We report a case of Zika virus (ZIKV) infection in a patient with diarrhea, fever, synovitis, non-purulent conjunctivitis, and with discreet retro-orbital pain, after returning from Colombia in January 2016. The patient referred several mosquito bites. Presence of ZIKV was detected by PCR (polymerase chain reaction) in plasma. Rapid microbiological diagnosis of ZIKV infection is needed in European countries with circulation of its vector, in order to avoid autochthonous circulation. The recent association of ZIKV infection with abortion and microcephaly, and a Guillain-Barré syndrome highlights the need for laboratory differentiation of ZIKV from other virus infection. Women with potential risk for Zika virus infection who are pregnant or planning to become pregnant must mention that fact during prenatal visits in order to be evaluated and properly monitored.
Presentamos un caso de infección por virus Zika (ZIKV) en un paciente con diarrea, fiebre, sinovitis, conjuntivitis no purulenta, con discreto dolor retroorbital, después de regresar de Colombia en enero de 2016. El paciente refería múltiples picaduras de mosquito. La presencia de ZIKV fue detectada en plasma por reacción en cadena de la polimerasa (PCR). En los países europeos en los que exista circulación de su vector es necesario un diagnóstico microbiológico rápido de la infección por ZIKV para evitar transmisión autóctona. La asociación reciente de la infección por ZIKV con abortos y microcefalia y síndrome de Guillén-Barré pone de relieve la necesidad de la diferenciación de ZIKV de otras infecciones por virus. Las mujeres con riesgo potencial de infección por el virus Zika que están embarazadas o que planeen quedar embarazadas deben mencionar esa circunstancia durante las visitas prenatales con el fin de ser evaluadas y monitorizadas adecuadamente.
A 49 years-old man is being followed at our Hospital in Spain for a clinical history of irritable bowel syndrome, hypertension and dyslipidemia and he is under treatment telmisartan and atorvastatin.
