A 61-year old woman with a history of end-stage liver disease presented to the Emergency Department with complaint of fever, chills and vomiting for 12h. She denied cough, dyspnea, abdominal pain or any other symptom. She was admitted; blood cultures and urine culture were taken, two blood culture sets incubated within 24h of admission were positive with grew Gram-negative rods, and ertapenem 1g q24h was started. She persisted with fever. The past medical history including cryptogenic Cirrhosis on May 2018, for which she received treatment with diuretics and systemic hypertension without acute complications, on chronic treatment with antihypertensive drugs. She owns a domestic dog, denied alcohol, tobacco or drug use as well as trips in the last year and other serious debilitating health conditions, hereditary hemochromatosis, chronic diseases such as diabetes mellitus, rheumatoid arthritis, thalassemia major, chronic renal failure, and lymphoma.
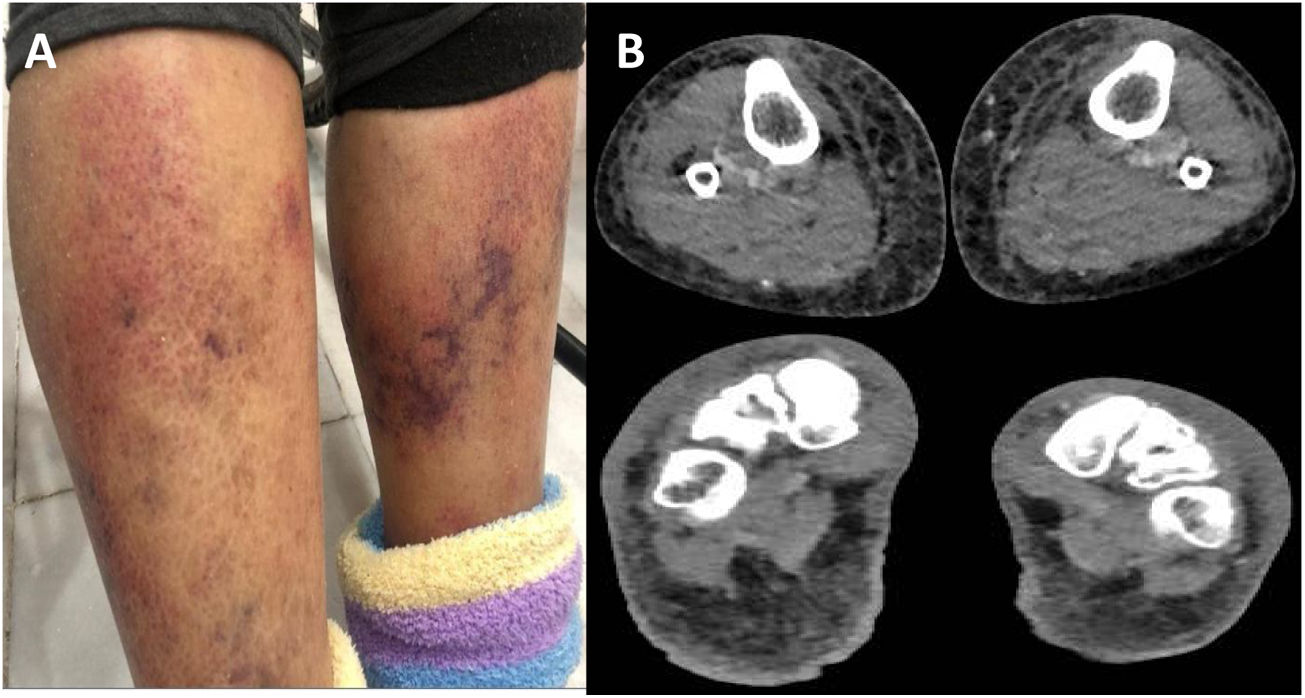
On examination, the patient was alert and interactive. She had 110/70-mmHg blood pressure, pulse 85beats/min, temperature 101.3°F (38.5°C), respirations 18breaths/min and O2 saturation 95%. An erythematous rash with ecchymosis was noted in the front of the legs below the knees (Fig. 1A). No other relevant sign was found on physical examination.
