A retrospective study was conducted to investigate the usefulness of systematic quantitative blood culture (QBC) in the diagnosis of catheter-related bloodstream infection (CRBSI) during two 1-year periods (2002 and 2012).
MethodsThe study included all QBC requests sent to the microbiology laboratory for suspected CRBSI in adults (≥18 years) with any type of intravascular catheter (IVC). Based on a ratio of ≥4:1CFU/mL of the same microorganism between IVC blood culture from any lumen and peripheral blood culture, 5 diagnostic groups were defined: confirmed or probable CRBSI, primary BSI, other focus of infection, and colonization.
ResultsIn total, 4521 QBCs were evaluated; 24% positive in 2002 and 16% in 2012 (P<0.0001). There were 243 episodes of suspected CRBSI (101 in 2002 and 142 in 2012). Confirmed CRBSI episodes were higher in 2002 than 2012 (56% vs 34%) (P<0.0001), whereas colonization episodes were lower (18% vs 38%) (P=0.0006). Gram-positive cocci decrease in 2012 relative to 2002 (56% vs 79.7%) (P=0.022). Almost one-third (32%) of confirmed CRBSI would have been missed if blood from all catheter lumens had not been cultured.
ConclusionsQBC is a useful method for diagnosing CRBSI. Blood samples from all catheter lumens must be cultured to avoid missing around one-third of CRBSI diagnoses.
Se ha realizado un estudio retrospectivo, para investigar la utilidad del hemocultivo cuantitativo (HC) para el diagnóstico de las bacteriemias relacionadas con catéteres (BRC), durante dos periodos de un año (2002 y 2012).
MétodosTodos los HC recibidos en el laboratorio de microbiología realizados ante la sospecha de BRC, a pacientes ≥18 años portadores de cualquier tipo de catéter intravascular (CIV), han sido incluidos en este estudio. Basándonos en la proporción ≥4:1CFU/mL del mismo microorganismo entre el HC de cualquier luz del CIV y el HC periférico se han definido 5 grupos diagnósticos: BRC confirmada o probable, bacteriemia primaria, otro foco de infección y colonización.
ResultadosHan sido evaluados 4521 HC; 24% positivos en 2002 y 16% en 2012 (P<0.0001). Fueron sospechosos de BRC 243 episodios (101 en 2002 y 142 en 2012). El Porcentaje de episodios de BRC confirmados fue mayor en 2002 que en 2012 (56% vs 34%) (P<0.0001), en cambio fue menor el de los episodios de colonización (18% vs 38%) (P=0.0006). Los cocos Gram-positivos disminuyeron en 2012 en relación con 2002 (56% vs 79.7%) (P=0.022). En el 32.2% de las BRC confirmadas se hubiese perdido el diagnóstico si no se hubiera realizado HC de todas las luces.
ConclusionesEl HC es un método muy útil para el diagnóstico de las BRC. Hay que obtener muestra de sangre de todas luces para cultivo con el fin de evitar la pérdida de alrededor del 30% de los episodios de BRC.
Intravascular catheters (IVCs) are commonly used in most medical centers. These devices are not only applied in hospitalized and emergency patients for administration of intravenous fluids or medication, but also in outpatients. A great variety of IVCs are available and all types are susceptible to colonization by microorganisms. The incidence of catheter-related bloodstream infection (CRBSI) is estimated at 0.1 to 5/1000 catheter-days.1–4 Once a long-term catheter is successfully placed, attempts are made to maintain it as long as it is needed, as replacement is not without risk and another suitable vascular access may not be available.
Three methods are currently used for diagnosing CRBSI without removing the IVC: quantitative blood culture (pour plate method),5 semiquantitative blood culture (lysis-centrifugation),6–9 and qualitative blood culture, using differential time to positivity on an automatic system.7–10 Since 1988, quantitative blood culture (QBC) has been used in our center (sensitivity of 94%, specificity of 100%).5 The aims of this study are to determine the usefulness of this technique in two different periods: that is, to know what percentage of QBCs enable a microbiological diagnosis of CRBSI, to ascertain the IVC colonization rate in our setting, and to determine the percentage of CRBSI diagnoses that would have been missed if QBC had not been performed in all catheters or lumens in patients using several devices or IVCs with 2 or more lumens.
