Antibiotic use and misuse are linked to pathogen resistance and, as such, both constitute a public health issue with local, national, and global dimensions. Early studies have shown striking variations in the use of these drugs between Nordic and Mediterranean countries. The aim of the present study was to describe and compare antibiotic prescribing in Primary Care in Denmark and Aragón (a North-eastern Spanish region).
MethodsOutpatient antibiotic prescription data (2010) were obtained from the National Institute for Health Data and Disease Control (Denmark), and the Information System on Medication Consumption in Aragón. The consumption of antibiotics (ATC J01) was analyzed from the prescription rates and the number of defined daily dose (DDD) per 1000 inhabitants/day (DID).
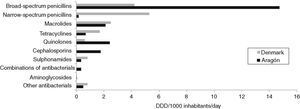
ResultsThe rate of antibiotic prescription in 2010 in Aragón was greater than in Denmark (407 compared to 315 exposed individuals/1000 inhabitants). There were significant differences as regards overall consumption of antibiotics (23.2 DID in Aragón and 17.0 DID in Denmark), as well as the therapeutic group selection. There was an elevated use of broad spectrum penicillins, quinolones and cephalosporins in the Spanish region while, in Denmark, the most-consumed antibiotic was narrow spectrum penicillin.
ConclusionThe use of antibiotics in the Spanish region is very high, and there are marked differences in the choice of drug between this region and Denmark. Interventions are needed that promote the rational use of these drugs to reduce potential bacterial resistance, and to avoid unnecessary risks to patients.
El uso inadecuado de antibióticos se ha relacionado con la aparición de resistencias microbianas, constituyendo así un problema de salud pública de dimensiones locales, nacionales y globales. Estudios previos han mostrado importantes diferencias en el uso de estos fármacos entre los países nórdicos y los mediterráneos. El objetivo de este estudio fue describir y comparar la prescripción antibiótica en atención primaria en Dinamarca y Aragón.
MétodosLos datos de utilización extrahospitalaria de antibióticos (2010) se obtuvieron del National Institute for Health Data and Disease Control (Dinamarca) y del Sistema de Información de Consumo Farmacéutico de Aragón. El consumo de antibióticos (ATC J01) se analizó mediante las tasas de prescripción y el número de dosis diaria definida por 1.000 habitantes/día (DHD).
ResultadosLa tasa de prescripción antibiótica en 2010 en Aragón fue superior a la de Dinamarca (407 frente a 315 expuestos/1.000 habitantes). Se observaron diferencias significativas en cuanto al consumo total de antibióticos (23,2 DHD en Aragón y 17 DHD en Dinamarca), así como en la elección del grupo terapéutico. La utilización de penicilinas de amplio espectro, quinolonas y cefalosporinas en la región española fue elevada, mientras que en Dinamarca el antibiótico más consumido fue una penicilina de espectro reducido.
ConclusiónEl uso de antibióticos en Aragón es elevado, y existen importantes diferencias en la elección del tipo de fármaco entre esta región y Dinamarca. Sería conveniente desarrollar intervenciones que promuevan el uso racional de estos fármacos, para reducir las resistencias bacterianas y evitar riesgos innecesarios a los pacientes.
Antimicrobial resistance threatens the effectiveness of successful treatment of infections. It is becoming a public health issue with local, national, and global dimensions. The outcomes are the increased morbidity, disease burden, and mortality.1 Several studies have shown the relationship between antimicrobial drug use and the level of pathogen resistance at a national level in countries within the European Union. Antibiotic overuse and misuse have been recognised as important factors determining the development of antimicrobial resistance.2
Early studies showed striking geographical variations in the use of antibiotics between the Nordic and the southern European countries. Denmark had a low consumption, and the prescribing profile followed national guidelines. Conversely, Spain was one of the countries where antibiotics were most often used.2,3 However, and according to recent data, changes have been occurring. Antimicrobial drug consumption in the Danish Primary Health Care has increased notably during the latest decade.3,4 In Spain, not only at the national level but also regional, there have been several campaigns and interventions conducted in favour of a more rational, and prudent, use of antibiotics.5 These messages directed at physicians, drug companies, and patients may have had positive influence on the observed decrease in antibiotic use.5
Awareness of outpatient antibiotic use and their regional differences are important tools for action and investigation, and should be a stimulus to improve the quality of prescription and, hopefully as a result, to reduce resistance levels.3
The aim of the present study was to describe and compare antibiotic prescribing in Primary Care in Denmark and Aragón (an Autonomous Region in north-eastern Spain).
