Passive transplacental immunity against respiratory syncytial virus (RSV) appears to mediate in the protection of the infant for the first 6 months of life. Lower environmental exposure in pregnant women to RSV epidemic may influence the susceptibility of these infants to infection by lowering the levels of antibodies that are transferred to the fetus.
ObjectivesTo contrast the risk of severe disease progression in infants with acute bronchiolitis by RSV, according to the mother's level of exposure to epidemic.
MethodRetrospective cohort study of previously healthy infants with RSV-acute bronchiolitis during 5 epidemics was made. We compared the severity of the infection in those born during the period of risk (when is less likely the mother's exposure to epidemic and the transfer of antibodies to the fetus: October 15th–December 15th in our latitude) with the rest of acute bronchiolitis. Bivariate analysis was performed regarding birth in period of risk and the rest of variables, using the Chi-square test. Multivariate logistic regression analysis was performed to study possible classical confounding factors.
Results695 infants were included in the study. 356 infants were born during the period of risk. Of the 56 patients requiring admission to PICU, 40 of them (71.4%) were born in this period (p=0.002). In the multivariate analysis, the birth in the period of risk showed a 6.5 OR (95% CI: 2.13–19.7) independently of the rest of variables.
ConclusionsThe worst clinical disease progression of the acute bronchiolitis by the RSV in less than 6 months age is related to lower exposure of the pregnant woman to the RSV epidemic.
La inmunidad pasiva transplacentaria contra el virus respiratorio sincitial (VRS) parece mediar en la protección del lactante durante los primeros 6 meses de vida. La menor exposición ambiental en embarazadas a la epidemia del VRS puede influir en la susceptibilidad de estos niños a la infección al disminuir los niveles de anticuerpos que se transfieren al feto.
ObjetivosContrastar el riesgo de progresión grave de la enfermedad en los lactantes con bronquiolitis aguda por VRS, de acuerdo con el nivel de exposición de la madre a la epidemia.
MétodoSe realizó un estudio de cohortes retrospectivo de recién nacidos previamente sanos con bronquiolitis aguda por VRS durante 5 epidemias. Comparamos la gravedad de la infección en los nacidos durante el período de riesgo (cuando es menos probable la exposición de la madre a la epidemia en nuestra latitud y la transferencia de anticuerpos al feto: del 15 de octubre al 15 de diciembre) con el resto de las bronquiolitis agudas. El análisis bivariante se realizó con respecto al nacimiento en el período de riesgo y el resto de las variables, utilizando la prueba de Chi-cuadrado. Posteriormente un análisis de regresión logística multivariable para estudiar los posibles factores de confusión.
ResultadosSeiscientos noventa y cinco bebés fueron incluidos en el estudio. Trescientos cincuenta y seis bebés nacieron durante el período de riesgo. De los 56 pacientes que requieren ingreso en la UCIP, 40 de ellos (71,4%) nacieron en este período (p=0,002). En el análisis multivariante, el nacimiento en el período de riesgo mostró una OR de 6,5 (IC 95%: 2,13-19,7) independientemente del resto de las variables.
ConclusionesLa evolución más grave de la enfermedad clínica de la bronquiolitis aguda por el VRS en menores de 6 meses de edad se relaciona con una menor exposición de la embarazada a la epidemia del VRS.
Despite the passage of time, no infectious illness has ever generated a greater health care burden than acute bronchiolitis in high-income countries. Respiratory syncytial virus (RSV) is the causative agent in approximately 65–80% of cases. It is a reason for hospital admission in itself, and up to 8–16% of admissions will end up in pediatric intensive care units (PICU).
The level of neutralizing antibody titers of the pregnant women against the RSV is different depending on the time of the year1,2 (the more epidemic season exposure, the greater titers) and will depend on many other factors,3 such as prior and current exposure to circulating epidemic viruses and the degree of exposure to the RSV depending on their cohabitants, especially children under 6 years of age. The degree of protection of the newborn and its antibody levels will differ according to the time of delivery with respect to the temporal evolution of the epidemic.4 At least in the first 6 months of life, the protection will depend on the transfer of neutralizing antibodies to the fetus.5 There are studies where it has become apparent the different risk of infection by the RSV, according to the month of birth,6–8 and it seems logical to think that this question may also have relation with the severity of the infection.