Material and methodsA retrospective observational study investigating the usefulness of our QBC method for the diagnosis of CRBSI was carried out in Vall d’Hebron Hospital (Barcelona, Spain), a 1000-bed reference hospital within the publically-funded health system. Two years were analyzed and compared: 2002 and 2012.
PatientsThe study included all QBC requests sent to the Microbiology Department for adult patients (≥18 years) using 1 or more IVCs, including 1-lumen or ≥2-lumen devices, multiple catheterizations, or Port-A-Cath (PAC) catheters. All culturing procedure protocols in which the IVC QBC was erroneously identified or peripheral blood culture was not carried out were excluded from the analysis.
Sample collectionIn each patient, samples containing 1–3mL of blood for QBC were taken through all the IVC lumens and placed in sterile tubes containing sodium polyanetholesulphonate as anticoagulant (SPS tubes, reference 745452, Imunohealth S.L. Alella, Barcelona, Spain). At the same time, a blood sample of >12mL was drawn from a peripheral vein, 1–3mL was inoculated in a QBC tube, and the remainder was placed in bottles for qualitative culture (aerobic and anaerobic medium, Bact/Alert 3D bioMérieux, Marcy L’Etoile, France). QBC follow-up of the CRBSI episodes was done only on samples from IVC lumens.
Quantitative methodFor each QBC, 1–3mL of blood was mixed with 20mL of previously melted (water bath or microwave at defrosting position for 1minute) brain heart infusion agar at ∼56°C in petri plates. After letting the plates stand for 20minutes at room temperature, they were incubated aerobically for 4 days at 35–37°C. The remaining sample was stored at 5–7°C. All QBCs were examined daily for growth. The number of colonies recovered was estimated using the rule of three calculation and expressed as colony-forming units per mL (CFU/mL). When the count was >1000CFU/mL, QBC was repeated on a sheep blood agar plate using a 1:1000 calibrated loop with the stored blood to provide a more precise count. In addition, Gram staining was done. Subculturing was performed on sheep blood agar and selective medium according to the morphology of the organism observed on Gram stain. Conventional methods were used for the preliminary identification11 and the Vitek 2 System (bioMérieux, Marcy L’Etoile, France) for definitive identification. Antimicrobial susceptibility was assessed according to the Clinical and Laboratory Standards Institute (CLSI) recommendations, using Mueller–Hinton agar (Kirby Bauer diffusion method) and Rosco disks (neo-Sensitab; Rosco Diagnostica, Taastrup, Denmark). The microorganisms isolated from the catheter(s) and peripheral blood were considered identical when the genus, species, biotype, and antibiotype coincided.
DefinitionsBased on the ratio between the CFU/mL count of the same microorganism (species and antibiotype) isolated in the peripheral blood QBC and the QBCs from each different IVC lumen,5 five groups were defined to classify each episode:
- I.
Confirmed catheter-related bloodstream infection: simultaneous QBCs in which the number of CFU/mL isolated from blood drawn from any lumen of the patient's IVC(s) was ≥4-fold the number isolated from peripheral blood.
- II.
Probable catheter-related bloodstream infection: QBCs in which the number of CFU/mL isolated from blood drawn from all lumens of the patient's IVC(s) was in no case ≥4-fold the number found on peripheral blood culture, but the same microorganism was simultaneously isolated on culture of purulent drainage at the insertion site or semiquantitative culture of a catheter tip using the Maki method (≥15CFU).12
- III.
Primary bloodstream infection: QBCs in which the number of CFU/mL isolated from blood drawn from all lumens of the patient's IVC(s) was in no case ≥4-fold the number found on peripheral blood culture and no other source of bloodstream infection was found.
- IV.
Bloodstream infection due to another origin: QBCs in which the number of CFU/mL isolated from blood drawn from all lumens of the patient's IVC(s) was in no case ≥4-fold the number found on peripheral blood culture, and the same microorganism (same species and antibiotype) was found on culture of samples from another source of infection.
- V.
Colonization: Culture of samples from one or various IVC lumens was positive, but peripheral blood qualitative and quantitative cultures were negative.
Procedure protocol: All blood samples were drawn from all lumens of all the patient's IVCs and were cultured at the same time as the qualitative and quantitative peripheral blood cultures.
