Psittacosis is a relatively uncommon cause of community-acquired pneumonia, often leading to diagnostic difficulty.
MethodsA retrospective study was conducted on the clinical features of psittacosis patients in China. Forty-six cases of Chlamydophila psittaci infection with atypical pneumonia of varying severity in the last two years were described retrospectively.
ResultsFever, relative bradycardia, and other systemic upsets were the main clinical presentation. The most common radiographic abnormality was segmental or lobar shadowing or consolidation. The total white cell counts were usually normal or slightly increased. The concentration of creatine kinase, C reactive protein, and lactic dehydrogenase increased, while albumin decreased remarkably. These cases exhibited good recovery after being treated with tetracycline or quinolone antibiotics.
ConclusionThese features may help differentiate psittacosis from other traditional bacterial pneumonia. However, they do not provide a definitive diagnosis. Psittacosis diagnosis must perform the whole-genome sequencing for Chlamydophila psittaci in respiratory, blood, or sputum specimens. Increased awareness of psittacosis can shorten diagnostic delays and improve patient outcomes.
La psitacosis es una causa relativamente poco común de neumonía adquirida en la comunidad, y a menudo conduce a dificultades diagnósticas.
MétodosSe realizó un estudio retrospectivo sobre las características clínicas de los pacientes con psitacosis en China, en el que se describen retrospectivamente 46 casos de infección por Chlamydia psittaci con neumonía atípica de gravedad variable en los últimos dos años.
ResultadosLa fiebre, la bradicardia relativa y otros trastornos sistémicos fueron la presentación clínica principal. La anomalía radiográfica más común fue el sombreado o consolidación segmentaria o lobular. Los recuentos totales de glóbulos blancos fueron generalmente normales o ligeramente aumentados. Las concentraciones de creatina quinasa, proteína C reactiva y deshidrogenasa láctica aumentaron, mientras que la albúmina disminuyó notablemente. Estos casos mostraron una buena recuperación después de ser tratados con antibióticos de tetraciclina o quinolona.
ConclusiónEstas características pueden ayudar a diferenciar la psitacosis de otras neumonías bacterianas tradicionales. Sin embargo, no proporcionan un diagnóstico definitivo. El diagnóstico de psitacosis debe realizar la secuenciación del genoma completo de Chlamydia psittaci en muestras respiratorias, sanguíneas o de esputo. Una mayor conciencia de la psitacosis puede acortar los retrasos en el diagnóstico y mejorar los resultados de los pacientes.
Psittacosis is a zoonosis resulting from Chlamydophila (C.) psittaci infection, with community-acquired pneumonia (CAP) being the most common clinical manifestation.1 The patients were infected with C. psittaci mainly through inhalation of infectious air droplets or dust particles from feces or respiratory tract secretions.2 Person-to-person transmission of Psittacosis is possible but rare.3
Psittacosis is a relatively rare cause of CAP. The disease ranges from subclinical infection to fatal pneumonia. According to a meta-analysis of 57 studies, Psittacosis accounts for 1% of incident cases of CAP,4 which is likely underdiagnosed and underreported due to the nonspecific presentation and the absence of this pathogen in most routine laboratory schemes. Therefore, it is critical for healthcare workers to distinguish it from bacterial pneumonia at an early stage. The research examined the clinical features of 46 cases of psittacosis pneumonia, which could help clinicians identify it and then treat it with a unique diagnostic process and medicine.
Materials and methodsStudy population and data collectionWe pooled psittacosis cases with pneumonia from 11 eastern and central China hospitals in the last two years. In the absence of positive nucleic results for other organisms, all cases were confirmed by venous blood, sputum, or bronchoalveolar lavage fluid (BALF) metagenomic next-generation sequencing (mNGS). The demographics, exposure history of poultry or birds, clinical findings, and radiographs were retrospectively obtained from the patients’ medical records. The study was approved by the Ethics Committee at the Hangzhou First People's Hospital of Zhejiang University and complied with the principles of the Declaration of Helsinki.
