Listeria monocytogenes infection is a severe disease affecting mainly aged people and patients with immune depression. The incidence of listeriosis seems to be increasing. In the present study cases of listeriosis from two hospitals are analyzed with the aims of studying changes in its incidence, clinical forms of presentation and possible factors associated with mortality.
MethodsRetrospective multicentric study of patients with culture-proven listeriosis in two university hospitals in Madrid between 1977 and 2021. Epidemiological and clinical variables, as well as factors for immune depression, complementary studies and treatments were registered. Factors associated with mortality were analyzed.
ResultsA total of 194 cases of listeriosis were analyzed. The incidence of listeriosis among in-patients increased through the study period, with a significant drop in the number of cases in 2020. The most common clinical presentations were isolated bacteriemia (37.1%) and central nervous system involvement (CNS) (36.6%). Symptoms of gastroenteritis occurred in 21% of cases. Other focal infections were present in 16.5% of patients, the most frequent were spontaneous bacterial peritonitis (8.2%), cholecystitis (2.1%), respiratory infection (1.5%) and vascular prothesis infection (1.5%). In-hospital mortality was 24.7%. Independent factors associated with mortality at admission were age (Odds Ratio [OR] 1.027, 95% confidence interval [IC95%] 1.003–1.056) and a diagnosis of a solid tumor (OR 3.525, IC95% 1.652–7.524).
ConclusionsThis study confirms an increasing incidence of listeriosis in our millieu. The most common clinical presentations were isolated bacteriemia and central nervous system involvement. In-hospital mortality was associated with age and the diagnosis of a solid tumor.
La infección por Listeria monocytogenes es una enfermedad grave que afecta mayoritariamente a personas de edad avanzada e inmunodeprimidos y cuya incidencia está aumentando. En este estudio se analizan los casos de listeriosis en dos hospitales con el fin de estudiar cambios en su incidencia, formas de presentación clínica y posibles factores asociados a mortalidad.
Material y métodosEstudio retrospectivo multicéntrico de pacientes con listeriosis diagnosticada por aislamiento microbiológico entre 1977 y 2021 en dos hospitales universitarios de Madrid. Se recogen variables epidemiológicas, clínicas, estado de inmunodepresión, pruebas complementarias y tratamiento. Se analizan factores asociados a mortalidad.
ResultadosSe analizaron 194 casos de listeriosis. La incidencia de listeriosis por ingresos aumentó a lo largo del estudio, con una importante caída del número de casos en 2020. La bacteriemia aislada (37,1%) y la afectación del sistema nervioso central (SNC) (36,6%) fueron las presentaciones más frecuentes. El 21% de los casos tuvo síntomas de gastroenteritis. El 16,5% presentaron otras infecciones focales, siendo las más frecuentes peritonitis bacteriana espontánea (8,2%), colecistitis (2,1%), infección respiratoria (1,5%) e infección de prótesis vascular (1,5%). La mortalidad intrahospitalaria fue del 24,7%. Fueron factores independientes asociados a mortalidad al ingreso la edad (Odds Ratio [OR] 1,027, intervalo de confianza 95% [IC95%]1,003–1,056) y la presencia de tumor sólido (OR 3,525, IC95%1,652–7,524).
ConclusionesEn este estudio se constata de la incidencia de listeriosis en nuestro medio. Las presentaciones más frecuentes fueron la bacteriemia aislada y la afectación del SNC. La mortalidad intrahospitalaria se asoció a la edad y al diagnóstico de tumor sólido.
Listeria monocytogenes is an intracellular Gram-positive rod-shaped bacterium, whose main transmission mechanism is through the ingestion of contaminated food1,2. Listeriosis can manifest as self-limiting acute gastroenteritis. Infection during pregnancy causes significant foetal morbidity and mortality2. Invasive forms of disease not associated with pregnancy include bacteraemia, central nervous system (CNS) involvement, or neurolisteriosis, and other localised infections such as peritonitis, endocarditis, liver abscess, cholecystitis, pleuropulmonary infection and joint infection. Most invasive forms of listeriosis affect older adult patients, or those with one or more factors associated with immunosuppression2–5. The incidence of listeriosis has been increasing over the last twenty or thirty years6–8, and we must therefore be more aware of the possibility of this disease when diagnosing and treating patients, particularly those with predisposing factors. In Spain, epidemiological studies on listeriosis have been carried out in the country as a whole and in some provinces7,9–11.