The patient traveled to Colombia where he stayed between December, 2015 and January, 2016. The day of his return to Spain, he began with diarrhea (up to 8 watery stools without blood, mucus or pus) and temperature of 37.3°C. On January the patient was attended at our Hospital for signs of swelling in the right hand, arthralgia in fingers, right knee, ankle and elbow, and conjunctival injection with mild retro-orbital pain. He did not report headache, rash, myalgias, or urinary symptoms. The patient referred mosquito bites in Colombia.
Cutaneous lesions were not observed, but there was evidence of synovitis at the proximal interphalangeal joint of the first finger of his right hand with no other significant exploratory signs.
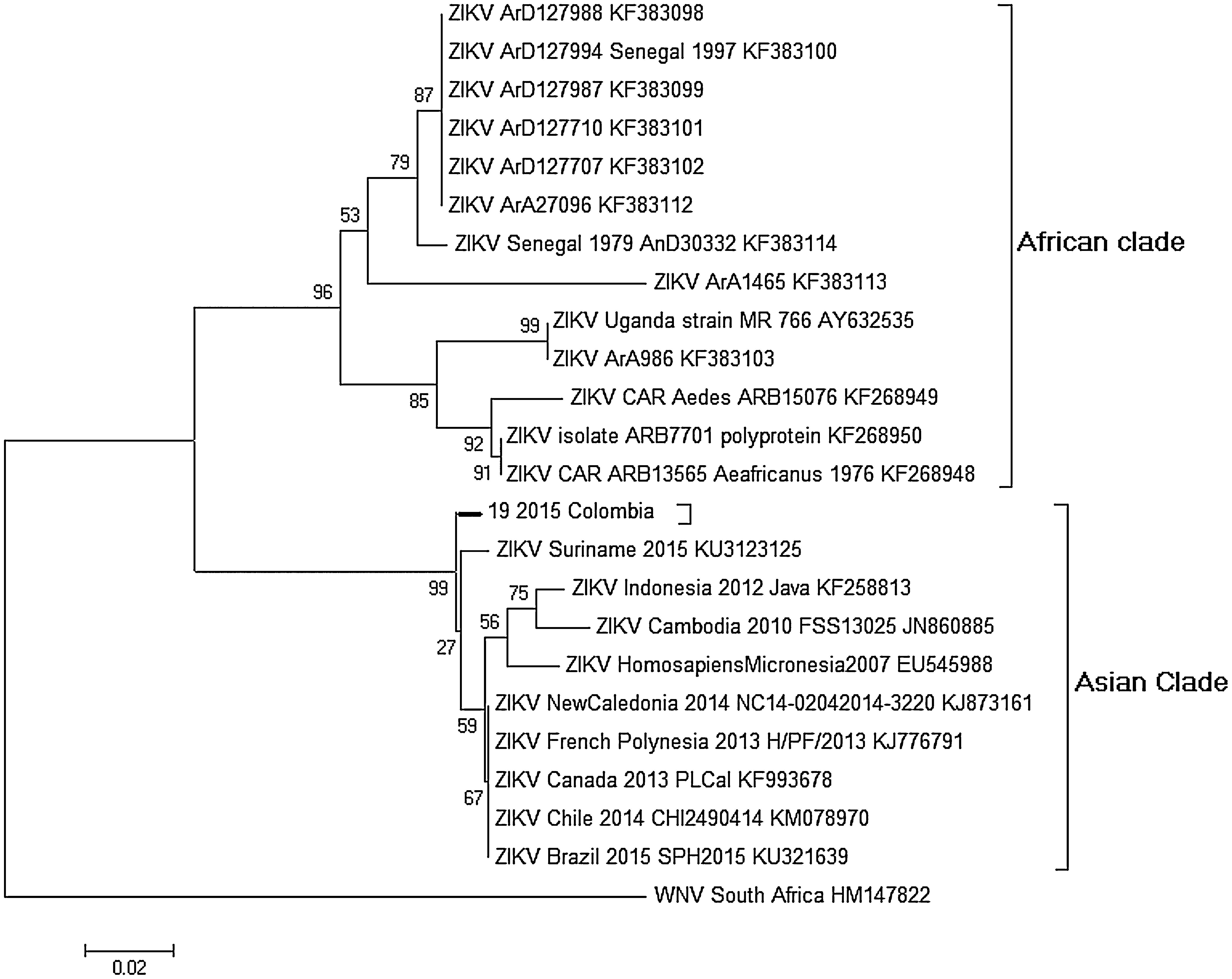
Having into consideration the epidemiological history, diagnosis of infection by Dengue (DENV), Chikungunya (CHKV) and Zika (ZIKV) viruses was requested, A 198bp amplicon was obtained from a sample of plasma taken 3 days after onset by using a RT-PCR specific for ZIKV (modified from Balm MN et al.).1 The product was sequenced and ZIKV was identified after BLAST analysis. A phylogenetic analysis with this fragment was carried out using the Mega 5 software, and the phylogenetic tree show that the sequence of ZIKV detected in the patient clusters within the Asian clade (Fig. 1). The sample was also used to detect DENV and CHIKV by PCR with negative results. A serum sample obtained the same day was analyzed by IFA against Zika virus (Arboviral Fever Mosaic IgG and IgM, Euroimmun, Germany). Positive and undetermined results for IgG and IgM, respectively, were obtained. An urine sample taken 14 days after the onset was also positive by PCR. It is remarkable that urine samples can be used for direct diagnostic and that virus can be detected for a longer period than in blood or serum samples.2 A case is confirmed when a positive result by PCR is obtained. This patient was confirmed by positive results in two different samples. The results of IFA are compatible with an acute Zika infection still without a clear IgM response in a patient with a previous exposition to another flavivirus such as DENV.
Phylogenetic analysis from partial NS5 gene of ZIKV. Neighbor-joining phylogenetic tree constructed by Mega 5 software using p-distance Method with 1000 bootstrap replicates. The tree was rooted with West Nile virus. The sequence obtained in this study is marked with the branch in bold.