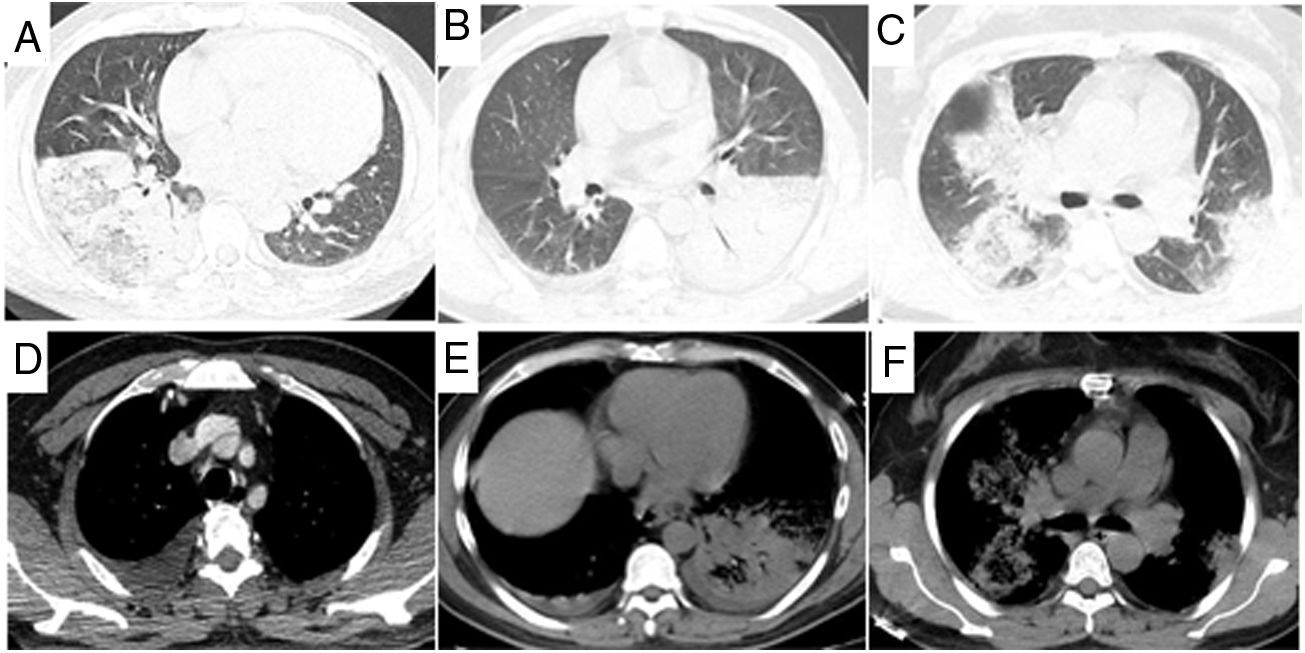
Data analysisThe chest CT was examined by a physician and a radiologist. The extent of radiographic consolidation was categorized as segmental, lobar, affecting more than one lung lobe, or affecting both lungs. The shadowing was described as patchy, confluent, and nodular. Pleural fluid, loss of lung volume, and hilar adenopathy were also recorded. A follow-up chest CT was performed to determine the resolution rate of radiographic changes.
Relative bradycardia was defined as an increase in pulse rate of <18bpm for every 1°C rise in body temperature, or body temperature>38.9°C with a pulse rate<120bpm.5 Categorical data were expressed as absolute values and in terms of the percentage of the population. Quantitative data were expressed in terms of mean±standard deviation and interquartile range (IQR).
ResultsPatients’ characteristicsThe study included 46 patients who were all hospitalized and tested positive for C. psittaci by mNGS. In our cases, 3–5mL of BALF were sampled for mNGS in 39 cases, 4mL of venous blood in 8 cases, and 1mL of sputum in 2 cases. All cases in our series were sampled on days 1–7 after admission. Our case series included 28 male patients and 18 female patients. Their mean age during diagnosis was 57.1±10.5 years (IQR, 50–65 years). Of these patients, five had diabetes, three had malignance, 28 (60.9%) had a definite history of poultry contact, and only one was exposed to parrot. A total of 34/46 (73.9%) cases occurred between September and March.
Clinical findingsAll cases were febrile with a mean temperature of 39.7±0.6°C (IQR 39.2–40.1°C) in the course, of which 5 cases had a normal temperature on admission, and 41 (89.1%) had the highest temperature up to more than 39°C. Cough was usually mild in 26 (56.5%) cases. It produced sputum in 11 (23.9%) cases, but no organisms were cultured. Sputum was bloody and purulent in two of the cases.
Some systemic upsets were widespread in our cases. Febrile symptoms were reported in 41 patients, with 9 (19.6%) cases experiencing breathlessness and 10 (21.7%) experiencing headaches. Less frequent symptoms were vomiting in six, diarrhea in one, and malaise in four cases. Before presentation at the hospital, the mean duration of symptoms was 6.6±3.2 days (IQR 4–8 days). Relative bradycardia was found in 33 (71.7%) cases. In most cases, localized inspiratory crackles were found, but other physical signs were uncommon.