Reinfection: Following antimicrobial treatment for one episode of bloodstream infection, the patient experienced one or more additional episodes caused by a different microorganism or the same microorganism with a different antibiotype.
Recurrence: Following antimicrobial treatment for one episode of bloodstream infection, the patient experienced one or more additional episodes caused by the same microorganism (same species and antibiotype) or the same microorganism differing in susceptibility to only one antimicrobial.
Statistical analysisCategorical variables were expressed in absolute frequencies and percentages, and comparisons between the two study time periods were performed with the chi-square test or Fisher exact test, as appropriate. A P value <0.05 was considered statistically significant. Statistical analyses were carried out using Epi Info 7 (CDC, Available at: http://wwwn.cdc.gov/epiinfo/7/index.htm. Accessed: March, 20, 2015).
ResultsA total of 4521 QBCs performed to investigate suspected CRBSI were included in the study, 1996 performed in 2002 (409 patients) and 2525 (1026 patients) in 2012. QBCs were positive in 24% (476/1996) in 2002 and 16% (415/2525) in 2012 (P<0.0001). The larger number of QBCs performed in 2012 correspond to the Hematology Department (855 vs 638), Emergency Department (701 vs 45), and outpatient facilities (85 vs 10).
The percentage of positive QBCs in 2012 was found to have significantly decreased relative to 2002 in the Hematology (9.4% vs 20.03%) (P<0.0001) and Emergency Departments (21.6% vs 40%) (P=0.004). The number of QBCs carried out in the ICU and Nephrology Department decreased between the 2 time periods, (162 vs 426 and 191 vs 274, respectively), and there was also a decline in the proportion of positive QBCs in these 2 hospital areas, with a significant difference in the Nephrology Department (8.9% vs 23.3%) (P<0.0001).
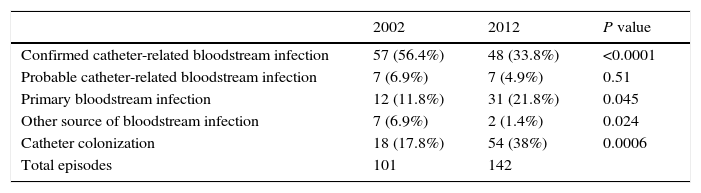
We excluded 71 procedure protocols, 16 in 2002 and 55 in 2012 (69% because the peripheral QBC was lacking and 31% because of erroneous sample identification). In total, 243 episodes of suspected CRBSI were analyzed (Table 1). The proportion of confirmed CRBSI was significantly higher in 2002 than in 2012 (56% vs 34%; P<0.0001), whereas the proportion of colonization episodes was lower (18% vs 38%; P=0.0006).
Results of quantitative culture to investigate suspected catheter-related bloodstream infection (2002 and 2012).
| 2002 | 2012 | P value | |
|---|---|---|---|
| Confirmed catheter-related bloodstream infection | 57 (56.4%) | 48 (33.8%) | <0.0001 |
| Probable catheter-related bloodstream infection | 7 (6.9%) | 7 (4.9%) | 0.51 |
| Primary bloodstream infection | 12 (11.8%) | 31 (21.8%) | 0.045 |
| Other source of bloodstream infection | 7 (6.9%) | 2 (1.4%) | 0.024 |
| Catheter colonization | 18 (17.8%) | 54 (38%) | 0.0006 |
| Total episodes | 101 | 142 |
There were 14 episodes of probable CRBSI, 7 in 2002 and 7 in 2012. In 8 episodes, the IVC was removed, and in 6 episodes, the skin surface or purulent drainage culture was positive for the same microorganism. Twelve episodes were considered a primary bloodstream infection in 2002 and 31 in 2012. Sources of infection other than the catheter accounted for 7 episodes of bloodstream infection in 2002, and 2 in 2012.
