Different species of the genus Dirofilaria, mainly D. immitis and D. repens, are responsible for emergent vector borne transmitted zoonotic diseases in the Old World. Human D. repens infections are characterized by the appearance of benign subcutaneous nodules that mimic skin malignant tumors or due to live worms in the ocular area.
MethodsThirty patients presenting superficial or deep nodules were treated at the Rostov Regional Diagnostic Center (Southwestern Russian Federation). Anatomical characteristics of the nodules were studied by non-invasive ultrasound and color and power Doppler techniques. Worms were surgically removed from every nodule and their DNA analyzed by polymerase chain reaction (PCR).
ResultsTwenty-four out of the 30 nodules were located in the hypodermis, two in a retro-ocular location and four in scrotal location. Image techniques allowed the identification of the helminthic origin of all nodules, based on their oval and regular shape, peripheral vasculature, and the existence of internal linear winding hyperechoic structures with or without movements, indicating the presence of live or dead worms, respectively. Specific adscription to D. repens was achieved by the PCR analysis.
ConclusionThe series described in the present paper confirms the increasing risk of infection by D. repens in humans living in endemic areas of Eastern Europe. The use of non-invasive ultrasounds and Doppler techniques can contribute to an appropriate management of human dirofilariasis. Moreover, awareness of the medical community in the endemic areas influences the report of cases, and consequently the current epidemiological picture of human dirofilariasis.
Diferentes especies del género Dirofilaria, principalmente D.immitis y D.repens, son responsables de enfermedades zoonóticas transmitidas por vectores en el viejo mundo. Las infecciones humanas causadas por D.repens se caracterizan por la aparición de nódulos subcutáneos benignos que se confunden con tumores malignos de piel o por la localización de vermes vivos en la zona ocular.
MétodosTreinta pacientes con nódulos superficiales o profundos fueron tratados en el Centro de Diagnóstico Regional de Rostov (suroeste de la Federación Rusa). Las características anatómicas de los nódulos fueron estudiadas mediante ultrasonidos no invasivos y Doppler de color y potencia. Los vermes se retiraron quirúrgicamente de cada nódulo y su ADN se analizó mediante la reacción en cadena de la polimerasa (PCR).
ResultadosVeinticuatro de los 30 nódulos se localizaron en la hipodermis, 2 en localización retroocular y 4 en la zona escrotal. Las técnicas de imagen permitieron la identificación del origen helmíntico de todos los nódulos, en base a su forma ovalada y regular, la vasculatura periférica y la existencia de estructuras lineales internas hiperecoicas con o sin movimientos, indicando la presencia de gusanos vivos o muertos, respectivamente. La adscripción específica a D.repens se logró mediante el análisis de PCR.
ConclusiónLa serie de casos descrita en el presente trabajo confirma el creciente riesgo de infección por D.repens en las personas que viven en zonas endémicas del Este de Europa. El uso de técnicas no invasivas como los ultrasonidos y el Doppler puede contribuir a un adecuado manejo de la dirofilariosis humana. Por otra parte, el conocimiento de la enfermedad por parte de la comunidad médica de las áreas endémicas influye en el informe de los casos y, consecuentemente, en el cuadro epidemiológico actual de la dirofilariosis humana.
Zoonotic filarioses are vector borne transmitted diseases caused by parasitic filarial nematodes of the genus Dirofilaria, mainly D. immitis and D. repens. These two species are primarily parasites of domestic and wild canines and felines all over the world1 being transmitted by different species of culicid mosquitoes belonging the genera Culex, Aedes and Anopheles.2 Because many of these species feed indiscriminately on animal reservoirs and man, in areas where canine dirofilariosis is endemic, the risk of human infections exists.3 In Europe, canine dirofilariosis caused by D. repens is spreading from the traditionally endemic Southern Mediterranean countries to the central and Northern countries, being currently considered an emerging disease in these areas. In parallel, a dramatic increase of human subcutaneous/ocular dirofilariosis is being detected, with more than 2850 cases reported until now in the world literature, many of them diagnosed in the last 13 years in Ukraine and Southwestern Russia.4,5 These changes are attributed to the global warming, human interventions modifying environment and pets management.6 Human subcutaneous dirofilariosis is a condition characterized by the development of subcutaneous nodules caused by the local inflammatory reaction against D. repens worms, usually immature, that mimic both benign and malignant primary or metastatic skin tumors.7 In addition live, fully developed adult worms can lodge in intraocular and retroocular locations, causing considerable damages and discomfort in patients by themselves or as a consequence of their surgical removal.8,9 Diagnosis of human subcutaneous dirofilariosis raises important procedure problems because of the initial suspicion of a malignant origin of the nodules and the very frequent absence of parasite larvae (microfilariae) in the blood of patients.4 Thus, most cases are diagnosed by histology and morphological and/or molecular analysis, subsequent to the surgical removal of the whole cysts or the worm themselves.7,10,11
The aim of this work is to report an extensive series of human subcutaneous/ocular dirofilariosis cases observed during an 11-year period (2003–2013) in the Rostov Oblast Diagnostic Center, located in the hyperendemic area of canine dirofilariosis in Southwestern Russian Federation.