MethodsThe data on consumption of antibiotics in Primary Care in the year 2010 were obtained from the National Institute for Health Data and Disease Control in Denmark6 and the Information System for Medication Consumption in the Aragón Community. The Danish database is a public, open-access web that contains the following information: identification of the dispensed product according to the Anatomical Therapeutic Chemical (ATC) classification code defined by the World Health Organization (WHO), volume sold, volume sold per 1000 inhabitants, number of users per 1000 inhabitants; each one of these categories segregated by age and gender. The Aragón database contains: patient code to ensure anonymity, ATC code of the dispensed product, number of packages and defined daily dose (DDD) dispensed, prescription month, gender and date of birth of the patient. Permission to access this source of information was obtained from the Aragón Health Sciences Institute.
In Denmark there were 5,534,738 inhabitants on the 1st of January 2010.7 It is mandatory to report the sale of these medicines and, therefore, the obtained data cover all sales to patients. Self-medication with antibiotics is rare in Denmark, and 97% of prescribed antibiotics were obtained after a clinical consultation.6 The population studied in Aragón were all those inhabitants of the Autonomous Region with cover under the National Health Service (NHS) of Aragón which, in 2010, were 1,327,827. All the antibiotic prescriptions dispensed in the pharmacies under the Aragon NHS were included. Not taken into account were private prescriptions and those covered by private insurances, hospital-based consumption, and drugs purchased without prescription.
To compare antibiotic consumption (ATC code J01) we used the antibiotic prescription rates (number of individuals receiving at least one prescription in one year per 1000 inhabitants), unadjusted as well as adjusted for age by the direct method using the standard European population, with a confidence level of 95%. Data were broken down by gender and different age groups. In Aragón, 19.8% of the registered prescriptions in the database corresponded to non-identified patients whose patient code, gender, date of birth were not available. To preclude underestimation of the real rate of consumption and to facilitate comparisons of both populations in the two study areas, the number of patients that would correspond to these prescriptions was estimated based on the data of those for whom this information was available.
Also, the technical unit suggested by the WHO was used i.e. the defined daily dose (DDD), which enables the population exposure to drug use to be calculated as number of DDD per 1000 inhabitants per day (DID), according to the ATC/DDD method.8 For the DID calculation, the DDD for each of the following groups was collated: tetracyclines (J01A), narrow spectrum penicillins (J01CE), broad spectrum penicillins (J01CA and J01CR), cephalosporins (J01D), sulphonamides and trimethoprim (J01E), macrolides (J01F), aminoglycosides (J01G), quinolones (J01M), combinations of antimicrobials (J01R) and other antimicrobials (J01X). To establish the consumption of DID by gender and by age, we calculated the new values of DID for each case in Aragón according to the same methodology as for the rates of prescription, which enables comparisons to be made with the data obtained from Denmark.