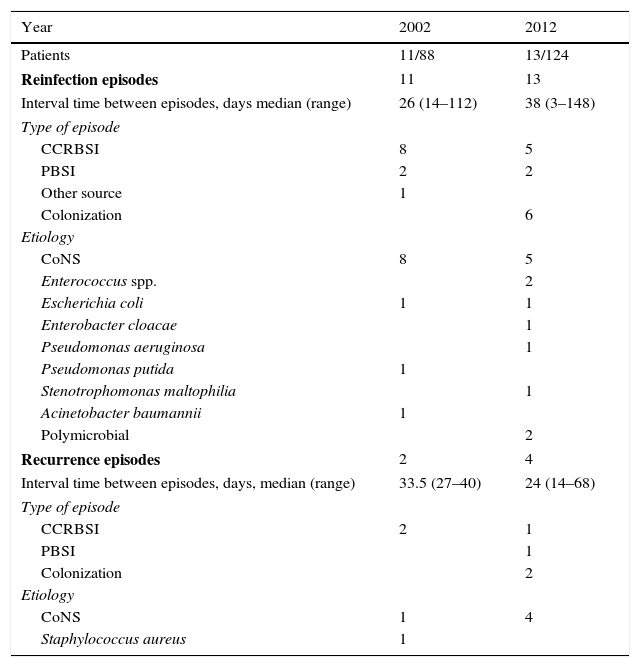
The percentage of patients experiencing ≥2 episodes of BSI was 12% (11/88) in 2002 (9 patients had 2, and 2 patients had 3 episodes), and 10.5% (13/124) in 2012 (11 had 2, and 2 had 4 episodes) (Table 2). In both 2002 and 2012, 10 patients underwent IVC removal after each episode. One patient had a recurrence of confirmed CRBSI caused by cloxacillin-susceptible Staphylococcus aureus. The IVC was removed in each episode and tip culture was negative; however, the same microorganism was isolated in the purulent drainage at the insertion site.
Patients with 2 or more episodes (2002 and 2012).
| Year | 2002 | 2012 |
|---|---|---|
| Patients | 11/88 | 13/124 |
| Reinfection episodes | 11 | 13 |
| Interval time between episodes, days median (range) | 26 (14–112) | 38 (3–148) |
| Type of episode | ||
| CCRBSI | 8 | 5 |
| PBSI | 2 | 2 |
| Other source | 1 | |
| Colonization | 6 | |
| Etiology | ||
| CoNS | 8 | 5 |
| Enterococcus spp. | 2 | |
| Escherichia coli | 1 | 1 |
| Enterobacter cloacae | 1 | |
| Pseudomonas aeruginosa | 1 | |
| Pseudomonas putida | 1 | |
| Stenotrophomonas maltophilia | 1 | |
| Acinetobacter baumannii | 1 | |
| Polymicrobial | 2 | |
| Recurrence episodes | 2 | 4 |
| Interval time between episodes, days, median (range) | 33.5 (27–40) | 24 (14–68) |
| Type of episode | ||
| CCRBSI | 2 | 1 |
| PBSI | 1 | |
| Colonization | 2 | |
| Etiology | ||
| CoNS | 1 | 4 |
| Staphylococcus aureus | 1 | |
CCRBSI, confirmed catheter-related bloodstream infection; PBSI, primary bloodstream infection; CoNS, coagulase-negative staphylococci.
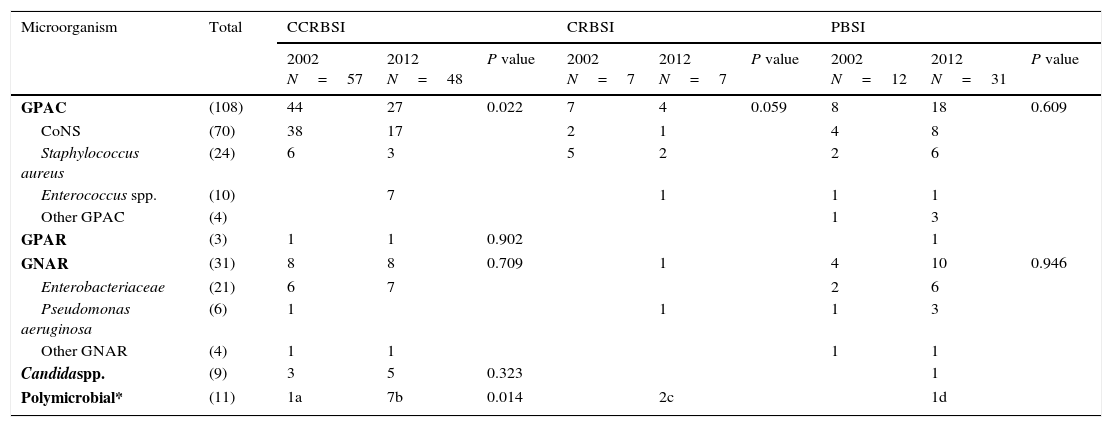
The causative microorganisms of the bloodstream infection episodes documented are shown in Table 3. Gram-positive aerobic cocci were the most commonly isolated pathogens in both periods. These microorganisms accounted for 77.2% (44/57) of confirmed CRBSI in 2002 versus 56.2% (27/48) in 2012 (P=0.022). Eight episodes of confirmed CRBSI were polymicrobial: 1 (1.7%) in 2002 and 7 (14.6%) in 2012.
