Pituitary apoplexy (PA) is a life-threatening, acute clinical syndrome caused by pituitary gland hemorrhage and/or infarction. A diagnosis of PA requires a high suspicion index, and computed tomography (CT) allows for diagnosis in less than 30% of cases, although a sellar mass may be seen in more than 80%.1
On the other hand, gonadotropin-releasing hormone (GnRH) agonists have become a common treatment for patients with prostate cancer, breast cancer, uterine myoma,2 endometriosis, or early puberty.
These drugs stimulate gonadotropic cells of the adenohypophysis and may induce the growth of adenoma cells,3 and also PA, a very uncommon condition.3 Since Ando et al. reported the first case in 1995,4 there have been reports of at least another 14 patients.2
The case of a 77-year-old male diagnosed with prostatic adenocarcinoma T2cN0M0 who was prescribed treatment with tryptorelin 22.5mg by the intramuscular route every six months is reported. One hour after administration of the first dose, the patient experienced sudden moderate frontal headache associated with nausea and vomiting.
Initial neurological examination was completely normal. Urgent CT of the head revealed a previously unknown sellar lesion, 20 by 25mm in size, extending to the suprasellar area and the right cavernous sinus, consistent with uncomplicated pituitary macroadenoma. Based on a clinical suspicion of PA, treatment was started with intravenous glucocorticoids after blood sampling for hormone tests.
Twelve hours after hospital admission, the patient experienced diplopia and palpebral ptosis in the right eye consistent with incomplete involvement of the third right cranial nerve, with no vision impairment in confrontation perimetry, nor with impaired consciousness.
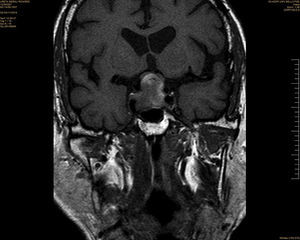
Magnetic resonance imaging (MRI) of the pituitary gland showed significant pituitary enlargement with high signal foci on T1-weighted images and low signal foci on T2-weighted images suggesting bleeding, as well as nodular 25mm uptake in the right half of the pituitary gland consistent with an underlying adenoma (Fig. 1).
Hormone test results were as follows: ACTH, 6.9pmol/L (normal: 2–12); cortisol, 652nmol/L (normal: 155–678); GH, 0.30μg/L (normal: <3.5); IGF-I, 4.7nmol/L (normal: 4.7–22.3); TSH, 1.86mIU/L (normal: 0.48–4.36); FT4, 17.5pmol/L (normal: 9.7–30.9); prolactin, 24mIU/L (normal: 113–200); testosterone, 3.5nmol/L (normal: 7.6–23); FSH, 5.9IU/L (normal: 1.5–6.8); LH, 3.6IU/L (normal: 1.5–6.8).
Transsphenoidal surgery with a complete resection of the pituitary lesion was performed. The pathological study revealed infracted pituitary tissue with abundant necrosis and inflammatory infiltrate consistent with a diagnosis of PA. Pituitary hormone tests performed two months after surgery showed persistent hypoprolactinemia, increased hypogonadotropic hypogonadism, which was mainly attributed to apoplexy and, partly, also to surgery, because the drug could not have acted on a pituitary gland severely compromised by the hemorrhagic complication. A partial corticotropic deficiency that required replacement therapy was also found.
In cases reported in the literature of PA after the administration of GnRH agonists,2 all patients had pituitary macroadenomas. The condition occurred in the first 4h after drug administration in 53% of patients. Significantly, 14/15 patients were male, although this could be related to the more frequent prescription of the drug to patients with prostate cancer. The only case reported in a woman occurred after treatment as a preparation for oocyte donation.2–5 In 9/15 patients, PA occurred following the administration of leuprolide, and only one case was reported following the use of triptorelin.2–6 Headache was the first manifestation in all patients, with a subsequent occurrence of visual impairment, ophthalmoplegia, decreased consciousness, or hypopituitarism.2
The pathophysiology of PA mediated by GnRH agonists is unknown, but the temporal relationship of the condition with drug administration strongly suggests a causal relationship.7 Factors attributed include tumor size or intrasellar pressure. As symptoms started in some patients within 24h of drug administration, but up to 10 days later in other patients, Guerra et al.8 suggested a biphasic phenomenon.
In cases where the condition occurs a few minutes or hours after drug administration, cell division could not induce a significant tumor growth in such a short time. It has been suggested that a combination of cell degranulation and metabolic hyperactivity inducing ischemia in a poorly perfused adenomatous pituitary tissue could occur in these patients.8
In the group of patients with a later start, it has been suggested that pituitary ischemia and bleeding risk could be related to increased intrasellar pressure caused by the adenoma. In addition, the drug stimulates LH secretion, which leads to the growth/division of the adenoma, which is supplied by an abnormal capillary network probably insufficient in the face of increased metabolic demand, thus promoting the occurrence of ischemia.
The data available in the literature suggest that GnRH agonists may trigger PA in patients with pituitary adenoma. Because of the relative frequency of pituitary lesions in the general population and the widespread use of these drugs in highly prevalent diseases such as prostate or breast cancer, and the fact that pre-treatment pituitary hormone tests or X-ray evaluation are probably not cost-effective,9 a greater understanding of this relationship by physicians who prescribe these drugs is essential. Similarly, patients should be adequately instructed to promptly seek medical care if suspicious symptoms occur.
Although this is a rare adverse effect, the severity of the condition and the low sensitivity of CT of the head for detecting pituitary bleeding in the emergency room make it necessary to consider the possibility of PA in patients with pituitary adenoma who experience headache following the use of GnRH agonists even in the absence of visual deficiency, ophthalmoplegia, or impaired consciousness.
Please cite this article as: Guerrero-Pérez F, Marengo AP, Planas-Vilaseca A, Flores-Escobar V, Villabona-Artero C. Apoplejía hipofisaria inducida por triptorelina en paciente con cáncer de próstata. Endocrinol Nutr. 2015;62:411–412.