Other laboratory tests were unremarkable: leukocytes 5500cells/μL (neutrophils 67%, lymphocytes 20%), hemoglobin 13.5g/dL, platelets 208,000cells/μL, ESR 12mm/h; urinalysis with traces of proteinuria; AST 29U/L, ALT 31U/L. Research of fecal parasites and stool showed no significant findings.
BackgroundZIKV is an arbo-virus (Flavivirus genus, Flaviviridae family). It was first identified in 1947 in the Zika forest (Uganda) from the blood of a Rhesus monkey. In 1948 it was isolated from a pool of Ae. africanus mosquitoes in the same forest.3 Thereafter, serological and entomological studies indicated human and animal ZIKV infections in the African continent. In 2007 an epidemic developed in Malaysia and Micronesia, including Yap Islands.4 Zika fever outbreak was reported in April 2015 in Brazil.5 Subsequently, autochthonous transmission has been identified in many countries and regions of America, Africa and Asia as well,6 including Colombia where autochthonous transmission of ZIKV was confirmed in September, 2015. Since then, more than 776 laboratory confirmed cases and more than 11,000 suspected cases have been reported (January, 19th, 2016) (Promed, Archive Number: 20160119.3948723).
ZIKV is transmitted by the bite of an infected Aedes mosquito. The vector can share DENV and CHKV,7 the co-infection has been described.8
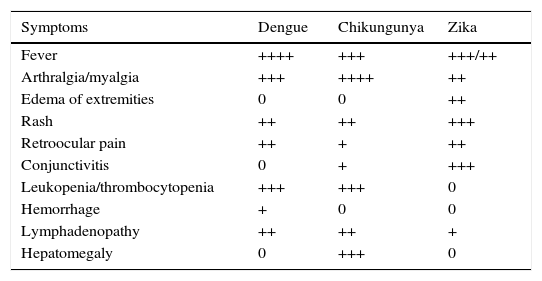
Signs and symptoms are similar to other arbovirus infections such as DENV or CHKV: mild fever (37.8–38.5°C), lasting usually four to seven days (Table 1), macular or papular rash, arthritis or arthralgia (usually in small joints) and no purulent conjunctivitis, myalgia, headache, asthenia and retro-orbital pain. Itching, abdominal pain, vomiting and diarrhea are less frequent.9 No hemorrhagic manifestations are associated with ZIKV infection; however, a case with hematospermia has been described.10 Overall, Zika fever it is a benign disease with few fatalities are reported.9 It seems that in rare cases, the infection can be complicated with Guillain-Barré syndrome.11 ZIKV infection in pregnant women could cause microcephaly as recently described in Brazil.11–14
Comparison of symptoms and signs between Dengue, Chikungunya and Zika.
| Symptoms | Dengue | Chikungunya | Zika |
|---|---|---|---|
| Fever | ++++ | +++ | +++/++ |
| Arthralgia/myalgia | +++ | ++++ | ++ |
| Edema of extremities | 0 | 0 | ++ |
| Rash | ++ | ++ | +++ |
| Retroocular pain | ++ | + | ++ |
| Conjunctivitis | 0 | + | +++ |
| Leukopenia/thrombocytopenia | +++ | +++ | 0 |
| Hemorrhage | + | 0 | 0 |
| Lymphadenopathy | ++ | ++ | + |
| Hepatomegaly | 0 | +++ | 0 |
Differential diagnosis includes other pathogens causing arthritis, including DENV and CHKV (in the regions where are present), rubella, parvovirus, measles, leptospirosis, malaria and rickettsiosis.
Diagnosis is based on clinical and epidemiological history of possible exposure to vectors. The definitive diagnosis is laboratory based, by detection of specific antibodies (IgG and IgM, and neutralizing antibodies) in serum, or, as in our case, by detection of viral genomes. Some commercial kits for PCR, IFA or ELISA are being developed but their use needs care since validation in many cases is still pending. The National Centre of Microbiology offers techniques to do the diagnostic of these infections if needed and to confirm positive cases.