This study analysed all culture-confirmed cases of listeriosis in two university hospitals in Madrid. The aims of the study were to determine the incidence of listeriosis over the last forty years and the frequency of the different clinical presentations, and to study factors associated with in-hospital death in these patients.
Material and methodsThis was a non-interventional multicentre retrospective observational study of patients with a microbiological diagnosis of listeriosis.
PatientsPatients treated at two university hospitals in Madrid, Spain were selected by searching the computerised records of hospital discharge reports with the term “Listeria” and the computerised records of the microbiology departments of patients with positive cultures for L. monocytogenes. Patients diagnosed with listeria since 1993 were identified at the first hospital and since 1977 at the second. The microbiology records included positive cultures since 2011 at the first hospital, and since 1993 at the second.
These are two tertiary university hospitals, both of which perform haematopoietic stem cell transplants, and hospital 2 performs kidney and liver transplants. Neither of them provide obstetrics care.
Inclusion criteriaPatients with a microbiological diagnosis of L. monocytogenes infection by culture of a normally sterile sample at one of the two hospitals (invasive listeriosis). Cases of pregnancy-associated listeriosis (isolation of L. monocytogenes from pregnant women, foetuses or neonates) and cases demonstrated only by polymerase chain reaction (PCR) were not included.
Data collectionWe assessed the hospital discharge reports and medical records of the patients who met the inclusion criteria. Where necessary, we consulted the Horus program of Madrid Region's Health Department in order to obtain clinical and outcome data.
We collected the following groups of variables:
Epidemiological variables: gender; age at diagnosis; year of diagnosis of Listeria infection; and hospital at which diagnosed.
Previous medical history: high blood pressure; heart disease; lung disease; immunosuppression factors (diabetes mellitus, immunosuppressive therapy including chemotherapy, solid tumour disease without chemotherapy, haematological-oncological disease; liver cirrhosis; stage 3 or higher chronic kidney disease; human immunodeficiency virus infection (HIV) and CD4 lymphocyte count at diagnosis; alcoholism; and solid organ transplant).
Variables related to L. monocytogenes infection: type of sample in which L. monocytogenes was isolated; site of the primary disease by L. monocytogenes; treatment received and its duration; and in-hospital death.
DefinitionsIsolated bacteraemia: positive blood cultures with no sign of localised infection.
Meningitis: patients with more than five cells in the cerebrospinal fluid (CSF), clinical manifestations consistent with meningeal syndrome, and isolation of L. monocytogenes in CSF or blood culture.
Rhombencephalitis: patients with signs or symptoms of involvement of the brainstem or cerebellum and isolation of L. monocytogenes in CSF or blood culture. Cases with isolated ataxia explainable by aminoglycoside ototoxicity were excluded.
Brain abscess: brain lesion with uptake or contrast-enhancing ring on imaging tests and isolation of L. monocytogenes in CSF, abscess material or blood culture.
Other localised infections: localised infection demonstrated by investigations and culture of L. monocytogenes in an appropriate sample or blood culture.
ImmunosuppressionA patient's degree of immunosuppression was classified according to the following criteria:
Severe: HIV infection with CD4 lymphocytes below 200/mm3; treatment with immunosuppressants or chemotherapy; haematological-oncological disease; or solid organ transplantation. Treatment with corticosteroids is considered immunosuppressive with a dose equivalent to 20mg/day or higher of prednisone for more than 30 days.
Mild: diabetes mellitus; solid tumour disease; liver cirrhosis; chronic kidney disease stage 3 or higher; alcoholism (average consumption of more than five or six units per day or 50g of pure ethanol); HIV infection with CD4 lymphocytes greater than 200/mm3.
Not immunosuppressed: does not meet the criteria to be classified in any of the above.
Statistical analysisThe categorical variables are presented as absolute and relative frequencies. Quantitative variables are presented as mean and standard deviation.
Student's t test was used to compare continuous variables. For the contrast of hypotheses between two qualitative variables, Pearson's χ2 test was used, or Fisher's exact test where necessary.
We calculated the annual incidence per 10,000 admissions over the years of the study in the series as a whole and for the two hospitals separately.
