To determine the aetiological agent causing a gastroenteritis outbreak in two hotels in Majorca (Spain) on August and September 2014.
MethodsAn epidemiological study was carried out. Environmental and stool samples were analyzed for different pathogens, including norovirus.
ResultsEpidemiological analysis detected 79 cases among the tourists hosted in the affected hotels over the period 18th August to 3rd September. They included 52 (attack rate: 6.4%) and 27 (attack rate: 3.0%) cases in hotel A and B, respectively. Seven of the staff members were also affected. Microbiological analyses detected genotype 2 norovirus in patient's stool samples, in rooms and in common areas’ surfaces. The specific control plan rapidly implemented at the beginning of the outbreak, and further adapted for norovirus elimination, allowed to control the outbreak.
ConclusionsOur study demonstrates that the outbreak was caused by genotype 2 norovirus, and reflects the importance of a rapid analysis and response for its control.
Determinar el agente etiológico responsable del brote de gastroenteritis producido en 2 hoteles de Mallorca (España) en agosto y septiembre de 2014.
MétodosSe realizó un estudio epidemiológico y se analizaron muestras ambientales y de heces para la presencia de patógenos, incluyendo norovirus.
ResultadosEl análisis epidemiológico detectó 79 casos entre los clientes hospedados en los hoteles desde el 18 de agosto al 3 de septiembre: 52 en el hotel A (tasa de ataque: 6,4%) y 27 en el B (tasa de ataque: 3,0%), así como en 7 miembros del personal. Los análisis microbiológicos detectaron norovirus genotipo 2 en las heces de los pacientes y en las superficies de las habitaciones y zonas comunes. El plan específico implementado rápidamente y adaptado para la eliminación de norovirus permitió el control del brote.
ConclusionesEn este brote causado por norovirus del genotipo 2 se refleja la importancia de un análisis y una respuesta rápida para su control.
Noroviruses are a leading cause of gastroenteritis outbreaks worldwide, in particular those related to closed or semi-closed communities like hospitals, cruises and hotels.1–4 The prevention and control of these outbreaks is specially complicated because the characteristics of norovirus make them almost perfect human pathogens.2 The infectious dose of norovirus is very low,5 viral shedding in faeces is high and may last up to 3 weeks after the resolution of symptoms.6 Therefore, people where clinical manifestations have disappeared remain still infective and may become a new source of infection. The environmental stability of this group of virus is also high, and their routes of transmission include person-to-person, water, food, vomits and fomites.3,4
Different strategies aimed at preventing and controlling norovirus outbreaks are followed when facing this problem.1,7 Ideally, outbreak management guidelines would be supported by high-quality empirical evidence. However, generating high-quality evidence for efficacy is difficult, as the evidence for outbreak management is largely empirical.8 Implementation of these measures is not always effective9 and outbreak cannot be controlled.
A possible gastroenteritis outbreak in two hotels located in Majorca was reported on 21st August 2014. Norovirus was suspected as the most probable aetiological agent responsible for the outbreak. This study aimed to demonstrate the role of norovirus in this gastroenteritis outbreak.
MethodsA case was defined as any guest or employee of hotel A or B in Majorca with acute onset of at least two of the following symptoms: diarrhoea, vomiting, abdominal clumps, or fever (>37°C). The period considered ranged from 18th August to 7th September 2014. Cases were identified through the symptoms and epidemiological questionnaires by the medical staff and the Health & Safety Department of the two affected hotels.
Bacteriological analyses of environmental samples were performed as previously described.10 Food samples were analyzed for total aerobic count (TAC), enterobacteria, Escherichia coli and other lactose fermenting Enterobacteriaceae, Staphylococcus aureus, Salmonella and Listeria. Drinking water and juices from the self-service machines were tested for TAC, E. coli and other coliforms, and for Clostridium perfringens. Ice cubes and pool water were also analyzed for E. coli and other coliforms.
Stool samples were analyzed for intestinal pathogens, including members of Salmonella, Shigella, Yersinia, Cryptosporidium, as in Ref.10 Norovirus was studied in stool, surface and water samples following the methodology described in Ref.11 Water samples were concentrated by filtration previous to the RNA isolation.