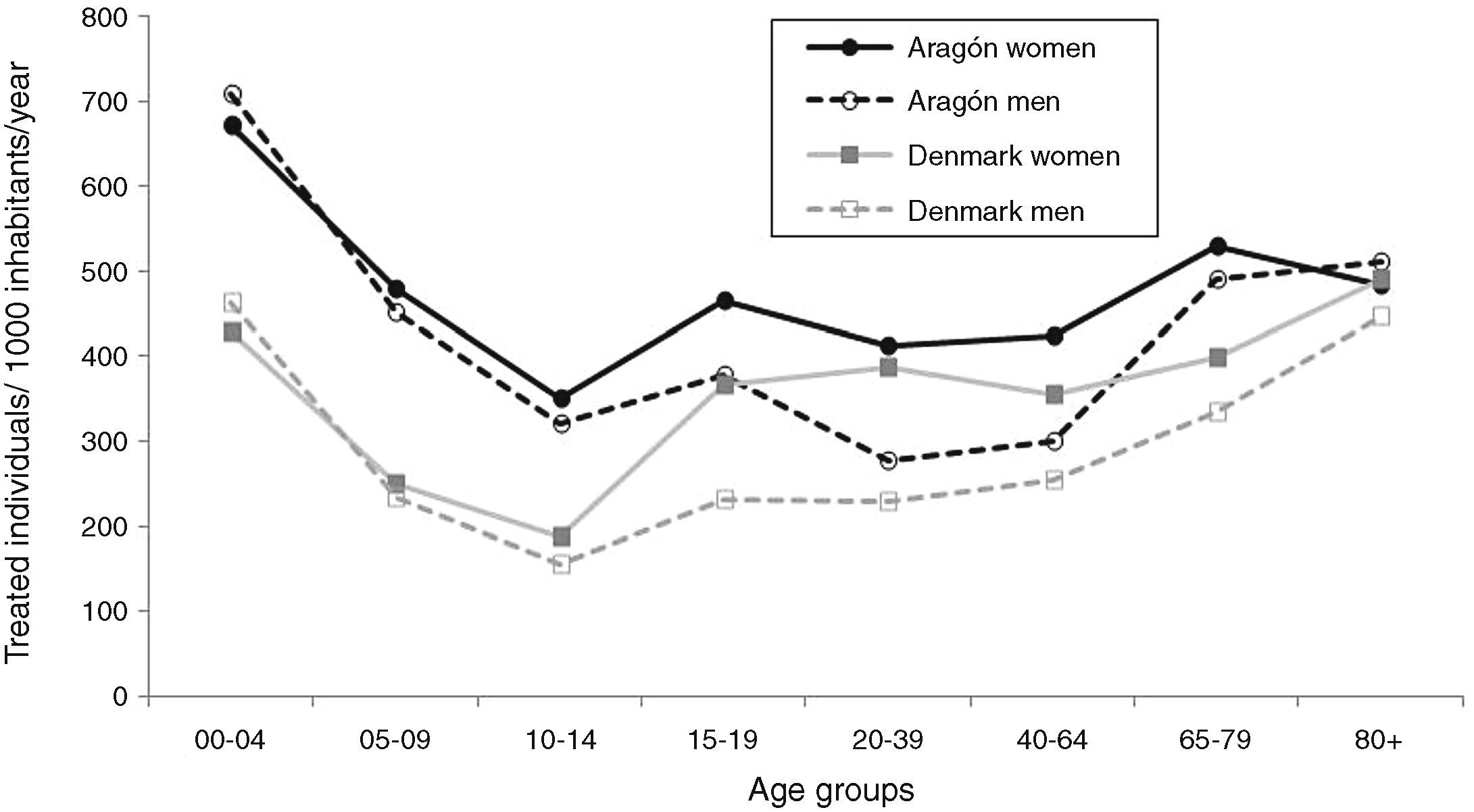
ResultsThe antibiotic prescription rate in Denmark in 2010 was 315 per 1000 inhabitants per year (95% CI: 311–320) compared to that in Aragón, 407 per 1000 inhabitants per year (95% CI: 396–418). When adjusted for age, these rates were 311 in Denmark and 409 per 1000 inhabitants per year in Aragón. The prescription rate was higher in Aragón for all ages, except for those above 80 years of age where the prescription rate was higher in Denmark. The differences between the two study regions were statistically significant for the 0–19 and 55–79 year age groups. Also, in the two populations studied there were differences between the rate of prescriptions in women and in men (364 women versus 266 men in Denmark and 453 women versus 360 men/1000 inhabitants in Aragón). Females received more treatment at all ages except 0–4 years, in both study regions (Fig. 1). The general trend observed in prescription rates segregated by gender and age was similar in both populations.