MethodsCases of human subcutaneous dirofilariasis were retrospectively collected from the case record of the Rostov Regional Diagnostic Center Department of Ultrasound. This center functions as referral medical center of the Rostov region which has a population of 4,277,976 inhabitants. Cases were referred from ophthalmologists, surgeons, oncologists, urologists, or from other physicians for assessment of subcutaneous or more deeply located nodules. The data were gathered reviewing the clinical charts or the clinical, laboratory and imaging registries.
Ultrasound examinations were performed in all patients on ultrasound equipment SonoCT HDI-5000 and iU22 “Philips” (Philips Healthcare, Bothell, WA, USA), using a broadband linear probes with an aperture of 38mm and the frequency of 5–12MHz and 5–17MHz. Patients were examined with multiple views scanning with the special program for superficial tissues study in B-mode as well as using a regimen of color and power Doppler with spectral curve analysis of blood flow. Ultrasounds study evaluated the skin thickness, the echogenicity and echo structure of the nodule itself and the structure of surrounding superficial and deeper tissues. Every nodule was characterized by the size, shape, borders, homogeneity, detailed characteristics of internal echo structure, presence or absence of blood flow and vascular pattern. All the nodules were afterwards surgically excised and the removed worms analyzed by the PCR technique with specific primers as described by Favia et al.12 In brief, DNA was extracted from each parasite with the DNeasy Blood & Tissue Kit (Qiagen, GmbH, D-40724). After activation of the Taq Gold polymerase at 94°C for 12min, PCR reactions were performed as follows: 94°C (30s), 65°C (30s), 72°C (30s) for 35 cycles and a final step at 72°C for 7min. PCR products were visualized on agarose gel.
All patients provided informed consent to participate in this study having been approved by the Ethical Committee of the Rostov State Medical University.
