Salmonellosis is an important public health problem. Turtles are increasingly involved in the role of transmitters of this infection to humans.
MethodsSalmonella cases are reported to the local Surveillance Agency where interviews are carried out to address possible exposures. Molecular epidemiology techniques were used to identify species.
ResultsIn this article we report two examples of this type of infection in two places, 300km apart in Spain. In Barcelona a turtle transmitted the disease to a small baby via her mother, and in Castellón 5 related cases of Salmonella infections were detected, and all were transmitted by imported turtles. Molecular epidemiology techniques confirmed the turtle-person transmissions and showed strong relationships between cases in Castellón and Barcelona.
DiscussionThese examples represent the tip of the iceberg of what is happening with pet reptiles as regards transmission of this infection. We believe that it is important to assess the impact of this type of infection in each country, in order to subsequently promote prevention strategies such as: regulations for pet shops, and educating/informing families who buy reptiles as pets.
La salmonelosis es un problema con un impacto importante en salud pública. Cada día es más importante el papel de las tortugas como transmisoras de esta enfermedad.
MétodosLos casos de salmonelosis son notificados a las Agencias de Vigilancia locales que realizan las encuestas pertinentes para valorar fuentes de exposición. Técnicas de epidemiologia molecular son utilizadas para identificar las especies.
ResultadosEn este artículo exponemos ejemplos de este tipo de transmisión en dos puntos de España que distan 300km. En Barcelona una tortuga transmitió la enfermedad a un bebé a través de su madre y en Castellón se registraron cinco casos de infecciones por Salmonella, todos ellos provocados por el contacto con tortugas. La epidemiologia molecular permitió confirmar la transmisión tortuga persona y así como una fuerte relación entre los casos de Barcelona y Castellón.
DiscusiónEstos ejemplos representan la punta del Iceberg en cuanto al papel de los reptiles en la transmisión de Salmonella. Creemos que evaluar el impacto de esta transmisión en los países es básico para poder aplicar y promover medidas preventivas. Normativas específicas en los puntos de venta de reptiles así como información y educación de las familias que pretenden comprar un animal de este tipo podrían ser muy útiles para disminuir el impacto de esta transmisión.
Salmonellosis is still an important public health problem worldwide. In the USA alone it has been estimated that there are approximately 1.5 million cases per year.1 In Spain it is the second cause of bacterial gastroenteritis, after that caused by Campylobacter.2,3
Salmonellosis is a zoonosis, the main reservoir being the intestinal tract of domestic and wild animals. There are over 2500 serotypes of Salmonella, 2000 of which can affect humans. Infection by Salmonella may involve diarrhoea, vomiting and fever. The clinical course of the infection is usually self-limiting; however it may also present a more severe ailment, and even end fatally in high risk patients such as babies, the elderly or patients with immunodeficiencies.4
In recent years an increase has been observed of Salmonella cases in humans directly or indirectly related with reptiles, mainly due to the increasing numbers of families who have such an animal at home.1,5–9 Usually the infection in these animals is asymptomatic, although it can become serious or even fatal.5
In Europe the number of families with small children who acquire a reptile as a pet is continually increasing and although it seems that the number of cases of salmonellosis associated with this form of exposure is increasing, we do not as yet have any data on this phenomenon.10 Before any programme for preventing this form of exposure can be set up, it is important to quantify the impact of the problem. The aim of the present article is to describe two outbreaks of infection by Salmonella in humans, associated with the same turtle type, which were detected in 2009 in Spain, in two towns 300km apart.
Description of the investigationInvestigation in CastellónBetween March and July 2009 two cases of infection by S. paratyphi B were reported to the Epidemiology Unit of the Castellon Public Health Centre (CSPCS), which covers an area with 450,000 inhabitants, and 71 towns. No case of such an infection [S. paratyphi B] had been reported during the previous 5 years. Both patients, aged 11 months (case J1) and 4 years (case J2), resided in the same town. The antibiograms of the two strains were identical. A CSPCS epidemiologist contacted the patients and their paediatrician in order to initiate an epidemiological investigation.
The symptoms consisted of gastroenteritis with fever lasting 3–5 days which was resolved with symtomatic treatment in out-patients. The two patients did not know each other and did not present any common antecedents, except that both had fresh-water turtles acquired prior to the onset of symptoms at the same pet-shop in their home town. During the investigation a third case (J3) was identified, the 2-year old brother of case J1 who had suffered similar symptoms and whose copro-culture revealed the same infection.