There were important differences between the two study regions in relation to the overall consumption of antibiotics; 23.2 DID in Aragón and 17.0 DID in Denmark. The volume of antibiotics used by the females was greater than that by the males; 19.3 versus 13.4 DID, respectively in Denmark and 24.9 versus 21.4 DID, respectively in Aragón.
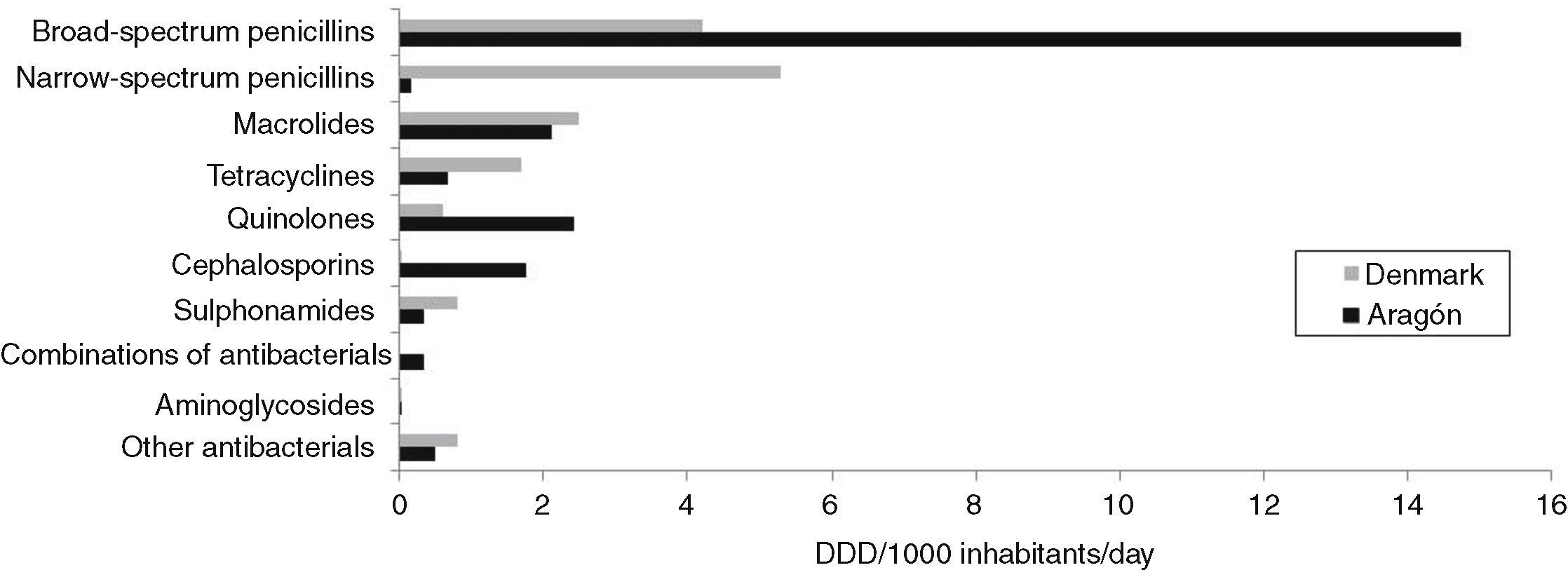
The election of therapeutic drug subgroups showed differences between the study regions (Fig. 2). Penicillins were the most prescribed antibiotics not only in Aragón but also in Denmark. A very high consumption of broad spectrum penicillins was registered in the Spanish region while, in Denmark, the most prescribed were the narrow spectrum penicillins. Also in Aragón there was a wide use of quinolones, macrolides and cephalosporins. In Denmark other groups being prescribed frequently were macrolides and tetracyclines. The consumption of aminoglucosides was insignificant in the two study regions. Of note in Aragón was the combination of antibiotics (principally spiramycin with metronidazol) and antibiotics of the J01X group that were, essentially, fosfomycin and nitrofurantoin. In Denmark, this group included antibiotics such as nitrofurantoin and methenamine.