We used a Poisson regression model to assess the temporal trend in the incidence of listeriosis over the study years, calculating the incidence ratio (IR) for the whole series and for each hospital separately.
To contrast the effect of the time period in the proportion of different qualitative variables (immunosuppressed patients, clinical presentations, mortality), we carried out a Mantel-Haenszel test for linear trend. The periods analysed were 1977–1999, 2000–2010 and 2011–2021.
Statistical significance was established at P<.05.
For the evaluation of prognostic factors, we used a binary logistic regression model. Variables present at admission with significance in the univariate analysis and other clinically relevant variables (age, gender, immunosuppression) were included in the maximum model. To assess the discrimination of the model, we calculated the area under the receiver operating characteristic (ROC) curve.
Statistical analysis was performed with the software program SPSS Statistics V. 27 (IBM Corp., Armonk, NY USA).
Ethics Committee approvalThe study was approved by the participating hospitals' independent ethics committees.
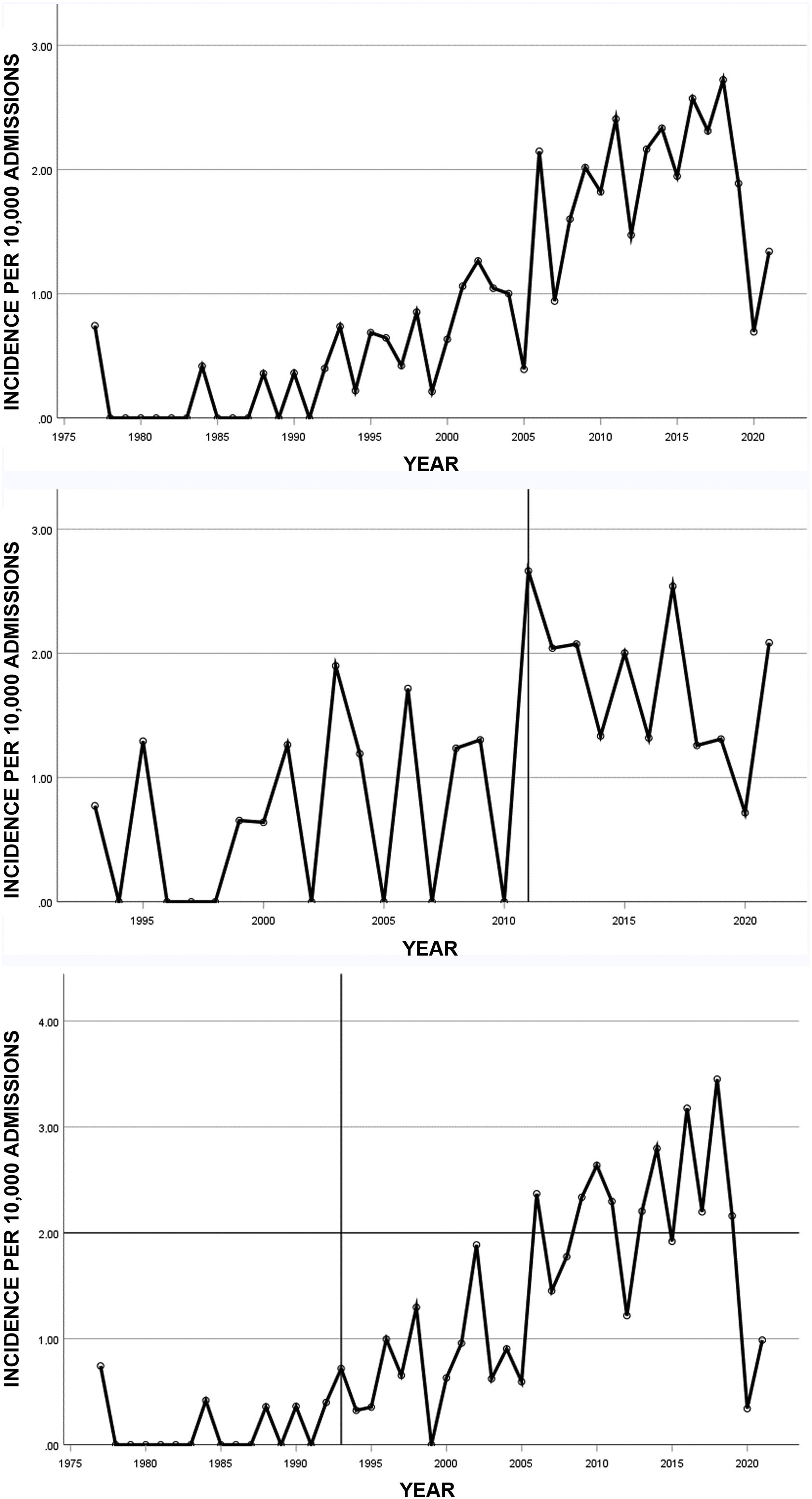
ResultsFrequency of listeriosisOver the study period, 194 patients diagnosed with listeriosis were identified, 51 at the first hospital and 143 at the second. The incidence of listeriosis per 10,000 admissions over