The objective of our study is to compare the risk of serious acute bronchiolitis in previously healthy infants under 6 months with acute bronchiolitis by RSV according to the time of birth regarding the beginning of the epidemic, on the assumption that lower environmental exposure to epidemic RSV of mothers during pregnancy can reduce the transmission of protective antibodies and, subsequently, increase the risk of severe infection in the child.
Patients and methodIt is a retrospective epidemiological study of the cohort of patients admitted with bronchiolitis by RSV to a pediatric reference hospital at meridional Europe in the period from April 1, 2010 to March 31, 2015. During these 5 epidemics, we consider those patients previously healthy, less than 6 months old with classical criteria of acute bronchiolitis9 and the presence of RSV antigen in nasopharyngeal aspirate10 (we tested systematically all infants at admission). There were excluded from the study babies with underlying pathology (congenital heart disease, bronchopulmonary dysplasia, immune deficiencies and neurological diseases) and preterm newborns below 32 weeks of gestation, because maternal antibodies pass largely between week 32 and 35 and in some cases, they could have received some dose of palivizumab.
In relation to the beginning of the epidemic, which usually occurs at the last weeks of October at our latitude in Europe, we established as infants at risk those born from the 15 October to 15 December, by low exposure to their mothers to the epidemic underway of RSV in the 6 months prior and therefore with less possibility of passive transfer of antibodies to the fetus. We contrasted the severity of the acute bronchiolitis of those born during the period of risk with the rest of the cohort. Severity was estimated according to the need of admission in PICU for mechanical ventilation (MV), considering any modality of invasive (conventional or high-frequency MV) or non-invasive support (positive pressure non-invasively, either CPAP or BiPAP), but not including the high-flow cannulas (HFC) mode. This variable was categorized as binary: present/absent.
In addition, to analyze possible confounding factors, we collected the variables of each patient at the moment of admission, sex, age, date of entry, weight at birth, gestational age, current age, birth by caesarean, gestational and postnatal tobacco exposure, any breastfeeding, atopic in any first-degree family (defined as asthma, atopic dermatitis, or proven allergy) fever, food intake less than 50% of usual, underweight in percentile less than 3, acute bronchiolitis severity score (ABSS),11 apnea episodes and serious bacterial superinfection, which was either suspected, based on clinical criteria previously described,12–14 either confirmed, by blood culture and/or urine cultures, whenever they occurred within 48h on admission. Nosocomial infections were excluded.
The qualitative variables were expressed in percentages. Quantitative variables were expressed as median and interquartile range. A bivariate analysis between need of PICU and independent variables using the Chi-square test was performed and also with respect to the variable birth in period of risk. The study for confounding factors was carried out as a multivariate logistic regression analysis with those variables that had reached at least a p<0.25 in the bivariate analysis. It was considered significant in multivariate analysis any p<0.05. The authors verified the autocorrelation between the independent variables in the multivariate analysis. The statistical analysis was made using SPSS 23.0 licensed software.
ResultsOf a total of 1006 infants admitted with acute bronchiolitis, it was detected RSV antigen in 774 nasopharyngeal aspirates (76.94%) and 719 cases were under 6 months of age. 45 cases were excluded because of previous underlying pathology and 34 were preterm infants less than 32 weeks gestation. In some patients, several exclusion criteria were overlapping. Finally, a total of 695 infants met the criteria for inclusion in our study.
56 admissions in PICU for MV during the stay were recorded, which means an incidence of 8.1% by season of healthy infants younger than 6 months (95% CI: 6–10%). 356 infants were born during the period of risk (51.5%). Of the 56 patients requiring admission to PICU, 40 of them were born in this period, while only 16 of them were born outside that period.
