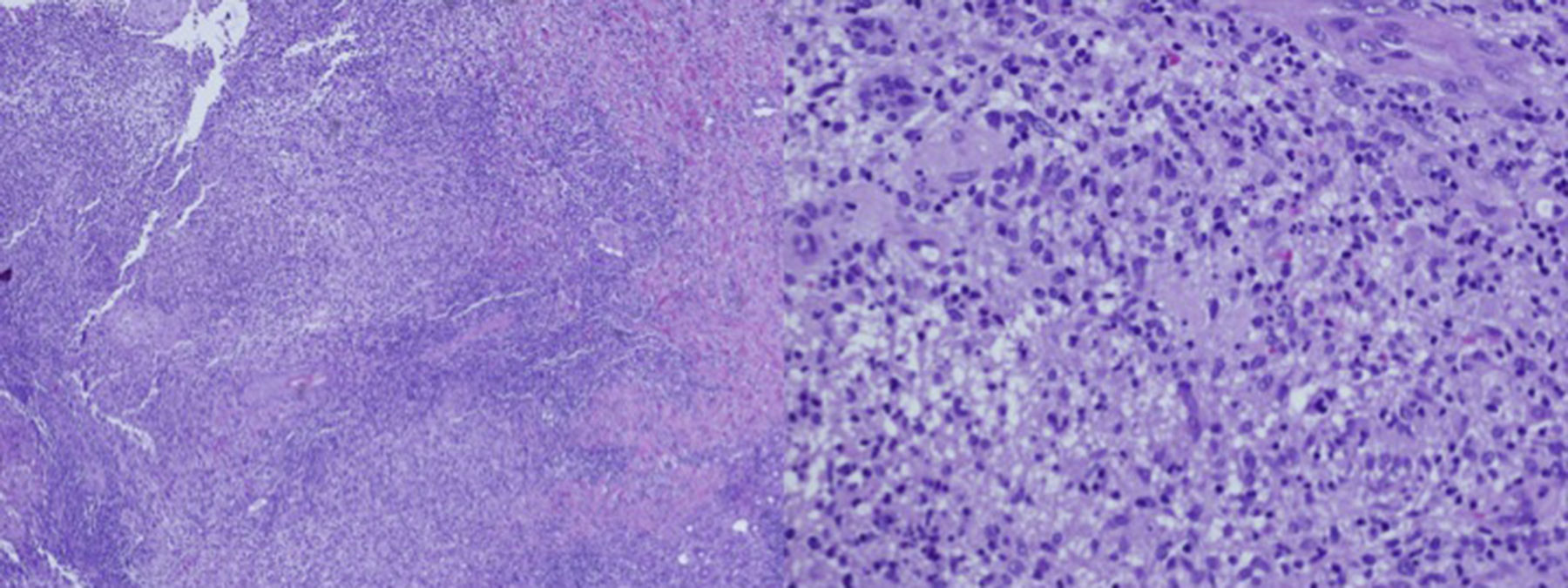
A 55-year-old male with a history of a traumatic amputation of the first three fingers on his left hand 25 years ago. Two years ago, two verrucous lesions appeared on the back of that hand which were treated with cryotherapy. The lesions did not fully resolve and slowly grew, developing into an ulcer draining purulent material. Biopsies and cultures were performed which were inconclusive. During this period, the patient had pneumonia which was treated with levofloxacin and a partial improvement of the hand lesion was observed. In the physical exam, a crusty, erythematous plaque was observed which was draining localised purulent material on the back on the left hand (Fig. 1). In the directed interview, the patient reported having an aquarium at home. With this new piece of information, a biopsy was performed for culture and pathology examination. The histological study showed a chronic, suppurative granulomatous dermatitis, compatible with an infectious aetiology. The Ziehl–Neelsen, Periodic acid–Schiff, and Grocott staining on the histology slices did not detect the presence of fungi, bacteria or acid/alcohol-fast bacilli colonies (Fig. 2).
Clinical courseDue to the patient's history of having been in contact with an aquarium, a Mycobacterium marinum infection was suspected and a mycobacteriological culture was ordered in which M. marinum colonies developed, confirming the diagnosis.
It was observed that the microorganism was sensitive to trimethoprim–sulfamethoxazole on the antibiogram. Since it is an infection limited to the skin and not disseminated, it was decided to initiate trimethoprim–sulfamethoxazole treatment in monotherapy with 800mg every 12h. After 2 months of treatment, it was observed that the lesions had improved, therefore it was decided to continue with this treatment and the lesions resolved after 4 months. This treatment regimen was continued for 2 more months, until 6 months were completed, as is recommended.
Final commentaryThe mycobacteria M. marinum grows slowly1 and commonly infects fish and amphibians.2 In humans, it causes skin and soft tissue infections. The main predisposing factor for this infection is exposure to aquatic or marine environments, therefore it is also known as “recreational water illness”. Moreover, skin wounds, local or systemic steroid treatment, treatment with immunosuppressants and lung diseases are predisposing factors for this infection.3
The lesions generally develop 1–4 weeks after an injury by handling objects used in aquatic or marine environments, or after a fish bite. In 95% of cases, the lesion is located on the upper limb. Clinically, it manifests as nodular lesions in two-thirds of cases, and with a sporotrichoid patterns in one third, showing multiple nodules along the lymphatic vessels.4 The infection can be cutaneous, subcutaneous or deep (tenosynovitis, arthritis and osteomyelitis).5,6 It can even become disseminated in immunosuppressed patients.
Two thirds of cases are diagnosed by mycobacterial culture at a temperature between 30 and 33°C7,8 in the usual culture media for mycobacteria, with a growth time of 2–6 weeks. Histological testing is non-specific, with a chronic, granulomatous and inflammatory reaction observed.
There is no established standard treatment, but responses to treatment have been described with azithromycin, amikacin, trimethoprim–sulfamethoxazole, linezolid, doxycycline, minocycline, levofloxacin and clarithromycin9 in combination with rifampicin or ethambutol. This combination is the most recommended for treatment, but if the disease is minimal, it can be treatment in monotherapy. It is recommended to complete two additional months of treatment after the lesions resolve. We present the case of a patient with M. marinum infection with a good response to treatment with trimethoprim–sulfamethoxazole in monotherapy.
We can conclude that in a patient with a chronic skin lesion, if there is a history of injury or immunosuppression and exposure to aquatic environments, it is important to suspect this infection and indicate specific cultures for M. marinum, since delaying the diagnosis and start of treatment is associated with a worse prognosis.10 As preventive measures, the use of waterproof gloves when handling fish tanks is advised if the patient has open or chronic skin wounds.
Conflicts of interestThe authors declare that there are no conflicts of interest.
Please cite this article as: Bernad I, Berroa F, Gil MP. Infección crónica en la mano. Enferm Infecc Microbiol Clin. 2017;35:125–126.