the study period is shown in Fig. 1. We found a significant increase in the incidence in terms of admissions over the course of the study, both for the series as a whole (IR 1.07, 95% CI 1.05–1.08, P<.001), and for each of the hospitals separately (hospital 1: IR 1.06, 95% CI 1.02–1.09, P=.003; hospital 2; IR 1.07, 95% CI 1.05–1.08, P<.001). In 2020, there was a large drop in cases, coinciding with lockdown due to the COVID-19 pandemic.
A: Annual incidence of listeriosis per 10,000 admissions from 1977 to 2021 in two hospitals in Madrid, Spain. B: Annual incidence at hospital 1. C: Annual incidence at hospital 2. The vertical lines mark the year from which computerised microbiology records were available at each hospital.
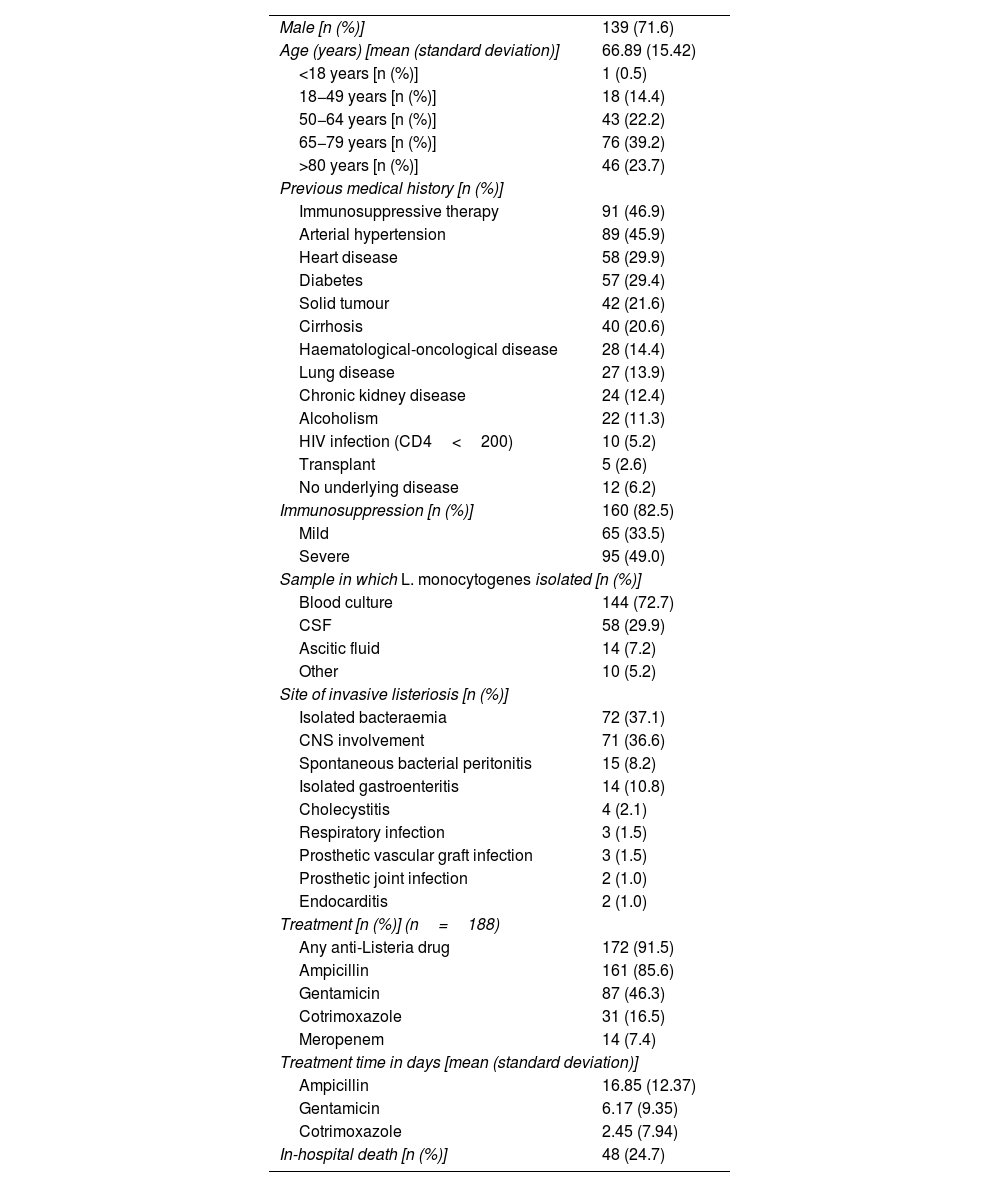
Patient characteristics are shown in Table 1. There was a predominance of males (71.6%) and the mean age was 66.9 years (15.4), with 83.5% over the age of 50.
Clinical data for the 194 patients with listeriosis.
| Male [n (%)] | 139 (71.6) |
| Age (years) [mean (standard deviation)] | 66.89 (15.42) |
| <18 years [n (%)] | 1 (0.5) |
| 18−49 years [n (%)] | 18 (14.4) |
| 50−64 years [n (%)] | 43 (22.2) |
| 65−79 years [n (%)] | 76 (39.2) |
| >80 years [n (%)] | 46 (23.7) |
| Previous medical history [n (%)] | |
| Immunosuppressive therapy | 91 (46.9) |
| Arterial hypertension | 89 (45.9) |
| Heart disease | 58 (29.9) |