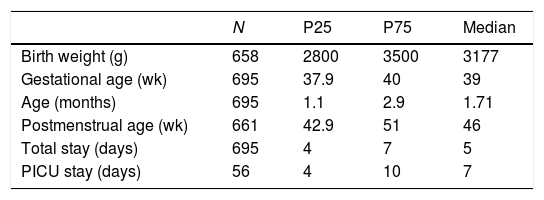
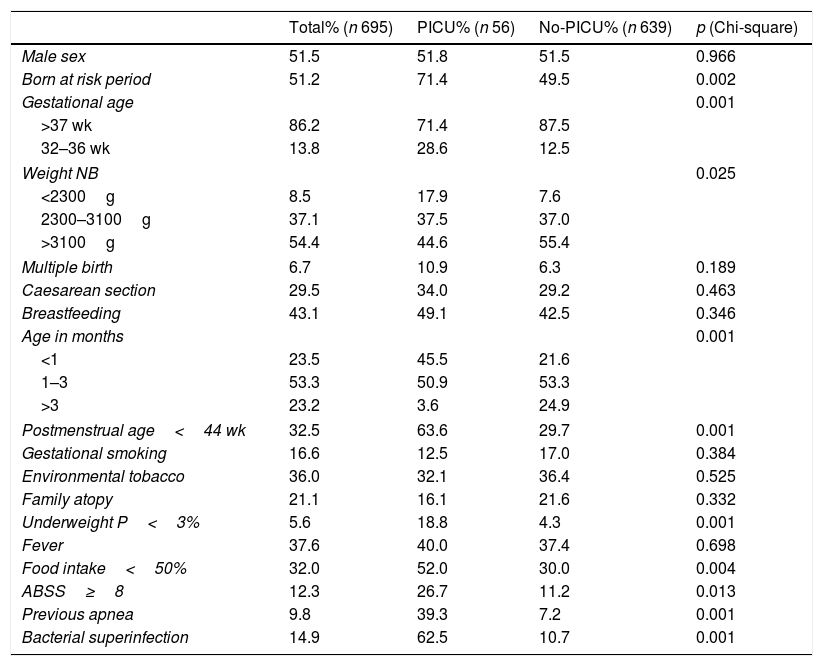
The quantitative variables of the sample are presented in Table 1. The independent variables are shown in Table 2, in global and distributed values according to the need of PICU admission. The bivariate analysis with Chi-squared test is also shown in Table 2. The variables that showed statistical significance were: birth at period of risk, birth weight, less than 50% hiporexia, the presence of apneas, low weight at admission, severity of acute bronchiolitis according to the scale of severity of acute bronchiolitis, bacterial superinfection, prematurity (32–37 weeks of gestation) and postmenstrual age (Table 2).
Characteristics of patients less than 6 months without underlying pathology admitted for acute RSV bronchiolitis.
| N | P25 | P75 | Median | |
|---|---|---|---|---|
| Birth weight (g) | 658 | 2800 | 3500 | 3177 |
| Gestational age (wk) | 695 | 37.9 | 40 | 39 |
| Age (months) | 695 | 1.1 | 2.9 | 1.71 |
| Postmenstrual age (wk) | 661 | 42.9 | 51 | 46 |
| Total stay (days) | 695 | 4 | 7 | 5 |
| PICU stay (days) | 56 | 4 | 10 | 7 |
Abbreviations: RSV: respiratory virus syncytial; g: grams; wk: weeks; P25: percentile 25; P75: percentile 75.
Frequency of qualitative variables in patients under 6 months without underlying pathology admitted for acute bronchiolitis by the RSV.