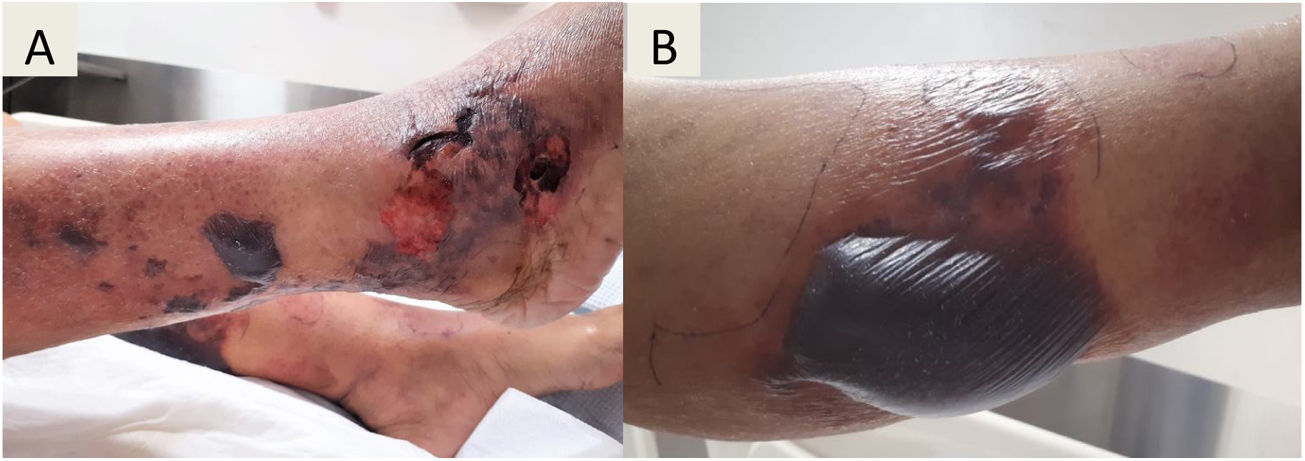
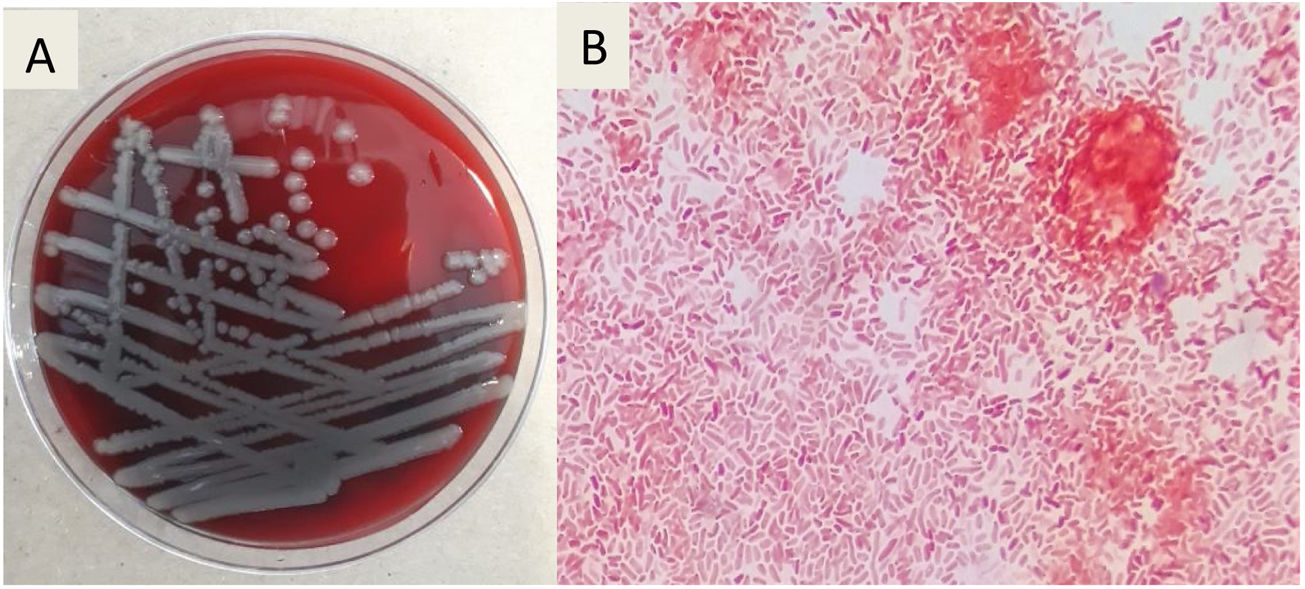
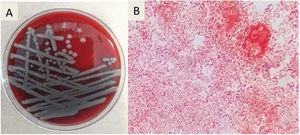
Diagnosis and evolutionThe initial laboratory investigations revealed white blood count of 3.9× 103 (reference range: 4–12), with 81% neutrophils, and 8% lymphocytes, the hemoglobin was 11.5g (reference range 13–15.7g/dL), platelet count was 40K/μL (reference range: 150–400). C-reactive protein was normal (CRP of 0.28mg/dL, reference range: 0–1), the concentrations of procalcitonin shows high level of ≥10μg/L. The liver tests reported: total bilirubin 3.5mg/dL (reference range: 0.3–1), alanine aminotransferase 32.9U/L (reference range: 7–52), aspartate aminotransferase 52U/L (reference range: 13–39), alkaline phosphatase 193U/L (reference range: 34–104). Kidney function was normal, with a creatinine level of 0.73mg/dL (reference range: 0.7–1.3). HIV and viral hepatitis serologies (acute and chronic) were negative. Blood cultures grew Gram-negative rods. A chest radiograph was normal and magnetic resonance imaging (MRI) of lower extremities showed bilateral soft tissue edema without fascial involvement (Fig. 1B). After 72h of empirical ertapenem, the patient continued with fever and presented progression of skin lesions with the appearance of multiple hemorrhagic bullae, the largest of 8cm by 4cm (Fig. 2A, B). She had severe lower limbs pain and edema. The patient became diaphoretic, tachycardic, tachypneic and hypotensive; resuscitation with crystalloid and norepinephrine was begun. The patient presented multiple organ failure and was admitted to the intensive care unit. The Gram-negative rods were identified as Vibrio vulnificus (Fig. 3A), BacT/Alert 3D system was used for the analysis of blood cultures, the identification of the specie was carried out using VITEK 2 system, antibiotic susceptibility profile shows that isolate was susceptible to antibiotics recommended for treating Vibrio infections (cefotaxime, ceftazidime, ceftrixone, TMP/SMX, quinolones and tetra-cyclines). It was learned that the patient consumed raw seafood 24h before presentation to the Emergency Department. Ceftazidime and doxycycline were started.
Follow-up laboratory investigations showed elevated liver function tests: total bilirubin: 6mg/dL (reference range: 0.3–1), alanine aminotransferase 86U/L (reference range: 7–52) and aspartate aminotransferase 140U/L (reference range: 13–39). The renal function worsened, with a creatinine of 2.7mg/dL and oliguria; disseminated intravascular coagulation was identified with an INR of 3.6, fibrinogen of 96mg/dL and oral bleeding. Platelets and fresh frozen plasma were transfused. The patient persisted with intense and progressive pain and underwent surgical exploration. Fasciotomy was performed for suspected compartment syndrome. V. vulnificus was isolated from the bullae and subcutaneous cellular tissue culture (Fig. 3B). Antimicrobial testing showed susceptibility to ceftazidime and doxycycline.