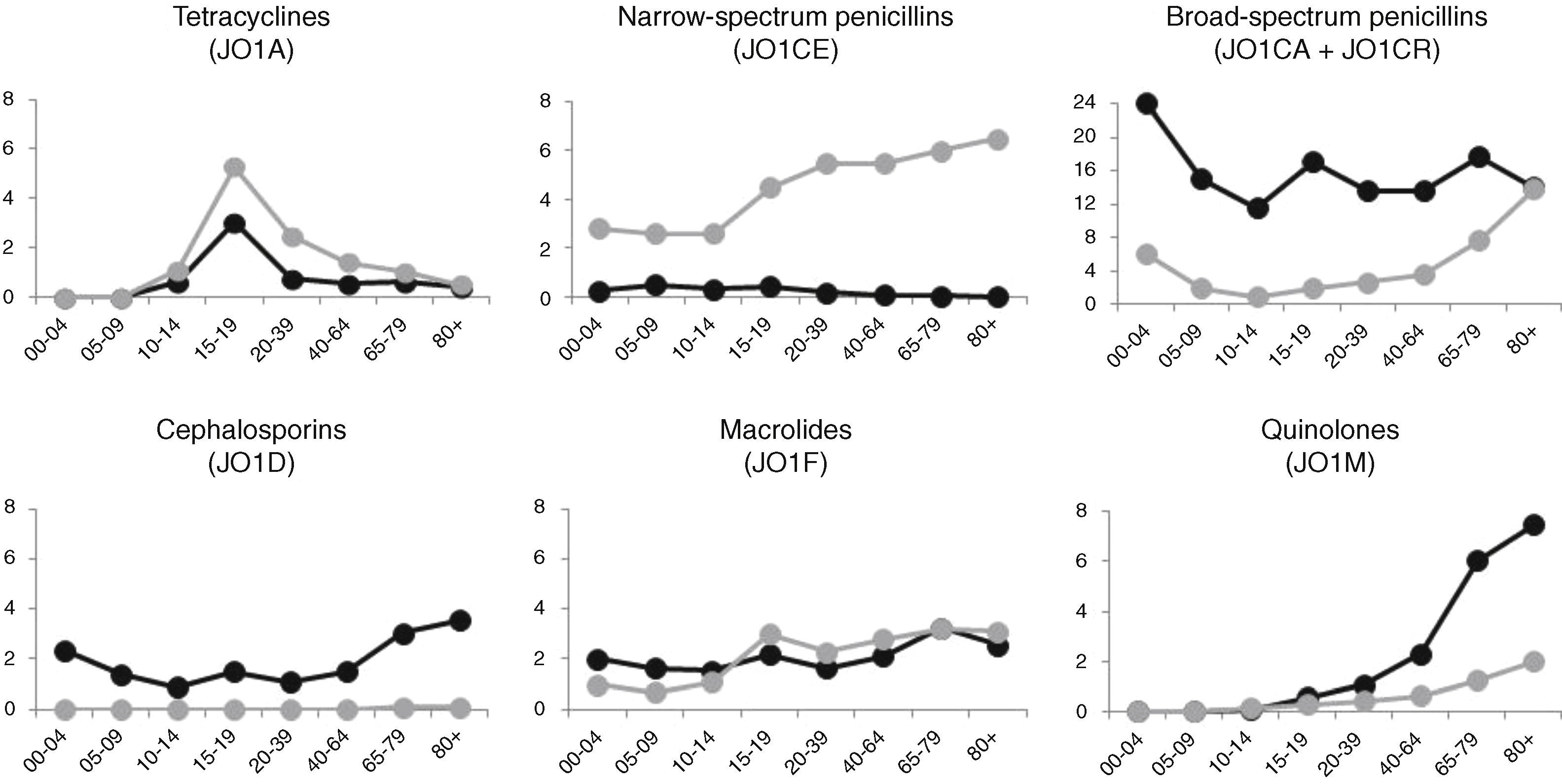
As shown in Fig. 3, consumption of broad spectrum penicillins was very high in Aragón in all age groups. Of note is that in children (0–4 years) the use was 23.9 DID. In Denmark the consumption of this therapeutic type was moderately high at 0–4 years (6.0 DID) and, as well, beyond the age of 65 years. Narrow spectrum penicillins, the prescription of which was non-significant in Aragón, had an increasing and notable use in Denmark beyond 15 years of age. Tetracyclines were highly prescribed in the 15–19 year old age group, especially among the Danes. In Aragón, the use of quinolones in the older age groups and cephalosporins in children and older age groups was of considerable note. The latter were not prescribed in Denmark. The use of macrolides showed a very similar pattern in both study areas, and in most age groups.