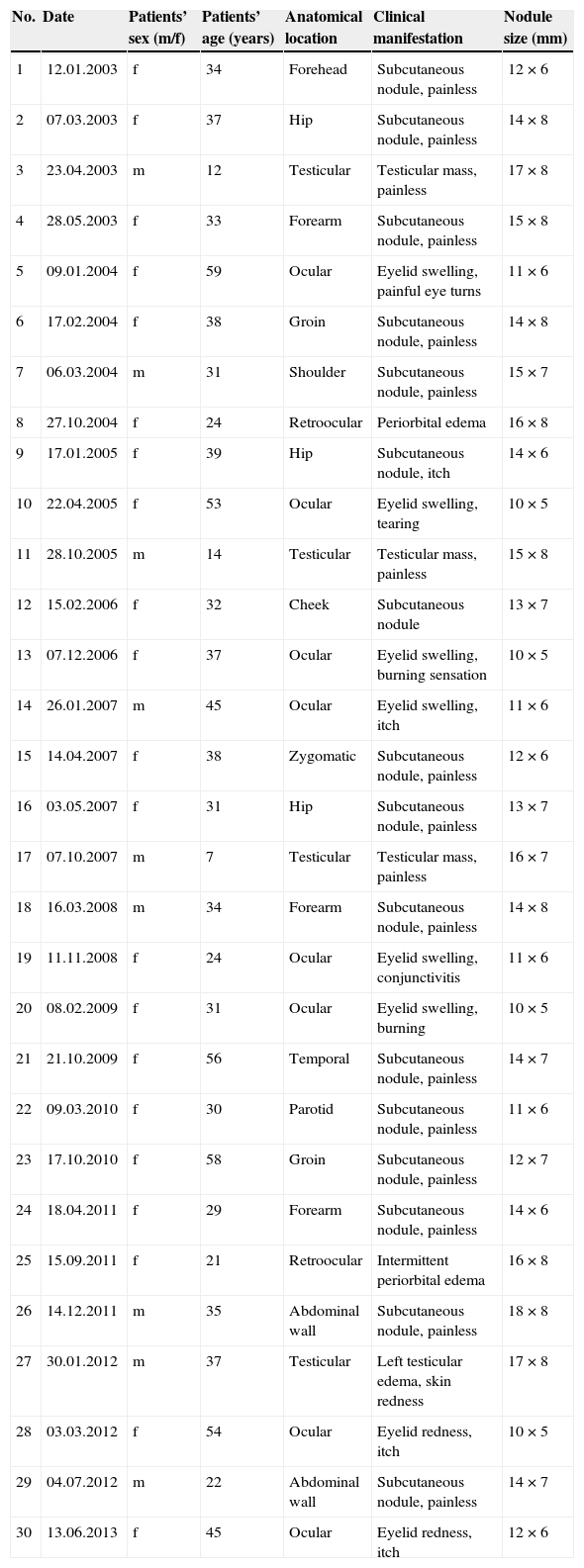
ResultsBetween 2003 and 2011, 30 patients (21 females) were diagnosed of dirofilariosis. Patients noticed a single superficial or deep nodule without history of previously diagnosed malignancies. Data on the patients, characteristics and location of the nodules appear in Table 1. The most common presentation was a painless subcutaneous nodule, visible with naked eyes (26/30) or found by palpation (2/30). Twenty-four out of the 30 nodules were located in the hypodermis and the other six were located in deeper locations. From these, two out of the 10 ocular cases appeared in retroocular location, and four additional cases in the scrotum. All the patients with ocular dirofilariosis reported history of swelling of the lower or upper eyelids or periorbital edema, burning sensation, itching, painful eye turns, conjunctival hyperemia and tearing. Some of them had the feeling of a foreign body in the eye. The patients with scrotal lesions presented with non-tender local soft tissue mass located separately from testicular appendages. One of the patients noticed a gradual increasing edema as well as hyperemia of one half of the scrotum without definite mass lesion. In other patient physical examination revealed a soft painless mass closely adjacent to the caudal portion of the epididymis (the first clinical impression was “a cyst of caudal epididymis”). Patients with other location of the nodules were asymptomatic. None have traveled outside the Rostov region in the previous past years.
Main clinical and epidemiological characteristics of 30 cases of dirofilariosis (Dirofilaria repens) reported in Rostov-on-Don (Southwestern Russia), 2003–2013.
| No. | Date | Patients’ sex (m/f) | Patients’ age (years) | Anatomical location | Clinical manifestation | Nodule size (mm) |
|---|---|---|---|---|---|---|
| 1 | 12.01.2003 | f | 34 | Forehead | Subcutaneous nodule, painless | 12×6 |