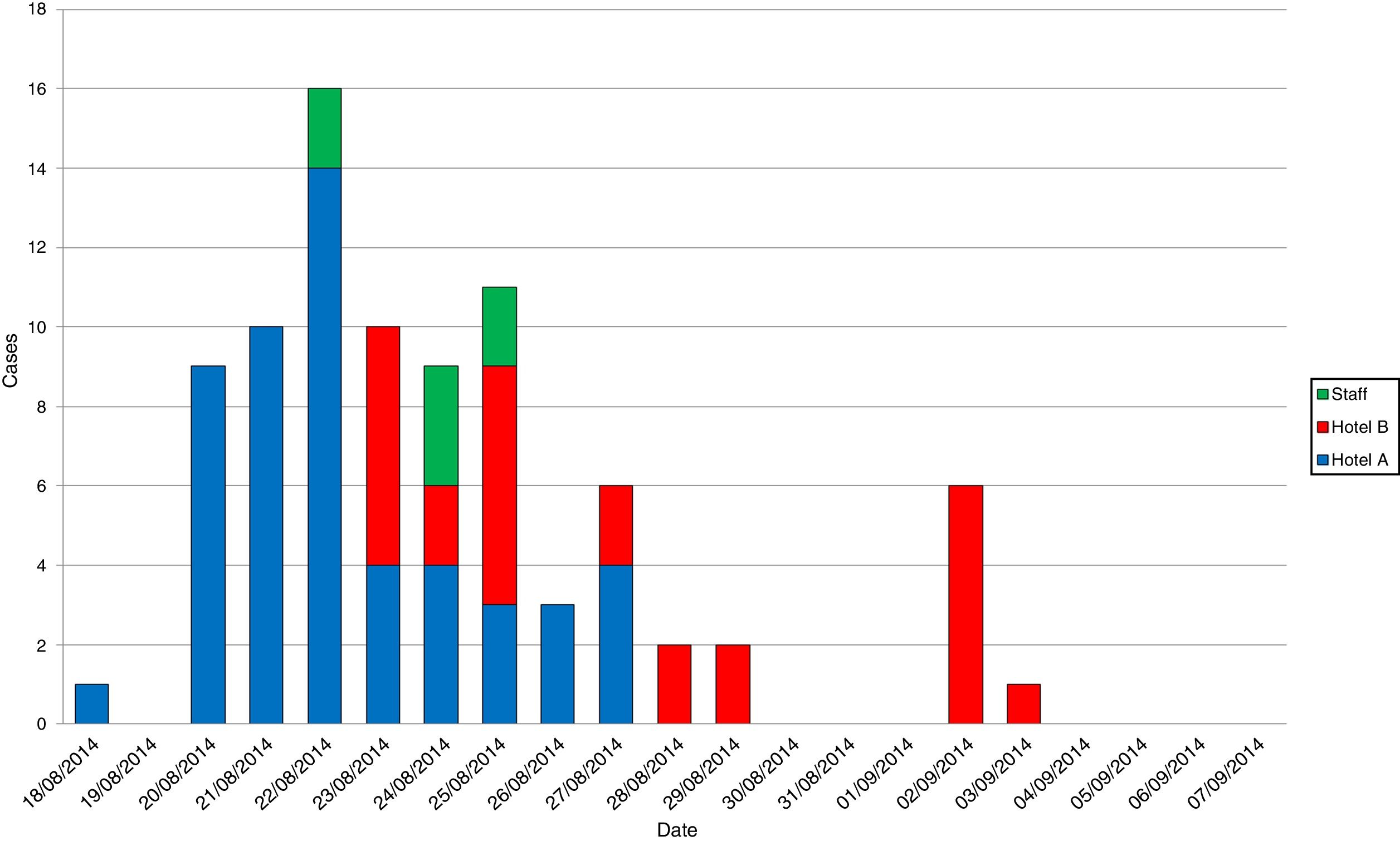
ResultsThe epidemiological investigation detected a total of 86 cases with onset of symptoms from 18th August to 3rd September. Seventy-nine cases (91.9%) affected to tourists: 52 (60.5%) and 27 (31.4%) cases in hotels A and B, respectively. In the 17-day outbreak period, 1715 guests were hosted in the two hotels: 815 in hotel A and 900 in hotel B. Overall, attack rate for guests was 4.6% (79 cases), 6.4% for hotel A and 3.0% for hotel B. The 282 staff worked in both hotel A and B. Gastroenteritis symptoms were informed by 7 of them (attack rate 2.5%), being separated from service to customers until the outbreak was solved. Symptoms were mainly vomiting and diarrhoea, and duration of symptoms was 1–3 days. Fig. 1 shows the evolution of cases during the outbreak. Initially, a woman hosted in hotel A was affected by abdominal pain and vomits on 18th August. Nine new cases appeared among guest of the same hotel two days later, increasing the number in the following days (about 10 new cases per day). A peak of 16 new patients arise on 22nd August, including two staff members, and hotel B guests began to be affected on the 23rd August. To note, cases with affected relatives, usually on different days, included 26 of the 79 affected clients (33%). Cases seemed to be controlled on 30th August, but a new peak arose on 2nd September. Finally, last case was detected on 3rd September.