| Diabetes | 57 (29.4) |
| Solid tumour | 42 (21.6) |
| Cirrhosis | 40 (20.6) |
| Haematological-oncological disease | 28 (14.4) |
| Lung disease | 27 (13.9) |
| Chronic kidney disease | 24 (12.4) |
| Alcoholism | 22 (11.3) |
| HIV infection (CD4<200) | 10 (5.2) |
| Transplant | 5 (2.6) |
| No underlying disease | 12 (6.2) |
| Immunosuppression [n (%)] | 160 (82.5) |
| Mild | 65 (33.5) |
| Severe | 95 (49.0) |
| Sample in which L. monocytogenes isolated [n (%)] | |
| Blood culture | 144 (72.7) |
| CSF | 58 (29.9) |
| Ascitic fluid | 14 (7.2) |
| Other | 10 (5.2) |
| Site of invasive listeriosis [n (%)] | |
| Isolated bacteraemia | 72 (37.1) |
| CNS involvement | 71 (36.6) |
| Spontaneous bacterial peritonitis | 15 (8.2) |
| Isolated gastroenteritis | 14 (10.8) |
| Cholecystitis | 4 (2.1) |
| Respiratory infection | 3 (1.5) |
| Prosthetic vascular graft infection | 3 (1.5) |
| Prosthetic joint infection | 2 (1.0) |
| Endocarditis | 2 (1.0) |
| Treatment [n (%)] (n=188) | |
| Any anti-Listeria drug | 172 (91.5) |
| Ampicillin | 161 (85.6) |
| Gentamicin | 87 (46.3) |
| Cotrimoxazole | 31 (16.5) |
| Meropenem | 14 (7.4) |
| Treatment time in days [mean (standard deviation)] | |
| Ampicillin | 16.85 (12.37) |
| Gentamicin | 6.17 (9.35) |
| Cotrimoxazole | 2.45 (7.94) |
| In-hospital death [n (%)] | 48 (24.7) |
CNS: central nervous system; CSF: cerebrospinal fluid; HIV: human immunodeficiency virus.