DiscussionThe present study provides relevant data on the use of antibiotics in Denmark and Aragón (Spain). In the past decade, Vaccheri et al.9 compared the prescription of antibiotics in Ravenna (Italy) with that in Funen (Denmark). The rate of prescription in the Italian region was higher than in the Danish region (400 inhabitants exposed versus 300/1000 inhabitants, respectively). Our results reflect a prescription rate in Aragón (407 exposed/1000 inhabitants) that is similar to the Italian population and, as such, represents an overall proportion of individuals exposed to antibiotics that is much higher than in Denmark (315 exposed/1000 inhabitants). In general, women were more exposed than males in both study areas. There are few studies that contain information on differences in the prescriptions of these drugs as a function of gender. Gulliford et al.10 observed that the prescriptions of antibiotics were about 30–50% higher in women than in men in the treatment of respiratory tract infections (RTIs). This was explained by the higher rate of consultations by the women. Other authors considered that the greater prescription of antibiotics in women was attributable, possibly, to their higher rate of urinary tract infections requiring treatment.11 The consumption (in terms of DID) obtained for both study regions was, as well, higher in women. Conversely, the prescription rate in children was much higher in Aragón than in Denmark. Two previous studies showed that antibiotic use in Danish children was substantially lower than that observed in children from a Canadian population12 and that of another population in Italy.13
The differences in our two study populations were important for the assessment of the consumption of antibiotics, as measured by DID. The value we obtained for the Danes was somewhat similar to that declared for the country in 2010 in the annual report of the European Surveillance of Antimicrobial Consumption Network (ESAC-Net) published by ECDC (17.0 DID versus 16.5 DID).3 On the other hand, the level observed in Aragón (23.2 DID) was higher than that presented by the EDCD for Spain for the year 2010 (20.3 DID).3 The Community of Aragón has been shown, already, to have a higher use of antibiotics compared to the mean of the rest of Spain.14 This could be due to factors related to a higher consumption of antibiotics such as by a higher older-aged population in Aragón15 or of a rural population that is proportionally greater than the rest of Spain.16
There are large variations in DID between countries. The consumption of antibiotics in Europe in 2010 varied between very high values (e.g. France; 28.2 DID) and others lower (e.g. Netherlands; 11.2 DID).3 Analysis of antibiotic use, as measured by DID, is considered a relevant indicator of public health quality since it is, probably, the best marker of the pressures leading to bacterial resistance.2 Although the number of DID used in Denmark has increased,4 it continues to be among the lowest in Europe, and with a lower proportion of antibiotic-resistant pathogens. On the other hand, Spain is positioned as a country with a higher rate of resistance to antibiotics.1 However, several of the comparative studies conducted to-date do not highlight Spain as being one of the regions with higher use. This is due, probably, to an underestimation of consumption. For example, the NHS in Spain estimated the total consumption of antibiotics in 2005 as 18.8 DID, a very low level compared with that obtained by Campos et al.17 who took into account the total sales of antibiotics (including private-health prescriptions as well as antibiotics purchased without a medical prescription). The DID, in this case, was equal to 28.93, which placed Spain among the countries with highest consumption in Europe.17
There are other important differences in the choice of antibiotics between the two populations. Penicillins were the drugs most utilized in both areas, representing >60% of the total DID prescribed. However, while in Denmark 6 of every 10 prescriptions of penicillins correspond to narrow spectrum type, in Aragón almost all the prescriptions of penicillins were the broad spectrum type. The high prescription rate of broad spectrum penicillins in the Danish population >60 years of age is explained, in part, by the treatment with pivmecillinam of urinary tract infections in women. The use of tetracyclines, higher in Denmark, peaks in the 15–19 year age group which is reasonable since this is the antibiotic used in this age group to treat juvenile acne. On the other hand, the quinolones are observed among the most prescribed antibiotics in the adult Aragón population, while its use