| Total% (n 695) | PICU% (n 56) | No-PICU% (n 639) | p (Chi-square) | |
|---|---|---|---|---|
| Male sex | 51.5 | 51.8 | 51.5 | 0.966 |
| Born at risk period | 51.2 | 71.4 | 49.5 | 0.002 |
| Gestational age | 0.001 | |||
| >37 wk | 86.2 | 71.4 | 87.5 | |
| 32–36 wk | 13.8 | 28.6 | 12.5 | |
| Weight NB | 0.025 | |||
| <2300g | 8.5 | 17.9 | 7.6 | |
| 2300–3100g | 37.1 | 37.5 | 37.0 | |
| >3100g | 54.4 | 44.6 | 55.4 | |
| Multiple birth | 6.7 | 10.9 | 6.3 | 0.189 |
| Caesarean section | 29.5 | 34.0 | 29.2 | 0.463 |
| Breastfeeding | 43.1 | 49.1 | 42.5 | 0.346 |
| Age in months | 0.001 | |||
| <1 | 23.5 | 45.5 | 21.6 | |
| 1–3 | 53.3 | 50.9 | 53.3 | |
| >3 | 23.2 | 3.6 | 24.9 | |
| Postmenstrual age<44 wk | 32.5 | 63.6 | 29.7 | 0.001 |
| Gestational smoking | 16.6 | 12.5 | 17.0 | 0.384 |
| Environmental tobacco | 36.0 | 32.1 | 36.4 | 0.525 |
| Family atopy | 21.1 | 16.1 | 21.6 | 0.332 |
| Underweight P<3% | 5.6 | 18.8 | 4.3 | 0.001 |
| Fever | 37.6 | 40.0 | 37.4 | 0.698 |
| Food intake<50% | 32.0 | 52.0 | 30.0 | 0.004 |
| ABSS≥8 | 12.3 | 26.7 | 11.2 | 0.013 |
| Previous apnea | 9.8 | 39.3 | 7.2 | 0.001 |
| Bacterial superinfection | 14.9 | 62.5 | 10.7 | 0.001 |
Abbreviations: RSV: respiratory virus syncytial; wk: weeks; NB: newborn; ABSS: acute bronchiolitis severity scale [11]; P: percentile.
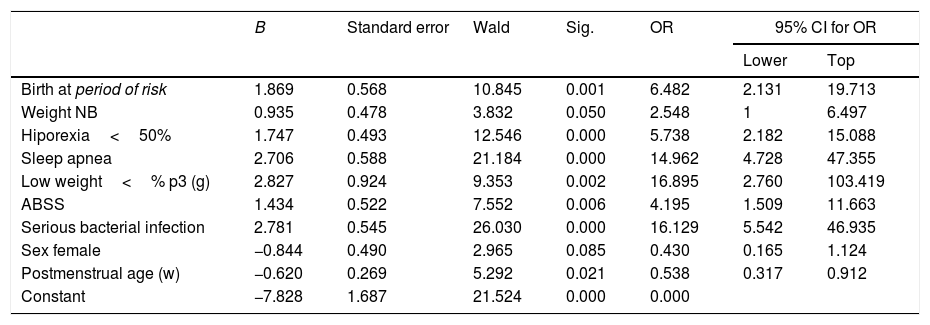
In the multivariate analysis, the birth in the period of risk showed a 6.5 OR (95% CI: 2.13–19.7) independently of the rest of variables included in the logistic regression model (Table 3).
Variables included in the calculation of logistic regression in infants with acute bronchiolitis in under 6 months previously healthy. NB: newborn. ABSS: acute bronchiolitis severity scale.
| B | Standard error | Wald | Sig. | OR | 95% CI for OR | ||
|---|---|---|---|---|---|---|---|
| Lower | Top | ||||||
| Birth at period of risk | 1.869 | 0.568 | 10.845 | 0.001 | 6.482 | 2.131 | 19.713 |
| Weight NB | 0.935 | 0.478 | 3.832 | 0.050 | 2.548 | 1 | 6.497 |
| Hiporexia<50% | 1.747 | 0.493 | 12.546 | 0.000 | 5.738 | 2.182 | 15.088 |
| Sleep apnea | 2.706 | 0.588 | 21.184 | 0.000 | 14.962 | 4.728 | 47.355 |
| Low weight<% p3 (g) | 2.827 | 0.924 | 9.353 | 0.002 | 16.895 | 2.760 | 103.419 |
| ABSS | 1.434 | 0.522 | 7.552 | 0.006 | 4.195 | 1.509 | 11.663 |
| Serious bacterial infection | 2.781 | 0.545 | 26.030 | 0.000 | 16.129 | 5.542 | 46.935 |
| Sex female | −0.844 | 0.490 | 2.965 | 0.085 | 0.430 | 0.165 | 1.124 |
| Postmenstrual age (w) | −0.620 | 0.269 | 5.292 | 0.021 | 0.538 | 0.317 | 0.912 |
| Constant | −7.828 | 1.687 | 21.524 | 0.000 | 0.000 | ||
B: estimated parameter of logistic regression; OR: odds ratio; Sig.: signification; CI: confidence interval.