Samples of aquarium water were taken in the homes of case J2 and of cases J1 and J3. Moreover, the investigation made it possible for one of the turtles to be taken to and kept alive at the CSPCS, where 3 more samples of water were taken, on 9 July, and 14 August, this is important since excretion is not continuous.11 The five water samples were all positive to Salmonella. Three of the strains isolated were serotyped and were found to be: two Salmonella litchfield (strains A1 and A2, taken July 8) and one Salmonella paratyphi B var. Java (strain A3, taken July 9). The turtle was identified as being a Trachemys scripta troosti [Fig. 1].
Given these findings, all cases of salmonellosis diagnosed during the first half of 2009 in the CSPCS jurisdiction area were checked and two cases of gastroenteritis due to S. litchfield were identified. These corresponded to two children (cases L1 and L2) both 2 years old and living in the same town as the above cases, whose symptoms had appeared in January and May 2009, the only common antecedent being exposure at home to fresh-water turtles bought in the same pet shop as the other cases.
Investigation in BarcelonaOn 5 November 2009 the Barcelona Public Health Agency (ASPB), which covers the Barcelona city area with 1.6 million inhabitants, was notified of the case of an infant aged 11 months who had been admitted to the Hospital Universitario Vall d’Hebrón, after 9 days with vomiting, fever, bloody diarrhoea and dehydration (case B1). Microbiological tests isolated Salmonella. The infant's situation normalised following treatment with antibiotics and intravenous fluid therapy and was discharged on the seventh day. An ASPB epidemiologist contacted the infant's mother in order to initiate the field study. It was found that the family did not have a history of trips or of eating out (the infant was still being fed formula milk and purees of fruit or vegetables, all of which were always prepared by the mother). Moreover, the grandparents, brother and mother also had gastroenteritis during the same period. However, Salmonella was not isolated in the copro-cultures taken from any of the family members. The only exposure factor which could be associated with the infection was the family's possession of a pet turtle. This animal was identified as T. scripta troosti, and was mainly looked after by the mother, who reported that the baby neither had any direct contact with the turtle nor its aquarium. On November 24 a sample of aquarium water was taken, which was positive to Salmonella (strain A4). Serotyping was carried out on the strains isolated from the baby's copro-culture, and from the turtle's aquarium water, both being identified as S. paratyphi B var. Java.
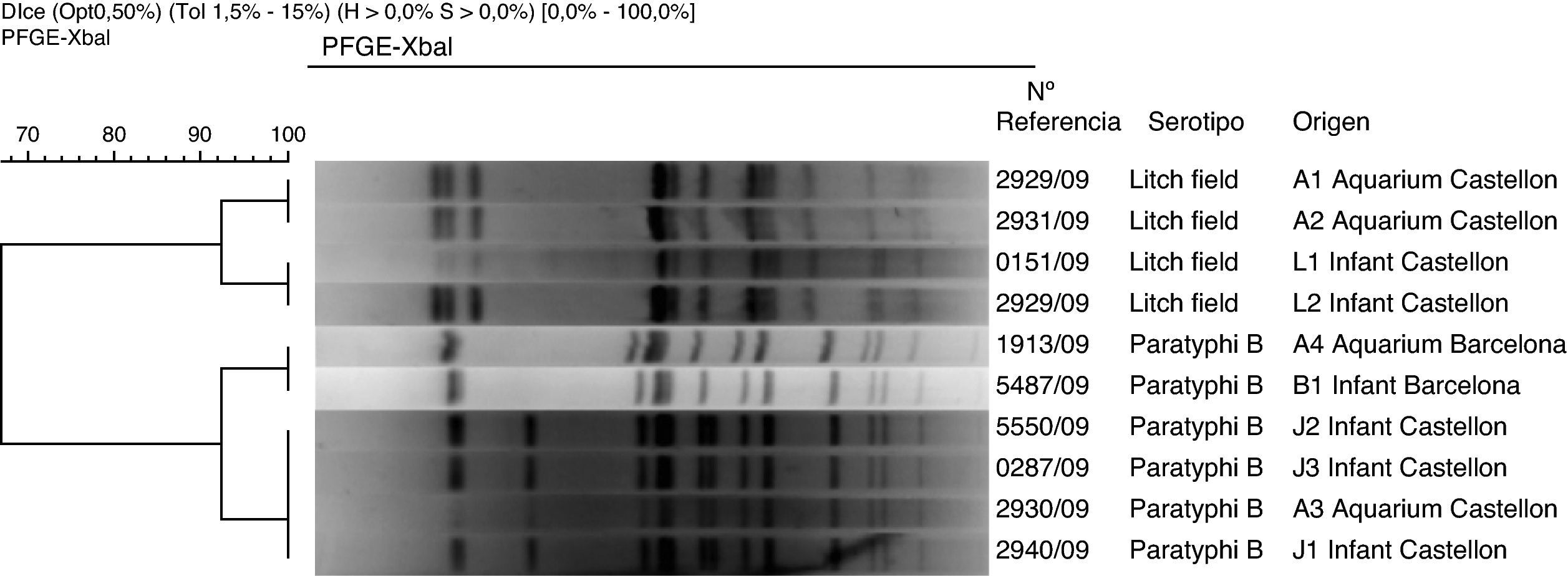
Characteristics of the two outbreaks are summarised in Table 1.
