been shown to have an increased prevalence of some chronic diseases, such as diabetes, and their complications. Such plans should provide information and training to these populations on healthy lifestyle habits. They must also guarantee the multidisciplinary coordination of health care teams, in which occupational physicians have a particularly relevant role to play because, in addition to promoting the prevention and early diagnosis or treatment of this metabolic disease and its complications, they are able to implement individualized occupational reinsertion plans for workers with diabetes.
FundingThis study was funded by Novo Nordisk Pharma S.A.
Conflicts of interestThe authors state that they have no conflicts of interest.
The authors thank Irantzu Izco-Basurko and Teresa Hernando (COCIENTE S.L.) for their collaboration in the preparation of this manuscript.
Please cite this article as: Vicente-Herrero MT, Terradillos García MJ, Capdevila García LM, Ramírez Iñiguez de la Torre MV, López-González ÁA. Costes por incapacidad temporal en España derivados de la diabetes mellitus y sus complicaciones. Endocrinol Nutr. 2013;60:447–455.