We report the case of a 37-year-old female patient who two years previously had been diagnosed with a 3-mm cystic microprolactinoma after routine laboratory tests revealed a prolactin level of 68ng/mL (normal, 2.4–25ng/mL). The patient had not experienced any prior menstrual changes, galactorrhea, or neurological symptoms. Cabergoline (0.5mg/week) was administered with a good biochemical response. However, tumor size increased in the first six months of treatment to 7.9mm×5mm×5mm, and then remained stable for the following six months. Some months after this last radiographic control, cabergoline was discontinued due to pregnancy, and levothyroxine (50μg/day) was added for secondary hypothyroidism (TSH 1.74mU/L [normal: 0.35–4.9mU/L] and free T4 0.65ng/dL [normal: 0.7–1.5ng/dL]).
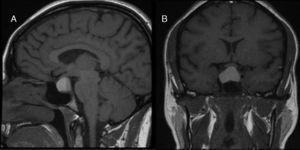
The patient attended the emergency room of our hospital at 24 weeks of pregnancy complaining of continuous retro-orbital headache and decreased visual acuity in the right eye for approximately 10 days. Pituitary MRI performed based on a clinical suspicion of pituitary apoplexy (PA) showed a cystic pituitary lesion 15mm×15mm×22mm in size with serohematic content and an extrasellar component compressing the central portion of the optic chiasm (Fig. 1). The results of a complete blood count, general chemistry, and coagulation tests were normal, and the serum PRL level was 64.5ng/mL. The ophthalmology department confirmed the decrease in visual acuity in the right eye (0.4/1), and also detected inferior temporal quadrantanopia in the same eye. Treatment was restarted with dopamine agonists (bromocriptine 2.5mg/day), and surgery was decided in agreement with the neurosurgery department and based on the decision taken by the patient herself. Surgery was performed through an endoscopic transsphenoidal approach with no complications. The histological report confirmed that the tumor was a pituitary adenoma with densely granulated cells secreting PRL.
(A) T1-weighted sagittal MRI image showing a sellar lesion with suprasellar extension with a fluid-fluid level suggesting bleeding in different evolutionary stages. (B) T1-weighted coronal MRI image showing a markedly hyperintense sellar lesion with suprasellar extension related to bleeding in contact with the optic chiasm.
After surgery, drug treatment with bromocriptine, hydrocortisone, and levothyroxine was maintained until the end of pregnancy. Visual acuity and campimetry findings normalized. During the remainder of her pregnancy, the patient was jointly monitored by the departments of obstetrics, neurosurgery, and endocrinology and nutrition. An elective cesarean section was performed at 37 weeks of pregnancy, and a healthy male infant was delivered (Apgar 10/10). Hormone replacement therapy was discontinued after delivery based on a normalization of pituitary function. MRI has not shown tumor remnants since then.
Drug therapy is the treatment of choice for prolactinomas.1,2 Bromocriptine is recommended during pregnancy because of the wide experience that has been accumulated in using this drug. When women with prolactinoma want to become pregnant, PRL levels in the normal range and a tumor size less than 10mm are recommended to prevent complications. In the event of a microprolactinoma, when pregnancy is confirmed, a discontinuation of drug treatment is recommended because of the estimated 2.2–5% risk of growth during pregnancy. Drug maintenance is however advised in macroprolactinoma, particularly in invasive tumors or tumors close to the optic chiasm.
In the reported cases, prolactinoma size a few months before pregnancy was less than 10mm, and PRL levels were normal. It could therefore be considered an adequate response to discontinue dopamine agonists once pregnancy had been confirmed. However, the following factors should have been taken into account before a decision was reached as to whether to continue or discontinue drug treatment:
- 1.
the tumor was a cystic microprolactinoma, a type of adenoma related to a lower response to treatment with dopamine agonists.1,3
- 2.
Adenoma size had increased despite treatment with dopamine agonists, although its growth had subsequently stabilized.1,3
- 3.
De novo TSH deficiency was diagnosed at the start of pregnancy, and should have raised the alert of a potential tumor growth.
PA results from bleeding or hemorrhagic infarction in a pituitary tumor, and is a potentially serious condition. It may represent the first manifestation of a macroadenoma or microadenoma, and occurs in both functioning and non-functioning tumors. PA has been related to diabetes mellitus, intracranial hypertension, functional pituitary tests, and the use of bromocriptine and anticoagulants. The occurrence of PA is very rare in pregnancy, and few cases have been reported in patients with microprolactinomas.4–8
Treatment of PA should be individualized.9,10 The few cases of PA reported during pregnancy have been treated both conservatively and with surgery, with good results irrespective of the option selected.11,12 In the case reported, because of visual symptoms and patient desire, as well as the availability of a team of experienced neurosurgeons, surgery was performed with an excellent result.
In conclusion, we think that in cases similar to the one reported (women with cystic microprolactinoma and/or with no adequate tumor size reduction despite treatment with dopamine agonists), the continuation of drug treatment during pregnancy and monitoring similar to that recommended for pregnant women with macroprolactinoma should be considered. If PA occurs during pregnancy, given the lack of consensus regarding its treatment, this should be decided upon only after the evidence provided by the series reported, the tolerability of oral medication, the opinion of patients and relatives, and the surgical experience of neurosurgeons at the hospital have all been taken into consideration.
FundingNone.
Conflicts of interestNone of the authors has conflicts of interest.
We thank the departments of neurosurgery, obstetrics, and endocrinology and nutrition.
Please cite this article as: Querol Ripoll R, Cámara Gómez R, del Olmo García M, Simal Julián JA, Merino Torres JF. Apoplejía hipofisaria en gestante con microprolactinoma quístico. Endocrinol Nutr. 2015;62:200–202.