Etiology of catheter-related bloodstream infections (2002 and 2012).
| Microorganism | Total | CCRBSI | CRBSI | PBSI | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 2002 N=57 | 2012 N=48 | P value | 2002 N=7 | 2012 N=7 | P value | 2002 N=12 | 2012 N=31 | P value | ||
| GPAC | (108) | 44 | 27 | 0.022 | 7 | 4 | 0.059 | 8 | 18 | 0.609 |
| CoNS | (70) | 38 | 17 | 2 | 1 | 4 | 8 | |||
| Staphylococcus aureus | (24) | 6 | 3 | 5 | 2 | 2 | 6 | |||
| Enterococcus spp. | (10) | 7 | 1 | 1 | 1 | |||||
| Other GPAC | (4) | 1 | 3 | |||||||
| GPAR | (3) | 1 | 1 | 0.902 | 1 | |||||
| GNAR | (31) | 8 | 8 | 0.709 | 1 | 4 | 10 | 0.946 | ||
| Enterobacteriaceae | (21) | 6 | 7 | 2 | 6 | |||||
| Pseudomonas aeruginosa | (6) | 1 | 1 | 1 | 3 | |||||
| Other GNAR | (4) | 1 | 1 | 1 | 1 | |||||
| Candidaspp. | (9) | 3 | 5 | 0.323 | 1 | |||||
| Polymicrobial* | (11) | 1a | 7b | 0.014 | 2c | 1d | ||||
CCRBSI, confirmed catheter-related bloodstream infection; PCRBSI, probable catheter-related bloodstream infection; PBSI, primary bloodstream infection; GPAC, gram-positive aerobic cocci; CoNS, coagulase-negative staphylococci; GPAR, gram-positive aerobic rod; GNAR, gram-negative aerobic rod; *1a, C. albicans+C. tropicalis, 1; 7b, CoNS+S. aureus, 1; CoNS+E. faecalis, 1; CoNS+Enterobacter spp., 1; E. coli+K. pneumoniae, 1; E. coli+Proteus mirabilis, 1; K. pneumoniae+P. aeruginosa, 1; K. pneumoniae+P. mirabilis+E. faecalis spp., 1; 2c, E. coli+K. pneumoniae+P. mirabilis, 1; E. coli+Enterobacter spp.+P. aeruginosa; 1d=E. coli+E. faecium
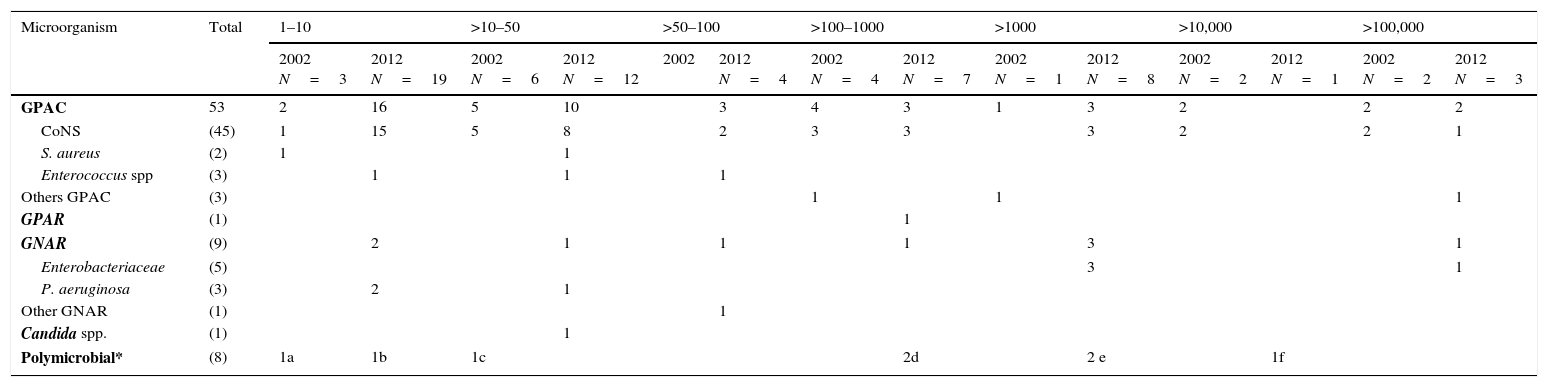
There were 72 episodes of colonization without bloodstream infection: 18 in 2002 versus 54 in 2012 (Table 4). In total, 23.6% (17/72) of patients with catheter colonization had one or several positive QBCs with >1000CFU/mL: 27.8% (5/18) in 2002 versus 22.2% (12/54) in 2012. Gram-positive aerobic cocci were the microorganisms most commonly isolated in colonizations in both periods: 88.9% (16/18) in 2002 versus 68.5% (37/54) in 2012.