| 2 | 07.03.2003 | f | 37 | Hip | Subcutaneous nodule, painless | 14×8 |
| 3 | 23.04.2003 | m | 12 | Testicular | Testicular mass, painless | 17×8 |
| 4 | 28.05.2003 | f | 33 | Forearm | Subcutaneous nodule, painless | 15×8 |
| 5 | 09.01.2004 | f | 59 | Ocular | Eyelid swelling, painful eye turns | 11×6 |
| 6 | 17.02.2004 | f | 38 | Groin | Subcutaneous nodule, painless | 14×8 |
| 7 | 06.03.2004 | m | 31 | Shoulder | Subcutaneous nodule, painless | 15×7 |
| 8 | 27.10.2004 | f | 24 | Retroocular | Periorbital edema | 16×8 |
| 9 | 17.01.2005 | f | 39 | Hip | Subcutaneous nodule, itch | 14×6 |
| 10 | 22.04.2005 | f | 53 | Ocular | Eyelid swelling, tearing | 10×5 |
| 11 | 28.10.2005 | m | 14 | Testicular | Testicular mass, painless | 15×8 |
| 12 | 15.02.2006 | f | 32 | Cheek | Subcutaneous nodule | 13×7 |
| 13 | 07.12.2006 | f | 37 | Ocular | Eyelid swelling, burning sensation | 10×5 |
| 14 | 26.01.2007 | m | 45 | Ocular | Eyelid swelling, itch | 11×6 |
| 15 | 14.04.2007 | f | 38 | Zygomatic | Subcutaneous nodule, painless | 12×6 |
| 16 | 03.05.2007 | f | 31 | Hip | Subcutaneous nodule, painless | 13×7 |
| 17 | 07.10.2007 | m | 7 | Testicular | Testicular mass, painless | 16×7 |
| 18 | 16.03.2008 | m | 34 | Forearm | Subcutaneous nodule, painless | 14×8 |
| 19 | 11.11.2008 | f | 24 | Ocular | Eyelid swelling, conjunctivitis | 11×6 |
| 20 | 08.02.2009 | f | 31 | Ocular | Eyelid swelling, burning | 10×5 |
| 21 | 21.10.2009 | f | 56 | Temporal | Subcutaneous nodule, painless | 14×7 |
| 22 | 09.03.2010 | f | 30 | Parotid | Subcutaneous nodule, painless | 11×6 |
| 23 | 17.10.2010 | f | 58 | Groin | Subcutaneous nodule, painless | 12×7 |
| 24 | 18.04.2011 | f | 29 | Forearm | Subcutaneous nodule, painless | 14×6 |
| 25 | 15.09.2011 | f | 21 | Retroocular | Intermittent periorbital edema | 16×8 |
| 26 | 14.12.2011 | m | 35 | Abdominal wall | Subcutaneous nodule, painless | 18×8 |
| 27 | 30.01.2012 | m | 37 | Testicular | Left testicular edema, skin redness | 17×8 |
