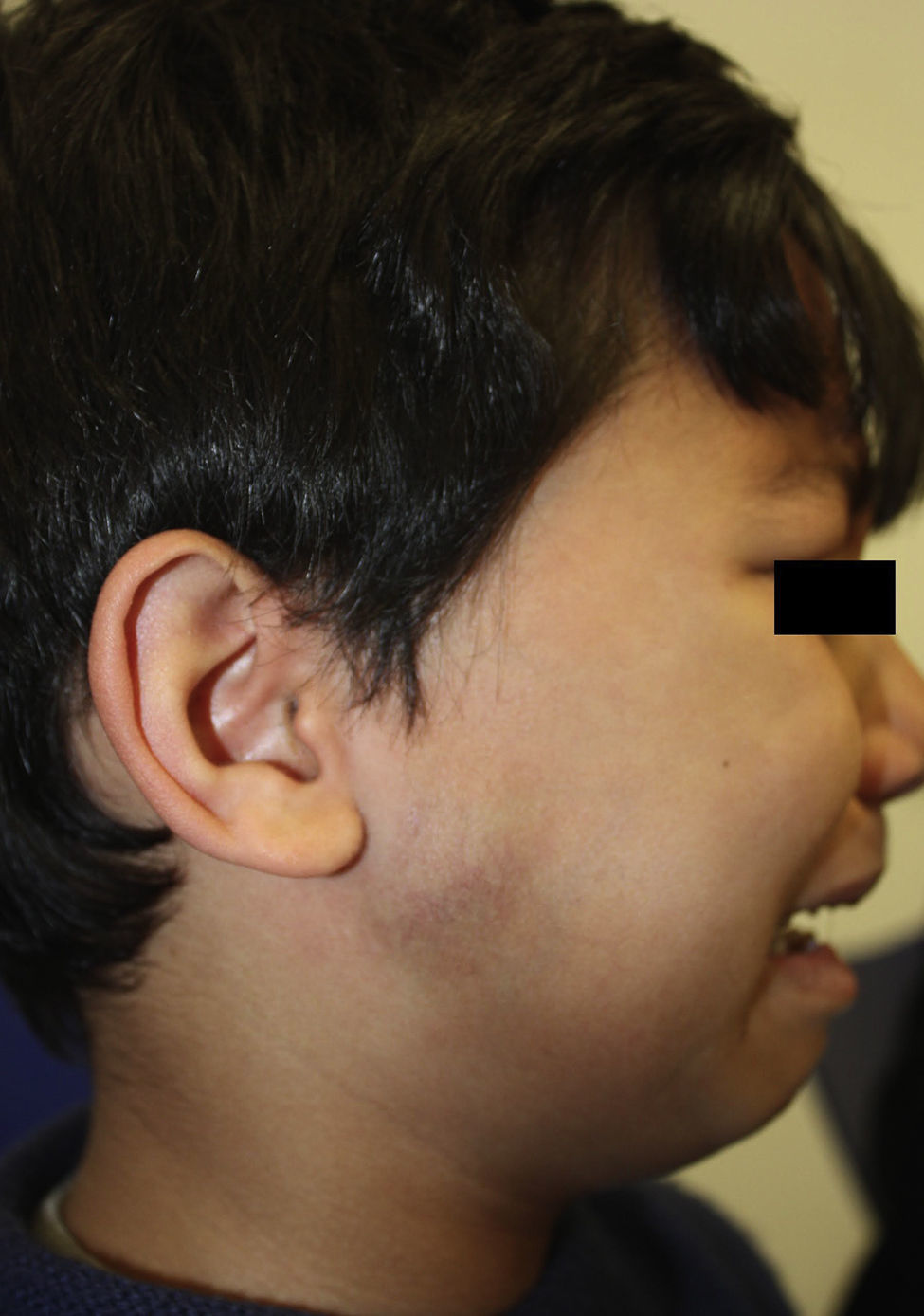
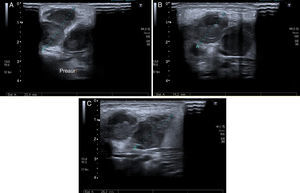
A 7-year-old male residing in Tenerife, who reported no recent trips, was seen for symptoms starting 3–4 weeks prior, with the onset of conjunctivitis of the right eye. He was treated locally with eye drops (gentamicin, dexamethasone and tetryzoline) and, given his poor progression, with eye ointment (oxytetracycline and hydrocortisone). Afterwards he presented a hard, tender, slightly erythematous, ipsilateral, preauricular swelling that was not attached to the deep planes (Fig. 1) with satellite adenopathies. The ultrasound of the laterocervical region showed a diffuse increase in the right parotid gland, multiple adenopathies with an abscessed appearance and oedema of the adjacent tissues. (Fig. 2). It was drained using ultrasound-guided FNA, and the bacteria and mycobacteria aspirate cultures, as well as the blood cultures, were negative. Serological analysis was also performed against: Toxoplasma spp., Epstein–Barr virus, cytomegalovirus, parvovirus, Brucella spp., Coxiella spp., Chlamydia pneumoniae, Borrelia burgdorferi and Bartonella henselae (B. henselae). The serology for B. henselae was positive for both IgM and IgG (titre 1/256) using indirect immunofluorescence, showing a serological profile compatible with acute infection.
Clinical courseThe patient received symptomatic treatment, as well as amoxicillin/clavulanic acid (100/12.5mg: 6.2ml/8h) and clindamycin (150mg/8h) for 4 weeks with complete remission (Fig. 3). During a second interview, we were told that he has 2 cats with which he plays regularly and he did not remember any insect or spider bits.
CommentsCat-scratch disease (CSD) is caused by B. henselae and follows a seasonal pattern, being at its most prevalent in autumn and winter.1 It has a cosmopolitan distribution although the seroprevalence in the general population differs from one country to another. In Spain in particular, different rates are observed between Communities: 8.7% in Catalonia2 and 24.7% in Seville.3 One of the most common atypical manifestations of this disease is Parinaud's oculoglandular syndrome (POS), which occurs in 5–10% of