Etiology of 72 episodes of colonization and CFU/mL (2002 and 2012).
| Microorganism | Total | 1–10 | >10–50 | >50–100 | >100–1000 | >1000 | >10,000 | >100,000 | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2002 N=3 | 2012 N=19 | 2002 N=6 | 2012 N=12 | 2002 | 2012 N=4 | 2002 N=4 | 2012 N=7 | 2002 N=1 | 2012 N=8 | 2002 N=2 | 2012 N=1 | 2002 N=2 | 2012 N=3 | ||
| GPAC | 53 | 2 | 16 | 5 | 10 | 3 | 4 | 3 | 1 | 3 | 2 | 2 | 2 | ||
| CoNS | (45) | 1 | 15 | 5 | 8 | 2 | 3 | 3 | 3 | 2 | 2 | 1 | |||
| S. aureus | (2) | 1 | 1 | ||||||||||||
| Enterococcus spp | (3) | 1 | 1 | 1 | |||||||||||
| Others GPAC | (3) | 1 | 1 | 1 | |||||||||||
| GPAR | (1) | 1 | |||||||||||||
| GNAR | (9) | 2 | 1 | 1 | 1 | 3 | 1 | ||||||||
| Enterobacteriaceae | (5) | 3 | 1 | ||||||||||||
| P. aeruginosa | (3) | 2 | 1 | ||||||||||||
| Other GNAR | (1) | 1 | |||||||||||||
| Candida spp. | (1) | 1 | |||||||||||||
| Polymicrobial* | (8) | 1a | 1b | 1c | 2d | 2 e | 1f | ||||||||
CFU, colony forming units; GPAC, gram-positive aerobic cocci; CoNS, coagulase-negative staphylococci; GPAR, gram-positive aerobic rod; GNAR, gram-negative aerobic rod; *1a, CoNS+S. aureus; 1b, CoNS+Bacillus spp.; 1c, CoNS+Enterococcus spp.+Bacillus spp.; 2d, CoNS+E. faecalis and CoNS+K. pneumoniae; 2e, CoNS+E. faecalis and CoNS+K. pneumoniae+P. aeruginosa; 1f, CoNS+Acinetobacter spp.
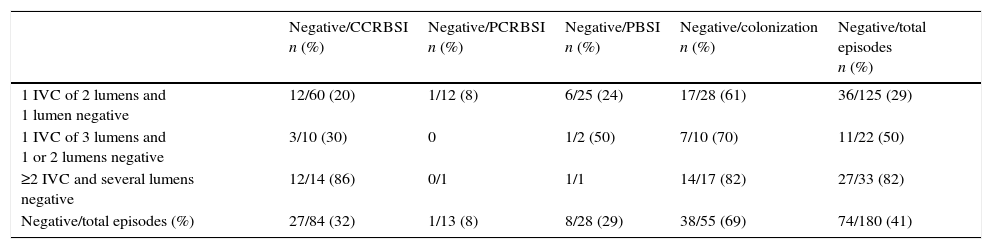
We divided the number of positive QBCs by the total number of QBCs performed per episode in patients with multilumen and several IVCs to calculate the percentage of diagnoses that would have been missed if culture of blood drawn from all lumens of all IVCs had not been done (Table 5). A total of 180/243 episodes were included (30 PACs, 24 single-lumen IVCs, and 9 sources of BSI other than IVCs were excluded). In 41% (74/180) of the episodes studied, QBC for at least one of the IVC lumens tested negative. Therefore, 32% of confirmed CRBSI diagnoses would have been missed.