| 28 | 03.03.2012 | f | 54 | Ocular | Eyelid redness, itch | 10×5 |
| 29 | 04.07.2012 | m | 22 | Abdominal wall | Subcutaneous nodule, painless | 14×7 |
| 30 | 13.06.2013 | f | 45 | Ocular | Eyelid redness, itch | 12×6 |
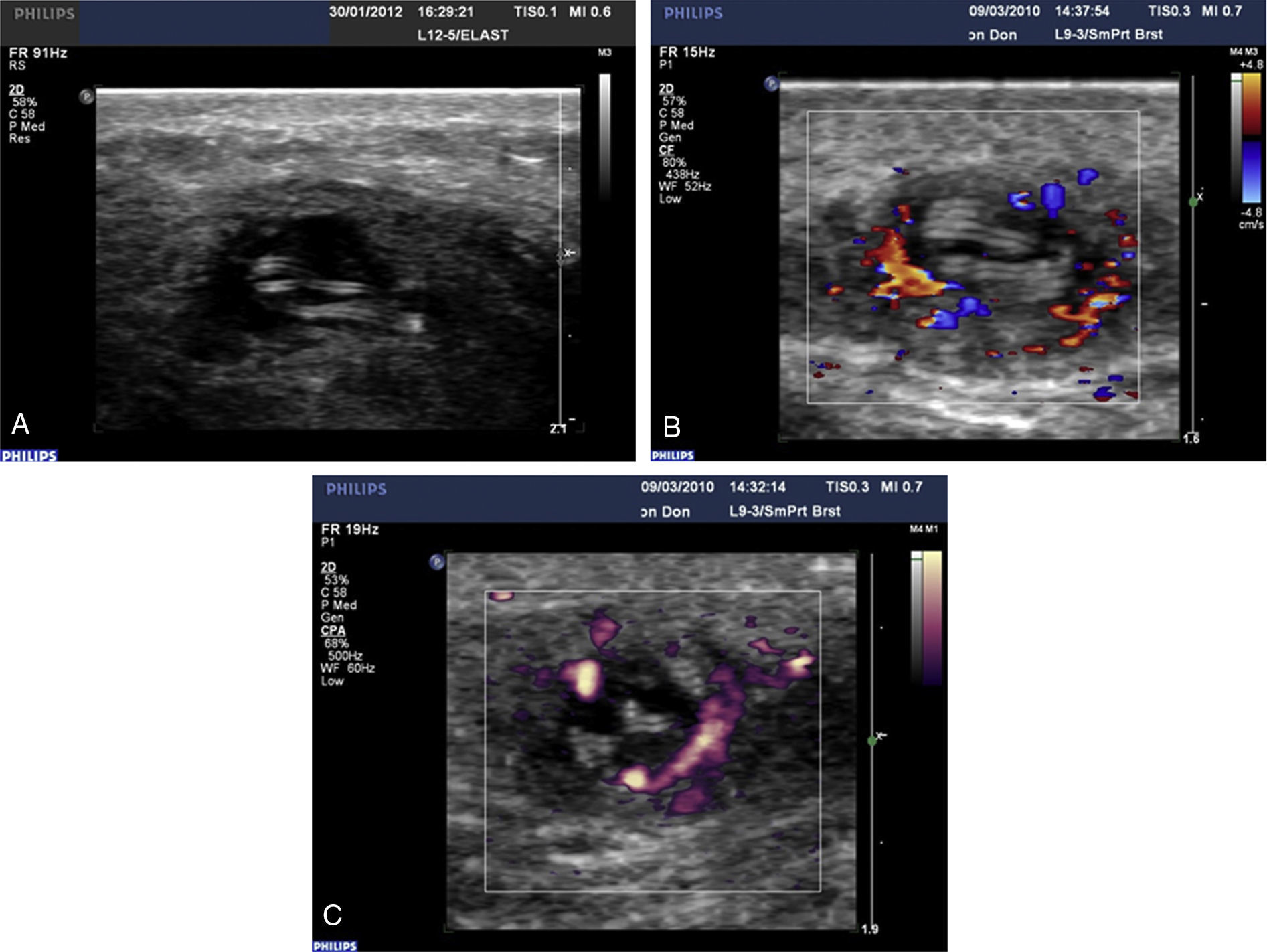
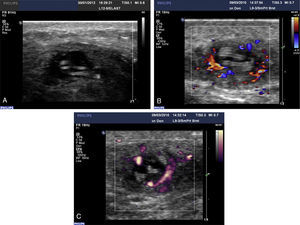
By ultrasound examination, nodules were oval and regular-shaped with well-defined but jagged and fuzzy outer contours. The inner contents of the cyst appear hypoechoic. Inside the nodule there were clear internal echoes with linear winding hyperechoic textures (Fig. 1A), sometimes with visible spontaneous writhing movement, detected in 14 out of 30 cases, indicating the presence of a live worm. Alive worms looked rich with hank-like multiple continuing and sharp but fine tubular textures. Dead worm showed the same structures but they looked motionless, non-continuous, mostly blurred and broken, with areas of high and low echo density. Color Doppler examination detected that none of the nodules showed any signs of internal or polar vascularity, the blood vessels being present at the periphery of the parasitic cyst wall (Fig. 1B). Power Doppler examination confirmed the existence of blood flow only at the periphery of the nodules in the fibrotic capsule surrounding the worms (Fig. 1C) and adjacent tissues. The two nodules detected at retroocular location showed the same characteristic findings to those described in the rest of the nodules in both ultrasounds and color and power Doppler examinations. These characteristics allowed the attribution of the origin of all nodules to a helminthic origin, probably Dirofilaria.
Representative images from a B-scan ultrasound (A, case no. 27) and color and power Doppler sonography (B and C) examination of a parasitic nodules (both from case no. 22). Parasite appears as multiple parallel hyperechoic linear structures (rail track pattern) inside the cysts and blood flow is located in the periphery of the capsule.