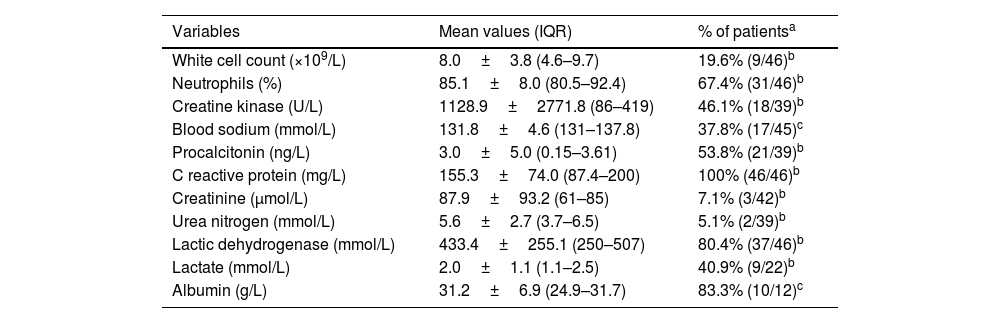
The prominent blood laboratory abnormalities are displayed in Table 1. The results of other routine blood chemicals and enzyme tests were normal.
Hematological laboratory values on admission.
| Variables | Mean values (IQR) | % of patientsa |
|---|---|---|
| White cell count (×109/L) | 8.0±3.8 (4.6–9.7) | 19.6% (9/46)b |
| Neutrophils (%) | 85.1±8.0 (80.5–92.4) | 67.4% (31/46)b |
| Creatine kinase (U/L) | 1128.9±2771.8 (86–419) | 46.1% (18/39)b |
| Blood sodium (mmol/L) | 131.8±4.6 (131–137.8) | 37.8% (17/45)c |
| Procalcitonin (ng/L) | 3.0±5.0 (0.15–3.61) | 53.8% (21/39)b |
| C reactive protein (mg/L) | 155.3±74.0 (87.4–200) | 100% (46/46)b |
| Creatinine (μmol/L) | 87.9±93.2 (61–85) | 7.1% (3/42)b |
| Urea nitrogen (mmol/L) | 5.6±2.7 (3.7–6.5) | 5.1% (2/39)b |
| Lactic dehydrogenase (mmol/L) | 433.4±255.1 (250–507) | 80.4% (37/46)b |
| Lactate (mmol/L) | 2.0±1.1 (1.1–2.5) | 40.9% (9/22)b |
| Albumin (g/L) | 31.2±6.9 (24.9–31.7) | 83.3% (10/12)c |
The chest CT (Fig. 1) showed patchy infiltration in 25 (54.3%) cases, lobar consolidation in 30 (65.2%) cases, and reserved halo in 1 case. Cavitation was not observed in our patients. Both lungs were affected in 14 (30.4%) cases. Lung lesions were found in the right upper lobe in 8 cases, the right middle lobe in 3, the right lower in 8, the left upper lobe in 5, and the left lower lobe in 8 cases. Mediastinal lymphadenopathy was observed in two cases. Pleural effusion occurred in 11 (23.9%) cases, and it was bilateral and independent of the pulmonary lesions in three cases.
Treatment and outcomesMoxifloxacin or levofloxacin was prescribed as the single antibiotic in 23 cases, quinolones combined with doxycycline in 12 cases, and doxycycline only in 5 cases. β-lactams or carbapenem antibiotics were changed to quinolones after identifying psittacosis in six cases.
The mean duration of fever was two days after the antibiotics above were prescribed. The body temperature was recovered, and most symptoms were reduced. Notably, not all patients had a fever before or on admission, but all had a fever later. A respiratory failure occurred in 34.8% (16/46) cases, in which non-invasive ventilation was applied in 26.1% (12/46) cases and invasive mechanical ventilation in 8.7% (4/46) cases. Four cases were exacerbated by shock, and one died from respiratory failure. The abnormal chest radiograph had improved significantly before the patients were discharged. The mean duration of hospitalization was 11.9 days. The chest CT abnormalities in the survivors resolved before they were discharged.
DiscussionIn this study, 46 cases of psittacosis infection were identified and collected from 11 hospitals. Our cases concluded that the clinical features of psittacosis include CAP with hyperpyrexia, relative bradycardia, varied extrapulmonary manifestations occurring before or after fever, and rapidly developing with a high rate of severe cases.
Human psittacosis is a zoonotic infectious disease predominantly transmitted through inhalation of the obligate intracellular bacterium C. psittaci from an infected or asymptomatic animal.1 Individuals exposed to birds, such as pet bird owners or workers, poultry processing workers, are at a higher risk of contracting psittacosis. Psittacosis has an incubation period of 5 to 28 days in humans after infection. It occurs prominently in winter and spring, which may be attributed to the vulnerability of C. psittaci in hot seasons.