No specific antiviral drugs for Zika fever are available. The treatment is symptomatic; rest, proper hydration, nonsteroidal anti-inflammatory drug and paracetamol, trying to avoid aspirin until dengue infection is completely ruled out in order to avoid bleeding.
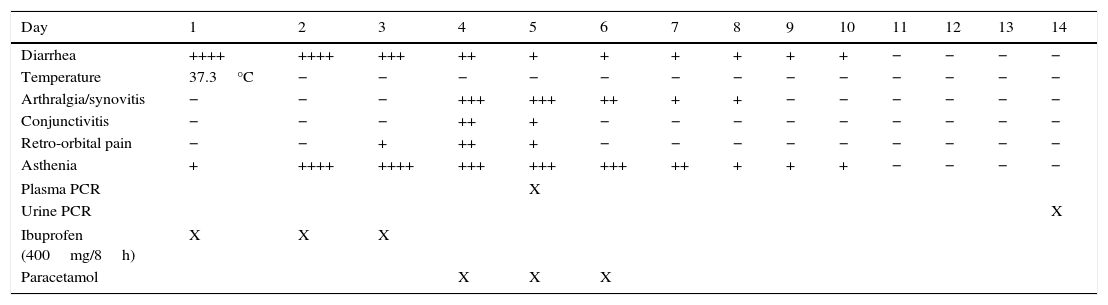
Evolution and conclusionsThe patient underwent treatment with ibuprofen for 72h and then paracetamol on demand for 72h. He evolved favorably with disappearance of fever and conjunctivitis within 48h; improvement of arthralgia and synovitis in five days. Diarrhea decreased to normalization in 10 days. He presented important asthenia during the first 6 days, with progressive normalization (Table 2).
Evolution of symptoms, signs, sampling and treatment.
| Day | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Diarrhea | ++++ | ++++ | +++ | ++ | + | + | + | + | + | + | − | − | − | − |
| Temperature | 37.3°C | − | − | − | − | − | − | − | − | − | − | − | − | − |
| Arthralgia/synovitis | − | − | − | +++ | +++ | ++ | + | + | − | − | − | − | − | − |
| Conjunctivitis | − | − | − | ++ | + | − | − | − | − | − | − | − | − | − |
| Retro-orbital pain | − | − | + | ++ | + | − | − | − | − | − | − | − | − | − |
| Asthenia | + | ++++ | ++++ | +++ | +++ | +++ | ++ | + | + | + | − | − | − | − |
| Plasma PCR | X | |||||||||||||
| Urine PCR | X | |||||||||||||
| Ibuprofen (400mg/8h) | X | X | X | |||||||||||
| Paracetamol | X | X | X | |||||||||||
In our environment ZIKV infection should be considered in any patient who presents with fever, rash, non-purulent conjunctivitis, edema of limbs and/or arthralgia and epidemiological history of visiting areas of transmission of this virus. The patient returned from Colombia to Valladolid, Castilla-León, a Spanish region located in the northwestern of Spain, where no Aedes albopictus has been described as far as we know.
Consequently there is no risk of autochthonous transmission by the bite of mosquitoes. The only concern could be associated to the possible sexual transmission. Surveillance programs in regions where the mosquito circulates should be applied in order to avoid the establishment of endemic cases.
Authors’ contributionsPBL, MDGG, AV, FO, MPSSF wrote the manuscript; MDGG, AV, FO, MPSSF performed laboratory investigations; PBL, JAM managed the patient and PBL collected diagnostic and clinical data.
Conflicts of interestNone declared.
Authors thank the staff from the Laboratories of “Arbovirus and Imported Viral Diseases” “Serology” National Centre of Microbiology of the Institute of Health Carlos III of the Ministry of Economy and Competitiveness Spain and Daniel de Luis for reviewing the manuscript.