A total of 160 patients (82.5%) had some degree of immunosuppression, which was defined as severe in 95 patients (49%) and mild in 65 patients (33.5%). Thirty-seven patients were on treatment with corticosteroids. The mean age was higher in patients with no immunosuppression than in immunosuppressed patients (73.2±18.3 vs 65.2±14.4, P=.009). The percentage of immunosuppressed patients did not increase over the study period (81.8% in 1977–1999, 80.5% in 2000–2009 and 81.6% in 2010–2021, P=.62).
Blood cultures were documented for 180 patients (92.8%). L. monocytogenes was isolated in the blood cultures of 144 patients (74.2%), of whom 72 (37.1%) had clinical signs of isolated bacteraemia. There were 71 patients (36.6%) with CNS involvement: 69 (97.2%) with meningitis; seven (9.9%) with brain abscess; and six (8.5%) with rhombencephalitis. Brain scans were performed on 66 patients with neurolisteriosis (93%) (62 computed tomography, 40 magnetic resonance imaging). The mean age was lower in patients with CNS involvement than in the rest (62.8±16.1 vs 69.3±14.6, P=.005). There were no differences between patients with or without CNS involvement in terms of immunosuppression. Twenty-one patients (10.8%) had gastroenteritis: all of them had positive blood cultures (14 cases, 7.2%) or signs or symptoms of other culture-confirmed localised infections (seven cases associated with meningitis). In total, 32 patients (16.5%) had other localised infections. There were 15 cases of spontaneous bacterial peritonitis (SBP) associated with cirrhosis (7.7%), 14 of whom were diagnosed with isolation in ascitic fluid, the rest with positive blood culture. Other localised infections were less common: cholecystitis, four cases; respiratory infection and prosthetic vascular graft infection, three each; endocarditis and prosthetic joint infection, two each; and one each for myopericarditis, perianal abscess, abdominal abscess, liver abscess and surgical wound infection. The frequency of some clinical forms changed over the course of the study: there was an increase in the frequency of both isolated bacteraemia (22.7% in 1977–1999, 31.9% in 2000–2010 and 43.7% in 2011−2021, P=.023) and gastroenteritis (0% in 1977–1999, 8.7% in 2000–2010 and 14.6% in 2011−2021, P=.036), while there was a decrease in the frequency of nervous system involvement (59.1% in 1977–1999, 44.9% in 2000–2010 and 26.2% in 2011−2021, P=.001) and peritonitis (13.6% in 1977–1999, 11.6% in 2000–2010 and 3.9% in 2011−2021, P=.04). There were no significant differences in the frequency of the different clinical forms of listeriosis in patients with or without immunosuppression. The frequency of the clinical forms of presentation was similar at the two hospitals, with the exception of a higher frequency at hospital 1 of rhombencephalitis (4 out of 51 vs 2 out of 143, P=.042) and gastroenteritis (10 out of 51 vs 11 out of 143, P=.007).
The treatment in six patients was unknown, and eight patients were not treated with antibiotics, three by medical decision as they were terminally ill from their underlying disease. In total, 172 patients (91.5%) received at least one antibiotic with activity against L. monocytogenes: 86.5% ampicillin (46.3% combined with gentamicin and 16.5% with cotrimoxazole); 7.4% meropenem; 4.3% levofloxacin; 3.2% linezolid; and 2.1% others.
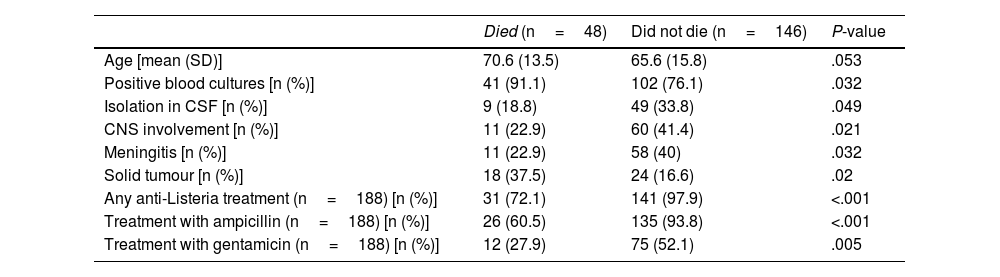
Mortality ratesForty-eight patients (24.7%) died while in hospital. There were no significant changes in the mortality rate over the course of the study period (36.4% in 1977–1999, 27.9% in 2000–2010 and 20.4% in 2011−2021, P=.084) and the rates for the two hospitals were similar (10 out of 51 [19.6%] vs 38 out of 142 [26.8%], P=.311).
