Exposure of the body to large amounts of iodine sometimes causes thyroid function changes, and may result in both hyperthyroidism and hypothyroidism. Potential iodine sources include dietary supplements, drugs, iodine-rich antiseptic solutions, or iodinated contrast agents used for imaging tests.1 Povidone iodine is a non-toxic, low cost chemical agent with high germicidal power which is widely used in hospital practice as a disinfectant and sterilizing agent. The case of a patient who experienced subclinical hyperthyroidism after repeated topical administration of iodine is reported below.
This was a 39-year-old male with Cacchi–Ricci disease. This condition, also known as medullary sponge kidney, is an uncommon congenital disease consisting of the cystic malformation of distal collecting tubules and usually causes recurrent urinary tract infection and renal stones. The patient was admitted for elective ureterorenoscopy with left lithotripsy, performed uneventfully. After surgery, however, he experienced septic and hemorrhagic shock that required admission to the ICU. Fluid therapy was started, followed by an infusion of norepinephrine 0.58μg/kg/min due to persistent hypotension. Because of the critical condition of the patient despite the actions taken, urgent left nephrectomy was required, as well as arteriography with urgent embolization for stump bleeding after nephrectomy.
High-dose catecholamines were maintained for two weeks, and the dose was tapered after patient stabilization. As the result of the administration of high doses of vasoactive drugs over a long time period, ischemic lesions developed in both feet, requiring the daily application of povidone iodine for periods ranging from 60 to 90min. The patient stayed at the ICU for 26 days and was later transferred to the hospitalization ward. Evaluation by the nutritional department was requested. The patient had lost 20% of his usual weight (75kg) and had an estimated weight of approximately 60kg (a body mass index [BMI] of 19.6kg/m2) and anthropometric parameters (mid-upper arm circumference [MUAC], tricipital fold [TF], and arm muscle circumference [AMC]) below the 10th percentile. A physical examination revealed marked muscle atrophy and cachexia, with no edema. Blood tests showed decreased visceral protein levels (albumin, 2.2g/dL; total protein, 8.2g/dL; transferrin, 82mg/dL) and malnutrition parameters (total cholesterol, 130mg/dL; lymphocyte count, 1.6×103/μL) with no thyroid function impairment (TSH, 3.280mU/L [0.350–4.940mU/L]; free T4, 1.23ng/dL [0.70–1.48ng/dL]). Acute, severe mixed malnutrition was diagnosed.
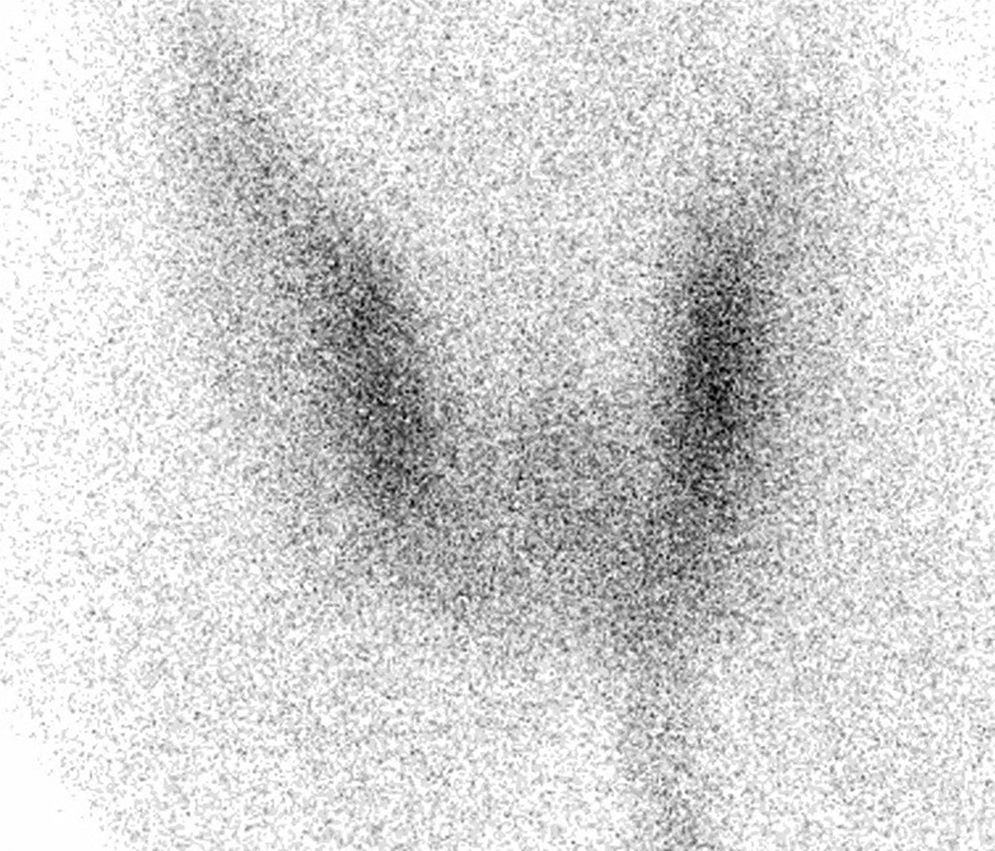
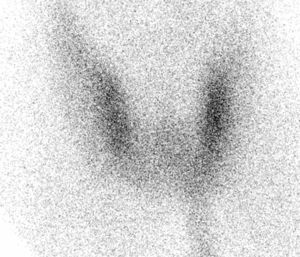