In addition to the traditionally psittacine birds, many studies suggested that other animal species were also regarded as possible sources of human psittacosis.2 The present cases showed that poultry was a more prominent source than the parrot-like birds. With this in mind, clinicians and public health investigators should pay more attention to poultry than parrots or other bird species in medical history and source tracing. Notably, there was no definite contact history of animals in 40% of cases, which led to a difficulty in early diagnosis. It is necessary to perform a rapid pathogenic detection for pneumonia of unknown causes.
In our cases, the most frequently encountered symptoms of psittacosis included fever, nonproductive cough, myalgia, chill, and respiratory distress that were often described as flu-like. In some severe cases, C.psittaci causes headache, vomiting, and diarrhea, but not encephalitis or myocarditis. Similar to previous studies, there was no gender difference in this series of psittacosis infections. However, all of our cases were over 40, differing from the earlier finding that the disease occurred in all age groups.6
In contrast to some earlier studies, chest pain was uncommon in our cases.6 Consistent with previous studies, relative bradycardia was one of the high incidence signs in our cases.7 Crackles were heard in most cases, but other signs were rare. Unlike the previous study showing a normal chest radiograph in 28% of cases,6 all of our patients showed varied lobar infiltration or consolidation in chest CT, which was the most frequent abnormality in the unilateral lung. There was an association of the dimension of consolidation with the severity of psittacosis. None of radiographic features allowed discrimination between psittacosis pneumonia and other acute cases of pneumonia.
The most frequent laboratory features were hypoxemia, normal count of WBC, slightly rising neutrophils percentage and PCT, increased C-reactive protein, CK and LDH, and lower blood albumin. The white cell count within the normal range may help to exclude other traditional bacterial causes of pneumonia.
Generally, psittacosis pneumonia is suspected when the pneumonia of unknown causes occurs between September and March. These features include relative bradycardia, fever, myalgia, acute respiratory distress, an average count of WBC, and increased CK or LDH, especially with a history of avian contact. The empirical treatment could be taken as soon as possible based on the diagnostic suspicion.
Notably, this disease does not present any clinical manifestation or alteration of routine diagnostic tests that could be considered diagnostic. In most hospitals, C. psittaci is excluded in the routine bacterial or viral detection workup.
Psittacosis can be diagnosed by isolating C. psittaci, serology, or molecular detection. Isolation of C. psittaci requires cell culture. The serological tests include complement fixation test, enzyme-linked immunosorbent assay, and microimmunofluorescence test, which require serum samples collected two weeks apart. The serological tests could be helpful in retrospective studies. Nucleic-acid amplification techniques such as PCR and mNGS provide sensitive and species-specific detection of C. psittaci.8 According to a systematic review, PCR aids in rapidly identifying psittacosis patients in outbreak situations, but its sensitivity is only high in the acute phase.9 However, the samples one week after admission remained positive for mNGS in our cases. Several previous studies indicated that mNGS was a reliable tool that rapidly and accurately identified the C. psittaci.10–12 All our cases got detected with C. psittaci using mNGS from venous blood, sputum, and BALF specimens. The mNGS takes 2–3 days to complete the detection and provides an accurate diagnosis of psittacosis. It is optimal to perform mNGS for severe pneumonia of unknown causes, especially in times of COVID when we tend to forget that there are other aetiologies.13
Tetracyclines, in particular doxycycline, are considered the drug of choice to treat chlamydiosis. Macrolides and quinolones can also be used as alternative therapies. A significant improvement was observed on day 3 of effective treatment in our patients. The diagnosis should be considered when there is a poor response to penicillin or other antibiotics to which chlamydia is insensitive.
Finally, we also realized that these clinic features observed in our cases could have limits due to the limited sample size. A clinic study on a larger scale should be conducted in the future.
ConclusionsPsittacosis diagnosis is often delayed due to a lack of special symptoms and regular laboratory detection. A history of avian exposure gives a valuable diagnostic clue in patients with atypical pneumonia. Early diagnosis with mNGS or PCR testing and timely initiation of appropriate antibiotics can reduce patient morbidity and mortality.
Ethics approval and consent to participateThe study was approved by the Ethics Committee at the Hangzhou First People's Hospital, Zhejiang University, and complied with the Declaration of Helsinki.
FundingThis work was supported by Zhejiang Province Nature Science Funding Commission Social Development Project [grant no. LGF20H010005].
Conflict of interestsThe authors declared that there is no conflict of interest regarding the publication of this article.
Not applicable.