Outbreak characteristics.
| Barcelona | Castellón | |
| Year | 2009 | 2009 |
| Report method | Familiar outbreak | Cluster of cases |
| Confirmed cases | 1 | 5 |
| Hospital admission | 1 | 0 |
| First case | November 2009 | January 2009 |
| Last case | November 2009 | May 2009 |
| Cases’ age | 11 months | 11 months to 4 years |
| Families affected | 1 | 4 |
| Stools cultures to cases | S. paratyphi B. Java | S. paratyphi B. Java (3 cases)S. litchfield (2 cases) |
| Aquaria water samples (all resulted positive) | 1 | 4 |
| Result of aquaria samples | S. paratyphi B. Java | S. paratyphi B. JavaS. litchfield |
| Turtle type | Trachemis scripta troosti | Trachemis scripta troosti[all of them bought in the same pet shop] |
On arrival at the National Centre of Microbiology (CNM) strains of Salmonella were classified as S. paratyphi B and S. litchfield using the Kauffman–White technique.12 All strains of serotype paratyphi B belonged to the Java variety.
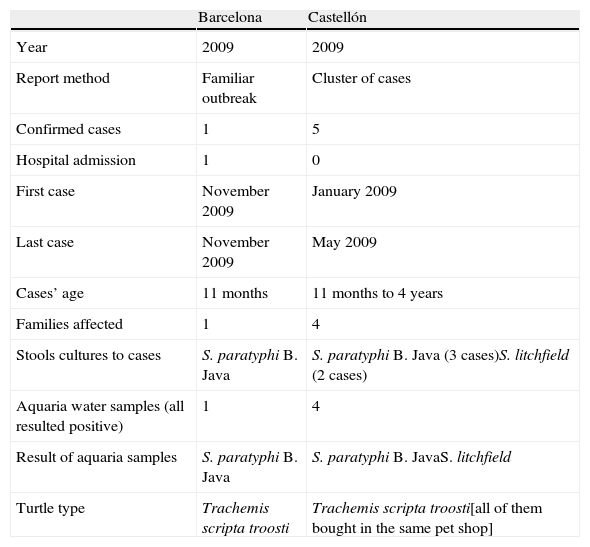
All human strains and 4 of those isolated from aquariums were of molecular-type using the pulsed field gel electrophoresis technique (PFGE-Xbal) following the protocol and interpretation criteria of PulseNet13 [Fig. 2].
In Castellón, all strains of S. paratyphi B var. Java, both from humans (cases J1–J3) and from the aquarium of one of the turtles (strain A3) were mutually indistinguishable. The human strains of Las S. litchfield (cases L1 and L2) were also mutually indistinguishable. The similarity between human strains of S. litchfield (from cases J1–J3) and those isolated from the turtle's aquarium water (strains A1 and A2) was >90%.
In Barcelona, the two strains studied (B1 and A4) were identified as S. paratyphi B, var. Java, mutually indistinguishable using PFGE-Xba. The similarity between the two Barcelona S. paratyphi B strains and those of Castellón was >90%. This suggests a strong relationship between cases for this particular serotype.
InterventionThe interventions employed in Barcelona and Castellón, with the aim of preventing more cases, were similar. Apart from follow-up of cases and environmental investigation, the families were given health education based on CDC recommendations for these cases, and official veterinary services carried out inspections with the aim of revising licenses in the pet-shops where these animals were sold.
DiscussionIn the present study we have described 6 cases of salmonellosis in children ranging in age from 11 months to 4 years related with exposure at home to pet turtles in 2009.