is sporadic in Denmark. Quinolones are among the antibiotics the WHO defines as Critically Important Antimicrobials (CIA) in medicine,18 the use of which should be rational and reserved for the treatment of serious infections in humans. According to Spanish therapeutic recommendations, quinolones are recommended as second-line treatment in several specific infections, such as pneumonia or acute exacerbation of Chronic Obstructive Pulmonary Disease (COPD).19 Nevertheless, the high number of DDD obtained could exhibit a low adherence to recommendations. The use of cephalosporins represented around 8% of the total DID in Aragón, and was almost completely absent in Denmark. Oral cephalosporins are not funded by the Danish NHS, but they are funded by the NHS in Spain. However, these drugs are considered first-line neither in the treatment of RTIs, nor in the majority of infections at other sites19 and, as such, its high use in Spain is not justified. The use of spiramycin with methronidazol, a combination that is used almost exclusively in odontology, was notable in Aragón while not being used in Denmark.
Earlier studies9,20 had shown that there was a marked difference in the geographic pattern of north-south Europe in the outpatient consumption of antibiotics. It is difficult to explain the high variability, but some characteristics of both populations should be considered when trying to explicate the disparities observed.
Our two study populations did not have important demographic differences, albeit the Aragón population showed an ageing that was slightly greater than the Danish population (the >80 age group was around 4% in Denmark compared to around 7% in Aragón).7,15 This does not appear to justify the differences observed, since these differences are maintained when the rates are adjusted for age.
The type of health care organisation in both regions plays also an important role in the prescribing habits. Danish Primary Health Care resembles the Spanish one in some aspects. Both of them are mostly financed by public funds, being the regions governments who manage the health care. The two are based on a patient list system, i.e. citizens are assigned to a GP, who is responsible for serving the patients on his/her list. This system enables the GP to develop a better knowledge of the individual patient.21,22
On the other hand, some differences between the ambulatory systems can be described. Spanish GPs work within a team of GPs, receiving a fixed salary regardless of the number of patients attended. Nevertheless, Danish GPs run private practices (self-employed), either on their own as solo practitioners or in collaboration with a few GPs more. Two thirds of their incomes are fees for services rendered.21 This latter situation may sometimes cause that Danish GPs prescribe according to the patient's wishes, to ensure upcoming consultations.
The number of inhabitants per GP in Denmark is not very distinct from that in Spain. However, in Spain there is in addition one paediatrician per 1029 inhabitants.21,22 Spanish children are normally treated by paediatricians, whereas in Denmark all patients, including children, are treated by the GP. Some authors noted that paediatricians may be more liberal prescribers than GPs, and were more likely to prescribe antibiotics inappropriately.23
Furthermore, the number of pharmacies per inhabitant is about ten times higher in Spain than in Denmark.21,22 It should not be a negligible difference, if we take into account the obtained results.
Some variables associated with an inappropriate prescription of antibiotics can be the fear of possible complications for the patients, and the desire on the part of the physician to satisfy the expectations of the patient (or their parents/guardians, in the case of children).24 Until a few years ago, obtaining an antibiotic in a Spanish pharmacy without a medical prescription was not an unusual practice. As a consequence, Spanish patients could have greater expectations to receive an antibiotic when they attend the medical consultation by reason of an infection.
The frequency of patients’ attendance in the outpatient clinic and/or the high clinical work-load could also be factors related to the prescription increase.25 In Spain, citizens attend outpatient clinics more often than those residing in rest of Europe and the mean duration of the clinical visit in the Primary Care Centre is 5.4min.26 Contrarily, in Denmark, the mean duration of a consultation is 10–15min. Time constraint is a risk factor for antibiotic overprescribing. It takes longer time to explain a patient the reasons for not prescribing an antibiotic than it takes to make a prescription.