Catheter-related bloodstream infections that would have been missed if samples from all catheter lumens had not been cultured.
| Negative/CCRBSI n (%) | Negative/PCRBSI n (%) | Negative/PBSI n (%) | Negative/colonization n (%) | Negative/total episodes n (%) | |
|---|---|---|---|---|---|
| 1 IVC of 2 lumens and 1 lumen negative | 12/60 (20) | 1/12 (8) | 6/25 (24) | 17/28 (61) | 36/125 (29) |
| 1 IVC of 3 lumens and 1 or 2 lumens negative | 3/10 (30) | 0 | 1/2 (50) | 7/10 (70) | 11/22 (50) |
| ≥2 IVC and several lumens negative | 12/14 (86) | 0/1 | 1/1 | 14/17 (82) | 27/33 (82) |
| Negative/total episodes (%) | 27/84 (32) | 1/13 (8) | 8/28 (29) | 38/55 (69) | 74/180 (41) |
IVC, intravascular catheter; CCRBSI, confirmed catheter-related bloodstream infection; PCRBSI, probable catheter-related bloodstream infection; PBSI, primary bloodstream infection.
The present study, together with our previous one,5 has enabled us to confirm the continuing utility of the QBC technique applied in our hospital to diagnose or rule out CRBSI. Of particular note, the results illustrate the importance of obtaining samples from each and every lumen of the patient's IVCs to avoid missed diagnoses. Over the years we have continued to use the same criterion for the diagnosis of CRBSI: simultaneous QBCs in which the number of CFU/mL isolated from blood drawn from any lumen of the patient's IVC(s) was ≥4-fold the number isolated from peripheral blood.
A 26% increase in the total number of QBCs carried out in our laboratory was documented in the second study period (2012) relative to the first (2002). This is likely because the health staff are highly aware of the need for prompt culturing at the slightest suspicion of CRBSI in patients hospitalized in the Hematology Department and in all patients with central lines in the Emergency Department and outpatient clinic.
Several interventions implemented in our hospital may have contributed to the reduction in positive QBC results between the two periods: educational programs for the staff, guidelines for insertion and handling of vascular accesses to prevent CRBSI,13 and implementation the Bacteremia Zero project, first applied in our ICUs and later extended to the whole hospital. Introduction of the Bacteremia Zero project in 2009 throughout the autonomous community of Catalonia was associated with a >40% decline in ICU CRBSI rates, reaching values of 3.04 episodes per 1000 catheter-days in hospitals with >500 beds.14
The percentage of patients experiencing several BSI episodes was similar in the 2 periods (12.5% in 2002 vs 10.5% in 2012). In both periods in our study, the number of reinfections was greater than the number of recurrences. Molecular biology techniques are essential to confirm that different isolates belong to the same strain, especially in patients with several episodes caused by the same species.9,15 These techniques can help in the decision of whether to remove or retain the catheter, particularly in patients with long-term catheters.
Gram-positive cocci continued to be the most common cause of CRBSI3,16 affecting 56% of cases in 2012, with a decrease relative to 2002 (79.7%). Among these cases, coagulase-negative staphylococci (CoNS) remained the most frequent causative pathogens, as has been seen in other European countries,3 although their incidence also decreased in 2012.
In the analysis of colonization episodes, an increase was detected in 2012 compared to 2002 and the percentage we found is higher than the value reported by other authors.17 The above-mentioned preventive measures and QBC analysis of IVCs at the slightest suspicion of catheter-related infection are likely to have contributed to greater detection of colonization episodes in 2012. A high degree of colonization (>1000CFU/mL) was found in 24% of colonization episodes. Although peripheral blood cultures were negative in these cases and CRBSI was not demonstrated, patients may have had intermittent bloodstream infection. S. aureus was not isolated in any of these high-colonization episodes. As occurred with CRBSI, CoNS were the microorganisms most commonly found.
