The aim of this study was to determine the prevalence of Mycoplasma genitalium infection and the resistance to macrolides within a general population in Madrid in 2015.
MethodsWe collected 359 urine samples from a general population with symptoms of sexually transmitted infections (STIs). All samples underwent a real-time PCR. For the detection of macrolide resistance, a 283bp fragment of region V of the 23S rRNA gene of M. genitalium was amplified and sequenced.
ResultsWe found a prevalence of 3.34% of M. genitalium and a macrolide resistance rate of 20%. In males, the prevalence was 6.62% and in women 0.96%, being significantly higher in males.
ConclusionsThe prevalence obtained shows that it is a pathogen to consider in our environment. These findings stress the need for routine testing of M. genitalium infections and would seem to suggest the advisability of resistance testing.
El objetivo de este estudio fue determinar en 2015 en una población general de Madrid la prevalencia de infección por Mycoplasma genitalium (M. genitalium) y la resistencia a macrólidos.
MétodosSe recogieron 359 muestras de orina procedentes de una población general con síntomas de infección de transmisión sexual. A todas las muestras se les realizó una PCR a tiempo real. Para la detección de resistencias a macrólidos, se amplificó y secuenció un fragmento de 283 pb de la región v del gen 23S rRNA de M. genitalium.
ResultadosSe encontró una prevalencia de un 3,34% de M. genitalium y un 20% de resistencia a macrólidos. En varones la prevalencia fue del 6,62% y en mujeres del 0,96%, siendo significativamente superior en varones.
ConclusiónLa prevalencia obtenida muestra que es un patógeno a considerar en nuestro entorno. Estos hallazgos hacen hincapié en la necesidad de realizar pruebas de rutina de infección por M. genitalium y argumentan que es recomendable realizar pruebas de resistencia.
Mycoplasma genitalium is a fastidious organism found in the urogenital tract of humans now recognized as a common cause of nongonococcal urethritis in men. In addition, it is associated with increased risk for cervicitis, pelvic inflammatory disease, and spontaneous abortions in women.1–3
Routine diagnostic detection is based on nucleic acid amplification methods.
The recommended treatment for M. genitalium is a single dose of 1g azithromycin, but in certain environments this pathogen responds poorly, having declined the eradication rate over the years.4,5 This has been associated with the development of resistance to macrolides,6 predominantly based on single point mutations in the V-region of the 23S rRNA gene.6,7
There are still a limited number of studies related to the prevalence of M. genitalium in the world, that can widely differ depending on both the geographic location and the population tested; there are less studies related to resistance to azithromycin. The aim of this study was to determine the prevalence of M. genitalium infection and the resistance to macrolides in a symptomatic general population of two separate areas of the Community of Madrid, Spain.
Between May and September 2015, 359 urine samples of patients attending general inquiries or emergency departments with symptoms suggestive of sexually transmitted infections (STIs) were collected from two separate areas of the Community of Madrid: the Getafe area with a population of 210,133 inhabitants (3.29% of the population of Madrid), and the La Paz area with 500,445 inhabitants (7.83% of the population of Madrid). 151 were from men (42.1%) and 208 from women. 7.52% of patients were aged between 0 and 20 years, 66.29% between 21 and 40 years, 20.89% between 41 and 60 years, and 2.2% were over 60 years. The samples underwent a technique of real time PCR in the Cobas 4800 (Roche®) to detect Chlamydia trachomatis and Neisseria gonorrhoeae (Cobas 4800 CT/NG Test, Roche®) and M. genitalium (M. genitalium EC LightMix Kit, Roche®) as per manufacturers protocol.
For the detection of macrolide resistance, a 283bp fragment of region V of the 23S rRNA gene of M. genitalium were amplified and sequenced.7
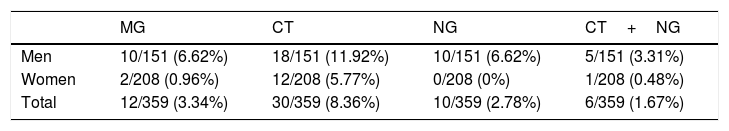
Of the 359 urine samples tested, 12 were found PCR-positive for M. genitalium, representing 3.34% of prevalence (95% CI, 1.48%–5.20%). In males, it was 6.62% (95% CI, 4.05%–9.19%) (10/151) and in women 0.96% (95% CI, 0%–1.97%) (2/208) (Table 1). Prevalence was significantly higher in males (p=0.003). The age range of infected patients was 21–40 (11/12) and 41–60 (1/12).
Prevalence of M. genitalium in the 359 samples studied.
| MG | CT | NG | CT+NG | |
|---|---|---|---|---|
| Men | 10/151 (6.62%) | 18/151 (11.92%) | 10/151 (6.62%) | 5/151 (3.31%) |
| Women | 2/208 (0.96%) | 12/208 (5.77%) | 0/208 (0%) | 1/208 (0.48%) |
| Total | 12/359 (3.34%) | 30/359 (8.36%) | 10/359 (2.78%) | 6/359 (1.67%) |
MG: Mycoplasma genitalium, CT: Chlamydia trachomatis, NG: Neisseria gonorrhoeae.
In the 359 samples studied, only C. trachomatis was detected in 30 (8.36%), only N. gonorrhoeae was detected in 10 (2.78%), and in 6 (1.67%) both agents were detected (Table 1).
Regarding the resistance results, we were able to determine it for 10/12 M. genitalium positive samples. Of these, 2 (20%) carried mutations that would render them resistant to macrolides: one of them had a mutation in the position A2058T and the other in A2059G.
To our knowledge there are no publications on the prevalence of M. genitalium in Spain, our study aimed to assess it in a general population of Madrid. The prevalence obtained, 3.34%, shows that it is a pathogen to consider in our environment in patients with symptoms suggestive of STIs. Infection with M. genitalium is generally assumed to result in more frequently clinical signs in males and this is supported by our finding that the prevalence was significantly higher in men than in women. The prevalence is in the range of other agents of STIs commonly searched for. However, testing for M. genitalium is not common, and in our opinion routine screening for this pathogen is advisable.
The studies carried out to date in other countries show different data. In the US, a national study in healthy young people, 1714 men and 1218 women, obtained a prevalence of 1%.8 In Sweden, in a heterogeneous population of 5519 women attending a gynecological clinic M. genitalium was found in 2.1%.9 In the UK, in 216 men with urethritis and without urethritis attending a genitourinary medicine clinic, the prevalence was 10.2%, higher in patients with urethritis.10 However, in France, in a study of 301 patients younger than 31 years who went to the emergency room with symptoms, a prevalence of 0.3%11 was found. In Denmark, 28,958 patients attending specialists and general hospitals were studied between 2006 and 2010, and the prevalence obtained, according to the year, was 2.4%–3.8% in women and 7.9%–10.3% in men.12 In Spain, there is no publication that discusses the prevalence of this organism, which makes this study of prevalence, co-infection, and macrolide resistance innovative. The findings in our study are similar to those obtained in the Denmark study12 that was also performed in the general population, but differs from other studies carried out in specific and selected population.
Data of macrolide resistance in other countries are also diverse and range from 14.2% to 43%.7,12,13 The data obtained in our study indicate an average rate of resistance compared to other studies.
After the rate of resistance to macrolides obtained, we thought that detection of macrolide resistance is required to guide the clinician in the choice of antibiotic and limiting the selection and propagation of resistances,6 and thus avoiding therapeutic failures. As an alternative, we propose a test of cure (test of care) on day 14 or later, due to the low probability of detecting nonviable DNA and its association if it is positive with resistance to azithromycin.5,14
Conflict of interestNone.