Our research confirms the hypothesis that clinical presentation and severity of acute bronchiolitis caused by the RSV in infants less than 6 months of age could be associated to the epidemic RSV exposure pattern of the pregnant woman. Although we do not perform serology on pregnant women, our theory is based on assumptions about serology from other populations in European countries.1,2 The increase in the severity of the acute bronchiolitis in infants born during the period of risk outlined in our study has a clear logic analyzed in relation to the knowledge about the seasonal fluctuation of virus antibodies7 and specifically against the RSV in pregnant.2 The risk of infection in the first months of life of the infant has been linked to the presence of antibodies in the mother.15 The risk of RSV hospitalization is higher for the 33–35 weeks old preterm babies, born between January and November in the Canadian collaborative study.16 Also, the risk of hospitalization is higher in preterm infants less than 35 weeks, born between October and December in Germany.16 In our study, it is not described the risk of hospitalization or infection, but we note the increased risk of severe disease progression of infection by RSV in infants previously healthy regardless of the other factors included in the study.
From the global perspective of different strategies for the prevention of infection with RSV in infants17 immunization of mothers against this virus during pregnancy seems today the best of them, since the infant vaccination offers problems, above all by the need of protective high titles of anti-RSV antibodies from the first days of life.18 Given that an optimum level of antibodies seems to protect against infection with RSV19 these must be transferred by the mother to the fetus before birth.3,19–21 Although it would be advisable to vaccinate also the infants later to maintain this protection during the period of greater risk of complicated infections or with the possibility of sequelae.
The strategy of vaccination of pregnant women is promising22,23 but it should be similar to environmental exposure, considering the half-life of the neutralizing against around 2.5 months RSV antibodies24 and estimation of the births of higher risk of severe disease progression, as it can be seen in our study. It should be considered that the effectiveness of vaccination in mothers will be related to the choice of optimal timing of vaccination in relation to childbirth.
We herein describe related risk factors for a severe disease progression which includes age less than 2 months, low weight at birth, gestational exposure to tobacco, presence of apneas, bacterial superinfection, severity of acute bronchiolitis and low food intake on admission. Although our study is a retrospective epidemiological research without measuring the level of maternal antibodies transferred to the newborn, this is a measurable indirect data of the increased risk of severe disease progression within the cases of acute bronchiolitis hospitalized by RSV which has not been included to date as risk factor at large series which investigating the risk of severe disease progression.13,14,25–29
The strengths of the study are the considerable sample of patients with acute bronchiolitis in a defined community with a same RSV exposition and a same beginning and end of the epidemic. It would be more difficult in a multicentre study. It is possible that mere titration of antibodies does not quantify the real protection that is transferred by the pregnant women exposed to the RSV since the studies focus on analyzing antibodies against the protein F or the viral G protein and is almost sure that maternal response to the RSV infection is more complex. So, the measurements in the newborn could not accurately test the level of protection against the RSV nor foresee the possibility of severe disease progression.30 Therefore, our research design has the advantage of its simplicity next to the physiological adjustment to the reality of the RSV infection in mothers and children. Retrospective selection of the cases included in the study makes possible to dismiss those cases whose bad evolution is due to other factors such as the bacterial superinfection and intercurrent illnesses.
The limitation of the study is mainly that we haven’t controlled some factors such as the very probable reality of viral co-infections that are been quantified around 30% of the acute bronchiolitis,31 although viral co-infection has not demonstrated an increase in the severity of the acute bronchiolitis in some reports.14
We conclude that birth during the period of risk with lower exposure of the pregnant woman to the RSV epidemic seems to increase the probability of severe disease progression of acute bronchiolitis.
FundingNo disclosure of funding received for this work.
Conflict of interestThe authors have no competing interests to declare.