In the Infectious Diseases Society of America 2009 guidelines, blood culture of all device lumens was categorized as a CIII recommendation because at the time, the available data did not suffice to advocate this practice.13 Nonetheless, our results show that QBC of blood samples drawn from all lumens in patients with multilumen catheters or several IVCs enabled more accurate diagnosis of CRBSI and colonization in both study periods. Previous studies have estimated proportions of 15–37% of missed CRBSI diagnoses when blood culture from all lumens is not performed.18–21
In our study, the estimated proportion of confirmed CRBSI diagnoses that would have been missed was 32%. Guembe et al. 19 found that failure to culture 1 lumen in IVCs having 2 or 3 lumens would have missed the diagnosis in 27.2% and 15.8% of CRBSI episodes, respectively. In our patients, the proportion of missed confirmed diagnoses would have been 20% of cases in ICVs having 2 lumens, 30% in those with 3 lumens, and 86% of those occurring in patients with 3 or more catheters. In addition, in polymicrobial episodes in which the microorganisms isolated were not the same in all the catheter lumens, the method we used enabled us to know which lumen was responsible for the infection.
In a group of pediatric patients, Acuña et al. 22 reported better results using the differential time to positivity technique with a 1.5-mL blood sample than QBC using a 0.5-mL sample inoculated on a 5% sheep blood agar plate. It would be expected that superior results would be obtained with differential time positivity because the sample volume was 3-fold larger. It is well recognized that a <0.5mL volume is insufficient to diagnose bloodstream infection with blood culture. In a pediatric study, Kellogg et al. detected concentrations of <1CFU/mL in 23% of children with BSI.23
We believe that QBC has several advantage over other methods used for the diagnosis of CRBSI. Is a simple technique commonly used in microbiological laboratories. The volume of blood needed for each QBC is smaller (1–3mL) than that used in the semiquantitative lysis-centrifugation method or the differential time to positivity method,9,10 which require around 10mL.7,9,15–17 Nor is an equal volume of blood needed for each sample, as is the case of the differential time to positivity method.6–9 These advantages imply less invasiveness for the patient and a lower risk of anemia, which can be a limiting factor in the follow-up of these patients.
Although a cost-analysis was not performed in this study, the quantitative method we use is generally considered less expensive than semiquantitative or qualitative automated methods. The tubes we use cost 250 € per box of 100. This factor is of particular importance when several catheters need to be analyzed in a single patient.
In our hospital, the use of QBC for diagnosing CRBSI in the Postoperative Cardiac Surgery Unit and ICU enabled exclusive removal of the IVC causing the infection while the others could be retained for an additional 2 or 3 days. Furthermore, long-term central or tunneled catheters could be retained in 82% to 100% of patients with the use of QBC plus antibiotic-lock therapy.24,25
This study has the limitations of a retrospective design. The data analyzed were obtained from the Microbiology database and later confirmed according to the information contained in the hospital medical records. However, all CRBSI episodes were well documented, as they had been prospectively evaluated by staff members of the Infectious Diseases Department. Another limitation is that molecular biology techniques had not been used to conclusively determine the strain involved in cases of recurrence or reinfection. Nonetheless, the antibiotype is considered a good marker in daily practice. For the same reason, in cases of colonization, we were unable to determine whether the CoNS species found was the same as the one subsequently causing CRBSI. Prospective studies that follow the colonization process in patients with tunneled IVCs and PACs including DNA genotyping of the strains found and determination of their biofilm production could be of great value.
In summary, the results of our study demonstrate the utility of quantitative blood culture to diagnose CRBSI and promptly detect catheter colonization. It is a simple, relatively economic method that requires a much smaller amount of blood for each culture than other methods used for this purpose, making it a less invasive test for patients. Of particular note, our results indicate that quantitative culture should be performed on samples from all lumens of all the patient's devices, as this practice diagnosed a large percentage of infections that otherwise may have been missed.
Conflict of interest statementThe authors declare no conflict of interest.
The authors are grateful to the hospital nursing and the microbiology staff, to J.J. González-López for providing helpful comments during the writing of the manuscript and to C. Cavallo for language support.