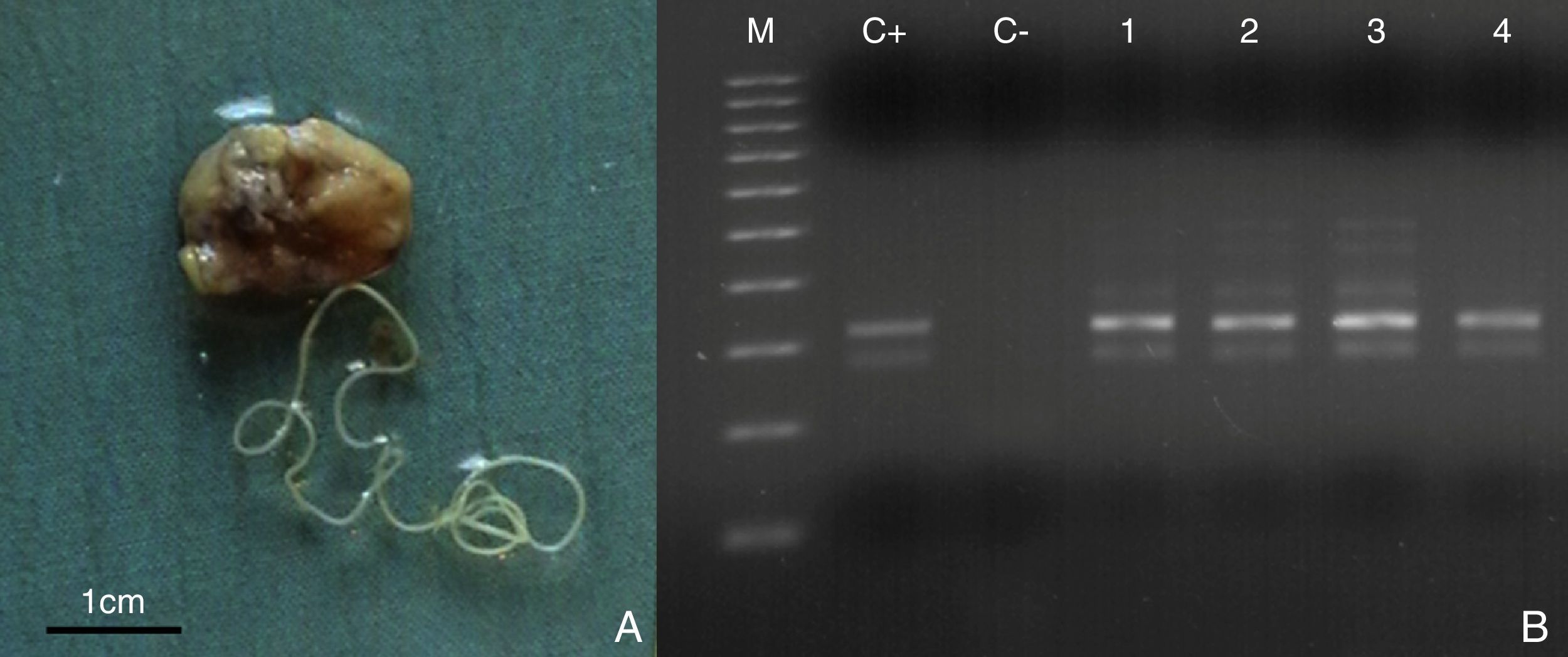
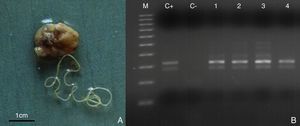
Surgical removal of the parasites revealed the presence of round worms with filiform appearance with lengths from 42 to 124mm and diameters from 102 to 527μm. They were sexually immature female worms in 28 out of 30 cases (Fig. 2A) and 2 immature male worms in the other 2 cases. PCR identified all of them as D. repens (Fig. 2B). Laboratory examination did not demonstrate any kind of abnormalities in conventional blood, urine and biochemistry tests.
Subcutaneous nodule containing a female worm surgically removed from a patient. The scale bar is in cm (A). Representative image of the PCR analysis of the DNA extracted from different worms after the surgical removal of the nodules (B). The dirofilariotic nodules were located in subcutaneous tissue of the shoulder (case no. 7) (Lane 1), ocular area (case no. 10) (Lane 2), testicular (case no. 17) (Lane 3), abdominal wall (case no. 26) (Lane 4) and. M, 100bp DNA marker; C+, positive control; C−, negative control.