To analyse variables associated with patient death, all available variables were included in the univariate analysis. The variables associated with mortality in the total number of patients in the univariate analysis are shown in Table 2. The mortality rate was significantly lower in patients who received any treatment with an anti-Listeria effect, particularly ampicillin and gentamicin. However, in patients treated with ampicillin, combing the treatment with gentamicin made no difference to the mortality rate (P=.418).
Variables associated with in-hospital death in the univariate analysis in patients with listeriosis.
| Died (n=48) | Did not die (n=146) | P-value | |
|---|---|---|---|
| Age [mean (SD)] | 70.6 (13.5) | 65.6 (15.8) | .053 |
| Positive blood cultures [n (%)] | 41 (91.1) | 102 (76.1) | .032 |
| Isolation in CSF [n (%)] | 9 (18.8) | 49 (33.8) | .049 |
| CNS involvement [n (%)] | 11 (22.9) | 60 (41.4) | .021 |
| Meningitis [n (%)] | 11 (22.9) | 58 (40) | .032 |
| Solid tumour [n (%)] | 18 (37.5) | 24 (16.6) | .02 |
| Any anti-Listeria treatment (n=188) [n (%)] | 31 (72.1) | 141 (97.9) | <.001 |
| Treatment with ampicillin (n=188) [n (%)] | 26 (60.5) | 135 (93.8) | <.001 |
| Treatment with gentamicin (n=188) [n (%)] | 12 (27.9) | 75 (52.1) | .005 |
CNS: central nervous system; SD: standard deviation.
In the multivariate analysis for factors present at admission associated with patient death, independent factors were age (OR 1.027, 95% CI 1.003–1.056) and having a solid tumour (OR 3.525, 95% CI 1.652–7.524). The area under the ROC curve was 0.684.
DiscussionIn this study, we analysed a large case series of non-pregnancy associated listeriosis in adults using strict criteria for the cases included. The annual incidence of listeriosis per 10,000 hospitalised patients showed an increasing trend throughout the study period in the two participating hospitals. That trend had already been demonstrated in a national study here in Spain, by analysing hospital admissions with the basic minimum data set7, and in various European and non-European countries6,8. Although the causes of this phenomenon are still not entirely clear, it is thought that the ageing of the population, an increase in the number of people with risk factors for L. monocytogenes infection, a greater consumption of ready-made meals and the effects of the changes over these last forty years in the way food is processed, distributed and prepared may all have had an influence6,7. Notably, although cases of isolated bacteraemia increased over the course of the study, cases of CNS involvement decreased. A higher rate of taking blood cultures in more recent times could have contributed to the increase in cases. However, at both hospitals, taking blood cultures when assessing febrile symptoms was routine throughout the study period and the percentage of positive blood cultures did not vary over that time.
This series confirms a sharp drop in the number of cases in 2020, coinciding with lockdown due to the COVID-19 pandemic, with this already having been reported in the USA12. The roll-out of the health measures applied to prevent the transmission of SARS-CoV-2, the closure of restaurants and a lower rate of detection of Listeria infection due to health service disruptions may also have contributed to this decrease12.
In this study, the vast majority of patients with listeriosis were male (72%). This finding had already been previously reported by other authors who, unlike our study, did include cases of pregnancy-associated listeriosis2,4,7,9. The mechanism for increased susceptibility to L. monocytogenes infection among males remains unknown. The mean age is high (67) and similar to that in other series2,4,8,10,13,14, explained by the increased risk of listeriosis with age.
We confirmed the common association of non-pregnancy associated listeriosis with immunosuppression factors, with our rate (83%) in the highest range of the published studies2,4,7,8,10,11,15, where rates range from 48.8% in a California study15 to 90.7% in the MONALISA study2. Almost half of these patients have severe immunosuppression (HIV infection with CD4 counts less than 200/mm3, transplant recipients, immunosuppressive therapy, chemotherapy, oncological-haematological disease), while the rest have one or more other associated factors (diabetes, alcoholism, liver disease and kidney disease). However, comparing the numbers of patients with immunosuppression between different studies is difficult due to the differences in the conditions included as immunosuppression. In the California study15, the criteria for immunosuppression are similar to our criteria for severe immunosuppression and do not include diabetes, kidney or liver disease, or alcoholism, while in the MONALISA study2 they include these diseases and patients aged over 70. In this context, we believe that our criteria for distinguishing patients with severe and mild immunosuppression is useful.