Microbiological analyses were performed to determine the aetiological agent of the outbreak, using both clinical and environmental samples. Stool samples from three adult patients (two guests and one employee) were taken during the acute phase of the gastroenteritis for culture. Genotype 2 norovirus was detected in 2 of the 3 samples, all other pathogens testing negative.
Bacteriological levels of environmental samples on 18th August were acceptable in all cases, ruling out their role as a source of infection. Days later, as the outbreak remained active, surface and water samples were analyzed for norovirus. In patients’ rooms, surfaces frequently fingered were swabbed before and after cleaning in all cases. Computer's keyboards and mousses, elevators’ and vending machines’ keypads were selected in the hall area. Surfaces from the nursery and the zones for entertainment activities were also chosen. Finally, drinking water from the self-service machines was also analyzed. Norovirus was detected in the four rooms sampled before cleaning, remaining two of them positive after cleaning. Elevators’ keypads were also contaminated with norovirus. The rest of samples from the hall area, the nursery and the zones for entertainment activities, and drinking water tested negative.
Regarding the control procedures, a specific plan for norovirus control was rapidly implemented. Enhanced hand hygiene practices were established among staff and guests, including hand sanitizer gel dispensers in common areas; special care was observed in the restaurant area, where hand sanitizing was mandatory before entering the buffet zone, raw food was removed from the buffet and cutlery was protected. Cleaning and disinfection of frequently contacted surfaces (doorknobs, phone keys, etc.) with alcohol 70% or bleach were performed. Toilets were also frequently treated with bleach, as flushing results in the formation of droplets or aerosols than may disseminated the virus through the air.12
Special concern was taken at the children club and patients’ rooms. In the last ones, access was blocked for at least 24h after cleaning, leaving the balcony open for the renovation of the air and allowing sunlight to penetrate the room. General guidelines included: mopping for floor cleaning; long programme of the washing machine for virus inactivation in contaminated clothes; and use of masks, gloves and closed bags for vomits elimination. Additional measures were executed once environmental results were available. The use of vapour machines for inactivation of norovirus in carpets and curtains. Increase of disinfection with the use of Virkon® (JohnsonDiversey, Spain) as an alternative disinfectant: for hand contact surfaces, a solution of 1% (w/w) in water was applied. Moreover, a solution of 0.25% (w/w) in water was sprayed for air disinfection in zones where vomits occurred, as it is a well-known route of dissemination.13,14 The tablecloths were changed for one use only. Finally, new room keys used anytime a new client check-in the hotel.
DiscussionIn this report, we describe a gastroenteritis outbreak associated to a hotel caused by norovirus. Stool samples analysis demonstrated norovirus being present in 67% of the tested samples, and no additional pathogen was detected. These results demonstrate the aetiology of norovirus. Epidemiology data showed that a single guest in hotel A felt ill on 18th August. This person may be the source of the outbreak, as new cases appeared in the same hotel two days later, fitting the incubation period for norovirus infections.8 New cases appeared in the following days, with a peak of 16 new patients on 22nd August. Staff members started to become ill precisely on 22nd August, and hotel B guests began to be affected on the 23rd August. Thus, a worker may have introduced norovirus in hotel B before symptoms appeared. Virus may also disseminate by the common areas, as pathogen was present in elevators’ keypads. Check-in dates and onset and duration of symptoms of patients were compared, meeting the incubation period for contracting the illness in the establishments and/or with a secondary infection from a sick relative. Interpersonal transmission, recurrent in norovirus outbreaks,15 was important in this outbreak since cases with affected relatives were frequent during the outbreak.
Control measures implemented on 22nd August and optimized later allowed the outbreak to be controlled almost in a week. Although a new small peak arose on 2nd September, it affected a single family, and last case was detected on 3rd September.
In summary, this study describes a gastroenteritis outbreak caused by norovirus in two hotels. This case reflects the importance of rapid analysis and response to control the outbreaks caused by norovirus in hotels, avoiding extreme measures like closure when outbreak becomes out of control.9
Conflict of interestAuthor declares that any funding was received for this study and data was generated as part of routine activities. Any conflicting or dual interests apply to the present manuscript.