In spite of human dirofilariosis has been considered traditionally a rare disease13,14 both the increase in clinical cases,4 mainly caused by D. repens, and the high seroprevalences revealed by serological surveys in humans15 suggest a high risk of infection by Dirofilaria species for people living in areas where dirofilariosis is endemic in dogs.3 At a global level the area with the highest increase in human dirofilariosis cases is Europe where approximately 280 cases were reported until 2000, most of them in the Mediterranean countries. However, in the next 13 years the number of reported cases surpassed 2400 from which 2087 were reported in Ukraine and the Russian Federation. Moreover, with increasing frequency clinical cases are reported in Central and Northern European countries, previously considered non-endemic.4,5,15 These changes have been associated, among other factors, to the strong thermal anomalies occurring in the area in the last years16 and the wide stray dogs population not receiving chemoprophylaxis against Dirofilaria. The cases described here were reported in a single Hospital of Rostov-on-Don (Southwestern Russia), where previous epidemiological surveys revealed canine prevalences higher than 30%.15 This indicates a clear concordance among the existence of Dirofilaria in dogs and the detection of human cases. Nevertheless, there are high canine prevalences in other Southwestern Russian oblasts where only sporadic or no human cases have been reported, suggesting that the awareness of the medical community is also necessary for the correct diagnosis of human dirofilariosis.4
Our series present similar epidemiological and clinical characteristics to those described previously by Pampiglione and Rivasi17 in their review of the world literature, with some different aspects. Ocular location is by far the most frequent, a fact that is in agreement with the high incidence of ocular cases reported in Russia as reviewed by Avdiukhina et al.18 Two of these cases appeared in retroocular location, having been one of them separately published to communicate this new anatomical location of D. repens.9 Because of the repetition of this presentation, it is necessary to warn the physicians about the possibility to find nodules in this anatomical location in the future. The frequency of genital location in our series (13.3%) is twice that found by Pampiglione and Rivasi17 and appeared mostly in adolescents. There exist also differences in the distribution by gender because we have observed 70.0% of incidence in women, clearly higher than 55.4% reviewed by Pampiglione and Rivasi.17
Detection of Dirofilaria nodules frequently causes the initial suspicion of a malignant origin, in spite of their benign character.3 Thus differential diagnosis is an essential step of the management of human dirofilariosis.7,19 Diagnosis of subcutaneous dirofilariosis is post-operative in most cases, causing moderate to serious injury to patients, mainly when nodules appear in internal, intraocular or retroocular locations.8,9 To avoid unnecessary damages and delay during the diagnostic procedure, efficient non-invasive techniques can be applied. The results obtained in the wide series of cases presented here consistently demonstrate the ability of ultrasounds combined to color and power Doppler technique in the presumptive attribution of these nodules to a dirofilariotic origin, in both superficial and deep locations. While in canine and feline cardiopulmonary dirofilariosis echocardiographic techniques are routinely used for the diagnosis and evaluation of the clinical situation of the hosts,20 these techniques have been successfully applied in the definitive diagnosis of human dirofilariosis only in very few cases21–23, or were used only to guide fine needle aspiration biopsy.24,25 The identification of the helminthic origin of the nodules, discarding a malignant tumor, was achieved according to morphological aspect of the nodules, the presence of worms which appear as parallel hyperechotic lines inside them and even their movements in nearly half of the cases and the peripheral location of blood vessels in Dirofilaria nodules, unlike what happens in malignant tumors, where the vascularization appears inside the nodule. Specific adscription to D. repens and thus confirmation of suspicions acquired by ultrasounds and Doppler examinations was performed in all cases by PCR once removed the nodules or the worm themselves. Nevertheless, once identified the dirofilariotic origin of the nodules and discarded a malignant origin, this is a secondary matter19 that must be performed when prognosis make necessary the removal of the nodules or worms.
In conclusion, we present here the report of a wide series of cases of human dirofilariosis in a hospital of a hyperendemic area of dirofilariosis in Southwestern Russia by means of image and molecular techniques. These techniques allowed the identification of dirofilariotic origin of all nodules located in both superficial and deeper locations. Results of epidemiological surveys and estimations of prediction models6,26 suggest a spreading of dirofilariosis both in animal reservoir and human populations of Northern and Eastern European countries. Thus human subcutaneous/ocular dirofilariosis would be diagnosed with increasing frequency in the nearest future in Europe.
Conflict of interestThe authors have no conflict of interest to declare.