Subsequently, the patient was regularly monitored at the clinic for approximately one year, during which he experienced a gradual improvement in his nutritional status and recovered his usual weight. However, routine tests performed 6 months after hospital discharge showed the following levels: TSH, 0.003mU/L (0.350–4.940mU/L); free T4, 1.42ng/dL (0.70–1.48ng/dL), and free T3, 3.38pg/mL (1.70–3.70pg/mL). There was no associated clinical evidence of low thyroid function. This finding, consistent with subclinical hyperthyroidism, persisted over time. The patient had no family or personal history of thyroid disease, thyroid gland palpation revealed no goiter or nodules, thyroglobulin antibodies were slightly positive (11.89U/mL, 0.05–6U/mL), and peroxidase antibodies were negative. A thyroid ultrasound examination was normal. A thyroid scan with technetium 99m (Fig. 1) showed low thyroid uptake, which was attributed to repeated application of povidone iodine to the ischemic lesions of the feet. The use of povidone iodine was discontinued, and chlorhexidine was used instead. The patient showed a favorable course, with a normalization of TSH levels two weeks after iodine exposure was stopped (TSH, 0.784mU/L; free T4, 0.95ng/dL; and free T3, 2.27pg/mL).
The minimum recommended iodine intake is 150μg/day.2 Exposure to iodine overload causes thyroid self-regulation, consisting of transient decreases in iodine organification and thyroid hormone synthesis (the Wolff–Chaikoff effect). A escape phenomenon occurring at 2–4 weeks normalized hormonal production. Iodine excess may, however, also cause hyperthyroidism (the Jod–Basedow effect) due to thyroid disease hyperproduction and sudden release in response to the administration of large amounts of iodine. This most commonly (but not only) affects people with prior thyroid disease such as endemic goiter, toxic multinodular goiter, or iodine deficiency.3
However, iodine overload is an uncommon cause of hyperthyroidism. A detailed clinical history is therefore essential to detect the condition, and should include data on the use of drugs or dietary supplements4 with high iodine contents, the use of antiseptic solutions such as povidone iodine, or imaging tests with contrast agents. Most cases of iodine-induced hyperthyroidism are self-limited and resolve when exposure ceases.5
Tu sum up, a case of subclinical hyperthyroidism induced by excess topical iodine is reported in a patient with no prior thyroid disease. The condition resolved after povidone iodine was replaced by a iodine-free antiseptic solution. The use of iodinated antiseptics is a widespread practice in hospitals, especially for patients undergoing surgery or with ulcers of both arterial and venous origin.6 In cases with long-term exposure, potential thyroid dysfunction should be considered because, as in the reported cases, it may not be exceptional even in the absence of a history of thyroid disease.
Please cite this article as: Burchés-Feliciano MJ, Argente-Pla M, García-Malpartida K, Rubio-Almanza M, Merino-Torres JF. Hipertiroidismo inducido por yodo tópico. Endocrinol Nutr. 2015;62:465–466.