Llor et al.27 compared GPs prescription of antibiotics for RTIs in Denmark and Spain. These authors showed the different approaches to the choice of antibiotics for RTIs existing in both countries. Danish GPs used primarily narrow spectrum penicillin for most of the RTIs, while Spanish GPs preferred broad spectrum penicillins either alone or in combination with clavulanic acid. Current Spanish guidelines recommend the use of broad spectrum antibiotics as first-line treatment in some urinary tract infections, exacerbation of COPD or pneumonia in the elderly.19 National guidelines are developed considering the different resistance patterns existing in each country. Given that bacterial resistance to the most used antimicrobials is clearly distinct in the two study areas,1 the recommendations for some of the most frequent infections are different.
The utilization of different diagnostic methods in general practice may influence on the prescription of antibiotics as well.27 Most Danish GPs use a rapid antigen test (strep A) or a C-reactive protein (CRP) as a support to verify the diagnoses of bacterial tonsillitis or lower respiratory infection. These tests have been shown to reduce the number of patients treated with antibiotics.28,29 In Spain, none of these tests are used routinely in general practice. It could explain, at least partially, the higher antibiotic prescription rates obtained in the Spanish region.
Some previous studies20,27 highlighted that there is a low probability that the differences existing between the prescription habits of the Danish and Spanish physicians could be due to the unequal prevalence of RTIs receiving attention in Primary Care. Also the pressure exerted by the pharmaceutical industry to the GPs plays an important part in the choice of the antibiotic.27 In Denmark, there are strict rules to avoid doctors’ potential influence of economic incentives from pharmaceutical companies.21 The situation is more liberal in Spain, where drug companies are one of the main sources of information for physicians.30
As previously mentioned, all these factors affecting the use of antibiotics in the two study populations such as different social and cultural traditions, marketing policies of pharmaceutical companies, organisation of the NHS, or the national recommendations should be taken into account when comparing antibiotic use.
One of the principal limitations of our study is that the Danish database included all the outpatient prescriptions of antibiotics in the country while, in Aragón, only the outpatient consumption funded by the NHS was taken into account i.e. no account was taken of the consumption in the Spanish region associated with other administrative/funding entities such as private health prescriptions, or drugs acquired without prescription, or self-medication. As has been highlighted, these practices would have a significant impact on the overall consumption, and could represent up to 30% of actual utilization of antibiotics.17 Therefore, although the words “outpatient use”, “utilisation” and “consumption” have been used all through the paper, the analysis performed only included those antibiotics being prescribed in a medical prescription and funded by the NHS. As such, the data from our present study could be an underestimation of the real antibiotic utilisation, particularly in Aragón.
Another limitation is that the consumption databases do not contain information on the clinical indication for which the antibiotic was prescribed. As such, the appropriateness of the prescription could not be evaluated.
In conclusion, the present study is useful in increasing the knowledge of outpatient antibiotic use in the two populations studied. The data obtained suggest that, in general, women in both regions received a higher volume more frequently. In Aragón, the use of antibiotics in the population is very high, while the data in Denmark indicate a more moderate use. The different traditions, habits, pressures and recommendations existing in both countries should be considered when comparing these data. The obtained results should be a starting point in the search for possible explanations for these variations, and of solutions, or updates on recommendations and prescription guidelines. The misuse of antimicrobial drugs, or their abuse, favours the development and propagation of resistant bacteria, which implies a health threat for the population. Hence, we consider it necessary to conduct interventions at national as well as international level to promote a rational use of antibiotics.
FundingS. Malo was supported by a grant from the Programa Europa XXI, funded by the DGA (CONAID) and the Inmaculada Savings Bank [Grant number CM 8/12 to S.M].
The work received external funding from the Proyecto del Fondo de Investigación Sanitaria (Instituto de Salud Carlos III, Spanish Ministry of Science, Grant PI10/01048).
Conflict of interestThe authors have no conflict of interest to declare.