The incidence of anal cancer has increased in frequency in these recent years, mainly in risk groups such as men who have sex with men (MSM), HIV-infected patients, immunocompromised men and women, and patients with a history of cervical cancer.1 Much data have been published to conclude that anal cancer is continuously increasing in HIV-positive MSM despite the use of highly active antiretroviral therapy (HAART) probably because of the longer life expectancy.2 Infection with high risk genotypes of human papillomavirus (HR-HPV) is a major risk factor for development of anal cancer.3 In men, 80-85% of anal cancers worldwide are associated with HPV infection.4 HR-HPV include 12 genotypes (16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59) and probably HR-HPV include 6 other genotypes (26, 53, 66, 68, 73, 82).5 Screening of anal cancer is based on collecting cells for anal cytology followed by a colposcopic examination of the anus and distal rectum (high-resolution anoscopy) for those patients with abnormal cytological results. Early diagnosis and treatment of precancerous anal lesions should decrease the incidence of anal cancer in the same way as the incidence of cervical cancer has been reduced through screening to diagnose and treat severe cervical lesions.
The aim of this study was to determine the prevalence and distribution of HR-HPV in anal samples from MSM with abnormal cytology, as well as the frequency of cytological lesions and its association with the human immunodeficiency virus (HIV) infection.
A total of 100 MSM who attended the Sexual Transmitted Disease Unit of the Ramón y Cajal Hospital were studied from June 2009 to October 2010. Anal samples were collected with cervical brushes (Cervix-Brush®) and stored in PreservCyt® medium. Cytological analyses were performed using the Bethesda classification6 and HPV genotypes were detected by PCR (Linear Array®, Roche Diagnostics, Mannheim, Germany). Statistical analysis were performed with SAS (S.A.S. Institute Inc., Cary, NC).
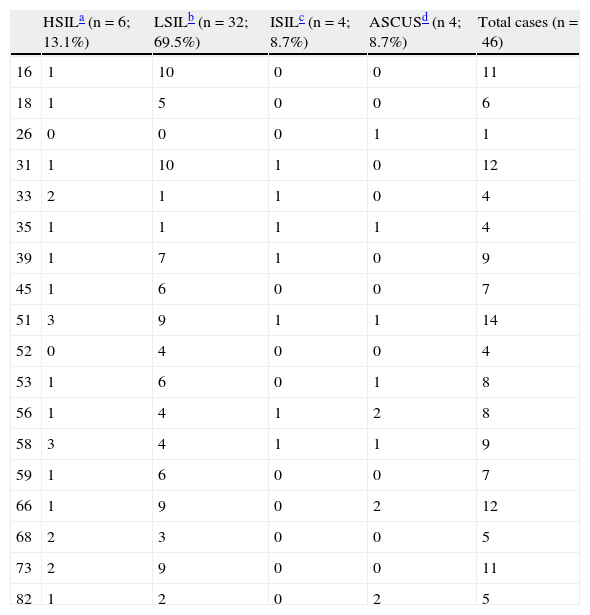
The mean age of the patients was 35.3 years (range: 17-65 years), 47 (47%) of them were HIV positive. Cytological lesions were only detected in 46 anal samples from 43 patients, and were as follows: 8.7% Atypical Squamous Cell Unknown Significance (ASCUS), 69.5% Low Squamous Intraepithelial Lesion (LSIL), 8.7% Indeterminate Squamous Intraepithelial Lesion (ISIL) and 13.1% High-Grade Squamous Intraepithelial Lesion (HSIL). HIV positive patients had 74% of LSIL and 11% of HSIL versus 63% and 15.7%, respectively in the non HIV-infected ones (P>.5). Negative results for HPV were observed in 4 samples with cytological lesions (3 LSIL and 1 ASCUS). Of the HPV positive samples, 93% showed a mixed co-infection (from 2 to 11 genotypes), the coexistence of three or more different genotypes in the same sample (19%) being most frequently observed. In the overall analysis (Table 1), HPV-51 was the most frequent genotype detected (30%), followed by HPV-31 and HPV-66 (both 26%), and finally genotypes HPV-16 and 18 were found in 24% and 13%, respectively. HR-HPV was detected in 80.4% of anal samples (68.4% in HIV negative versus 88.8% in HIV positive, P=0.08). The most frequent HR-HPV in HIV negative and HIV positive patients was HPV-31 and HPV-51 respectively. Both HR-HPV-16 and 31 were the most prevalent genotypes in patients with LSIL, whereas in the group of HSIL these were represented by HPV-51 and HPV-58.
Distribution of HR-HPV types by cytological diagnosis.*
| HSILa (n=6; 13.1%) | LSILb (n=32; 69.5%) | ISILc (n=4; 8.7%) | ASCUSd (n 4; 8.7%) | Total cases (n=46) | |
| 16 | 1 | 10 | 0 | 0 | 11 |
| 18 | 1 | 5 | 0 | 0 | 6 |
| 26 | 0 | 0 | 0 | 1 | 1 |
| 31 | 1 | 10 | 1 | 0 | 12 |
| 33 | 2 | 1 | 1 | 0 | 4 |
| 35 | 1 | 1 | 1 | 1 | 4 |
| 39 | 1 | 7 | 1 | 0 | 9 |
| 45 | 1 | 6 | 0 | 0 | 7 |
| 51 | 3 | 9 | 1 | 1 | 14 |
| 52 | 0 | 4 | 0 | 0 | 4 |
| 53 | 1 | 6 | 0 | 1 | 8 |
| 56 | 1 | 4 | 1 | 2 | 8 |
| 58 | 3 | 4 | 1 | 1 | 9 |
| 59 | 1 | 6 | 0 | 0 | 7 |
| 66 | 1 | 9 | 0 | 2 | 12 |
| 68 | 2 | 3 | 0 | 0 | 5 |
| 73 | 2 | 9 | 0 | 0 | 11 |
| 82 | 1 | 2 | 0 | 2 | 5 |
We conclude, that in our study the most prevalent HPV genotype in anal samples of MSM men that presented an abnormal cytology was HPV-51 (almost all in samples from HIV positive patients), followed by HPV-31 and HPV-66. Interestingly, genotypes 16 and 18 were not the most prevalent in anal samples as opposed to cervical samples in our country7 and several areas of the world.4 None of the patients included in the study had been vaccinated. Infections with multiple genotypes are common. The mean number of genotypes detected in each anal sample in our study is similar to other published studies using the same assay.8 Only in 7% of the patients was there a unique genotype present. There is no difference in the frequency of LSIL, HSIL and HR-HPV between HIV negative and positive patients. Thus, we could not demonstrate that HIV infection is associated with the presence of HSIL as stated by other authors.9 This can be explained because the immunological status and HAART play a role in the development of HSIL lesions in HIV positive patients and CD4+ T-cell counts, and compliance to HAART were not considered in our study. MSM can benefit from HPV vaccination due to immunity against genotype 16 and 18 and cross immunity with other high risk genotypes not included in the vaccine. Since anal cytology is very unspecific, especially in HIV negative patients (32-59%),10 to be used alone as screening, it is very important to screen with very sensitive assays such as PCR that detects not only genotypes 16 and 18 but genotypes 51, 31, 66 and other high risk genotypes in order to reduce the incidence of anal cancer.