The most common forms of presentation of listeriosis are isolated bacteraemia and neurolisteriosis, with each accounting for more than a third of the cases; other localised infections are less common. We stress that L. monocytogenes should be included in the aetiological differential diagnosis of SBP and that listeria is capable of infecting prosthetic vascular grafts or prosthetic joints and causing other intra-abdominal infections. Compared with the MONALISA study, a prospective multicentre study in France that included 818 patients, in our series the relative frequency of bacteraemia was lower and that of localised infections higher, because in the MONALISA study infections were only considered to be localised if L. monocytogenes was isolated in material from the site itself, while other localised infections with positive blood cultures were classified as bacteraemia2. Other studies have also reported a higher rate of bacteraemia and a lower rate of localised infections4,10,11, but an Israeli study using criteria similar to ours showed rates in line with ours14. It is not uncommon for patients with listeriosis to have gastroenteritis in addition to bacteraemia or other localised infections. In our study, 10.8% had gastroenteritis, a slightly lower rate than in other series2,5, which reported around 19% of the cases overall.
In our study, 7.7% of patients with non-pregnancy associated invasive listeriosis had SBP, a figure higher than the 1.6%–2.8% of cases reported in other studies2,11,13. L. monocytogenes is a very rare cause of SBP, with no cases mentioned in large SBP series, despite the recent increase in SBP by Gram-positive organisms16,17. Only one centre in Egypt reported a high incidence (24.4%) of listeria as a cause of SBP18.
The in-hospital mortality rate in this study was 24.7%, within the range of previous reports8,10,11. In the MONALISA study, the three-month mortality rate was higher (39.6%)2. Restricting the assessment of mortality rates to in-hospital death undoubtedly contributed to the lower rates in our study. We believe that the in-hospital mortality rate may be a better reflection of the mortality rate attributable to L. monocytogenes, as many cancer patients died not long after being discharged, having recovered from the listeriosis. Some 16% of patients who survive listeriosis die within the first year10.
In the MONALISA study, numerous independent factors were associated with the three-month mortality rate in listeriosis in general, including age, factors related to the severity of the systemic symptoms, and having active cancer2. Treatment with anti-Listeria drugs is a protective factor. In our study, older age and having a solid tumour were confirmed as independent factors prior to admission for in-hospital mortality in listeriosis, with an acceptable power of discrimination (area under the ROC curve 0.684). Other studies have replicated these findings and have found other factors, such as alcoholism, corticosteroid therapy, lung disease, kidney disease and cardiovascular disease8,10,12,13.
Our study has the limitations inherent to a retrospective study, including the problems in obtaining data and the variability in the diagnostic and therapeutic management of the patients. The case search strategy does not guarantee that all cases of listeriosis in the participating hospitals during the study period were found. In addition, the search strategy differed between the two hospitals, as in one, the Microbiology Department did not start keeping a record of positive cultures until 2011. We could therefore have underestimated the incidence in the early years of the study. Nevertheless, the strengths of this study are the large number of cases of listeriosis studied, the strict inclusion criteria and the large number of variables analysed.
In conclusion, this study shows a progressive increase in the incidence of listeriosis over the last forty years in our region, with a drop in the number of cases in 2020, coinciding with the COVID-19 pandemic. As in other studies, the majority of patients with non-pregnancy associated listeriosis are male, over the age of 50 and with some immunosuppressive factor. The most common clinical presentations of listeriosis were isolated bacteraemia and CNS infection, with each accounting for more than a third of the cases, followed by SBP associated with cirrhosis and gastroenteritis. A quarter of the patients with listeriosis died while in hospital. Independent factors associated with listeriosis patients dying in hospital were age and having a solid tumour.
FundingNo funding was received for this study.
Conflicts of interestThe authors declare that they have no conflicts of interest.