Turtles are reservoirs of Salmonella and their role as transmitters of this disease has been studied.14–17 Two different serotypes were involved in these 6 cases: S. paratyphi B var. Java and S. litchfield.5 Seldom studies have been done on investigations of serovars of Salmonella on reptiles and just one of them was done in our country.16 Highest prevalence of turtles infection has been found in 1972 in an American study that showed that up to 85% of domestic turtles were contaminated with this bacteria18 and a recently published Colombian study19 reported as 35% of the samples were positive to Salmonella and most of them were corresponding to Salmonella enteritidis. None of the serotypes detected in our work have been detected in those prevalence studies in reptiles.16,19–21 However, it is plausible that these varieties of Salmonella may infect both reptiles and humans, and while there are no relevant European studies showing this association, this relationship has been previously identified in the USA. A case-control study conducted in 2009 evaluated the strength of association between infections by S. paratyphi B and previous exposure to turtles, and an OR of 2.8 was found.22 For S. litchfield such relation has been previously described only once, in 2006, in the United States.23 The relationship between turtles and Salmonella infection (without distinguishing serotypes), has also been evaluated in various studies, finding OR values of 2.4624 and of 16.5.25 In USA, of the approximately 1.5 million cases annually of Salmonella, 74,000 are attributed to exposure to reptiles.6,10 It has been estimated that in between 3 and 5% of all cases of salmonellosis there is some association with reptiles.7
In Sweden, between 1990 and 2000, a total of 339 cases were reported of Salmonella infections associated with reptiles.26
In the present study we describe 5 cases of minor infection, and one serious one; this is a reminder that while in most cases Salmonella infection is banal and self-limiting, it can still lead to complications requiring hospitalisation and invasive treatment. There are many cases of serious infections by Salmonella associated with contact with turtles,27 serious cases in babies28 or in immunodepressed patients,29 and even fatal cases.23
It is becoming ever more common for families with small children to acquire a turtle as a pet, and therefore the number of Salmonella infections due to this exposure is increasing. We have no data on the incidence or impact of these infections in Spain, and although there are various reports of such infections in Europe, there are no global indicators that measure their magnitude. Given the high prevalence of infections associated with turtles, since 1975 legislation in the USA prohibits sale and distribution of small turtles (under 10.2cm in length).26 This legislation has been associated with an important decline in the annual number of infections of this nature. However, the fact that the law is not rigorously obeyed and that it has certain exceptions (sale for educational purposes), means that cases continue to appear.23,30 Prior to 1996 in Sweden there was a law that required imported turtles to be certified free of Salmonella infection. This requirement ceased to exist after Sweden joined the European Union (1996). There is some evidence that this legislative change provoked a rise in the incidence of this pathology, from 0.15/100,000 to 0.79/100,000 cases.26 When this became known, an educational television campaign was mounted, which reduced the incidence to 0.46/100,000, showing that both restrictions on importation and the information campaigns are effective measures for dealing with human salmonellosis associated with reptiles.
After important restrictions in turtle importation and commercialisation in USA, this business was redirected to other places such as Europe, where until now there are no importation or selling regulations regarding this matter.
The present article shows that in Spain there is a clear relationship between human salmonellosis and pet turtles exposure. Even though limited to the description of a few cases identified in Barcelona and Castellón as a result of a professional collaboration, we are certain that a considerable number of turtle-related cases Salmonella must occur which could neither be investigated nor be counted. Moreover, the number of families acquiring exotic turtles, normally from the USA, is continually increasing.
For these reasons we believe that it would be important to evaluate the extent of this problem in Spain and in Europe, based on the individualised notification and investigation of cases.
The vast majority of these turtles are exotic, and although importers ensure their Salmonella free culture proceedings, bad conditions of their transportation and their maintenance in pet shops facilitates bacterial growth and increases the risk of associated infections.31
Based on the available evidence, it is not easy to affirm that turtles are free of Salmonella32 due to the irregular secretion of the bacteria and hence it would not be appropriate to require them to have a certificate to this effect. We believe that flat prohibition of turtle sales is also too drastic as a measure.
However, controlled import quotas, promotion of educational campaigns for both the general public and pet shops, and getting the shops to comply strictly with regulations would all be basic steps to help prevent this type of infections.
Conflicts of interestThe authors have no conflicts of interest to declare.
The authors would like to thank the patients and families for their collaboration during the interviews. They are also sincerely grateful to the paediatricians who treated the children: Inmaculada Rius and Jaume Izquierdo, and to all the people related to microbiology work: Pilar Pons, Julia Quirós and Ana Gimeno in Castellón and Virginia Rodriguez and M.a Dolors Ferrer in Barcelona. Other important collaborators of this study for which the authors would like to acknowledge are: Antonio L. García-Sanz, Judith Hidalgo, Milagros Sanz and Carmen Díaz-Paniagua.