Bullae presented spontaneous drainage of serous fluid. Despite treatment, she presented refractory septic shock, worsening liver function and the skin lesions progressed to deep necrotic ulcers. Surgical debridement was performed 10 days after presentation. The patient died 2 weeks after admission due to disseminated intravascular coagulation and acute on chronic liver failure.
Final commentV. vulnificus is a halophilic, motile, Gram-negative bacillus capable of causing severe to life-threatening infection.
The main risk factor for V. vulnificus infection is chronic liver disease, especially cirrhosis due to alcoholism or chronic hepatitis such as hepatitis B or C. Other risk factors include underlying cancers or immunosuppressive chemotherapy, acquired immunodeficiency syndrome, end-stage renal disease, gastrointestinal disorders, diabetes mellitus, and hematological disorders characterized by elevated iron levels such as hemochromatosis.1,2
Virulence of V. vulnificus has been associated with a variety of potential factors: production of an anti-phagocytic polysaccharide capsule, metalloprotease VvpE, the cytolysin/hemolysin VvhA, and the multifunctional autoprocessing repeats-in-toxins (MARTX) toxin. and iron availability and iron acquisition systems.3,4
The spectrum of illness varies from gastroenteritis to primary sepsis and necrotizing fasciitis. V. vulnificus is the most lethal species; the case-fatality rate has been reported to exceed 50% in primary sepsis.
V. vulnificus infection is suspected based on clinical and epidemiological findings and is confirmed by bacteriological culture. Because bacteremia is common, routine Blood cultures should be performed when this infection is suspected.2
This patient had a chronic liver disease and a history of seafood consumption, the latter being reported in up to 90% of cases.
Case fatality rates for V. vulnificus infections have been shown to increase with delays between the onset of illness and administration of antibiotics; appropriate antibiotic treatment should be immediately administered. Furthermore, in many patients with serious skin and soft tissue infections such as necrotizing fasciitis, surgical interventions such as debridement or fasciotomy are necessary.5,6
The CDC recommends doxycycline 100mg intravenously or orally plus ceftazidime (or any other third-generation cephalosporin) for the treatment of V. vulnificus infection. This patient received proper management, however her evolution was poor. Surgical debridement was also performed, however, liver function deteriorated, which is associated with higher mortality.
The teaching point of this case is that V. vulnificus septicemia should be considered a differential diagnosis in patients with chronic liver disease and fever. Seafood consumption should be questioned on admission in all patients with fever and cirrhosis.