cases and presents with unilateral palpebral, non-suppurative conjunctivitis with a local granulomatous reaction associated with regional lymphadenopathy which affects the preauricular and/or submandibular lymph nodes. The conjunctival lesion can involve both the palpebral and bulbar surface, and ulceration and necrosis is common.4,5 The typical symptoms include conjunctival hyperaemia, foreign body sensation, palpebral oedema, epiphora and aqueous secretion.5
It is postulated that the route of transmission in POS patients occurs by conjunctiva contamination from the infected faeces of the flea Ctenocephalides felis4 after direct inoculation or after rubbing the eyes with contaminated hands.6 Other possible causative infectious agents for this syndrome include: Francisella tularensis, Mycobacterium tuberculosis, Treponema pallidum, Sporothrix spp. and Chlamydia trachomatis.4 Microbiological diagnosis is determined mainly through serological determinations based on indirect immunofluorescence. IgG 1/64 is the diagnostic cut-off point for patients with CSD and 1/800 for endocarditis cases. However, cross-reactions with other species are possible (Chlamydia, Coxiella burnetii). Real-time PCR has higher specificity, and it is especially useful in patients with Bartonella spp.-induced endocarditis in whom only a serum sample is available.7
Most cases of CSD resolve spontaneously, although the current recommended treatment is weight-adjusted azithromycin for 5 days. The alternative in complicated cases would be a combination of doxycycline plus rifampicin for a minimum of 4 weeks.8 Recently, cases have also been described of liver abscesses treated simply with 5 doses of azithromycin (500mg/24h for 5 days).9
We believe that the presented case corresponds to a self-limited process, who received unsuitable prolonged antibiotic treatment and who actually improved after draining the abscess and NSAID treatment. It shows the importance of taking a good clinical history that enables bartonellosis to be suspected in people who live with cats, although in this case, the child claimed not to have been scratched.
The manifestations of “cat-scratch disease” may be atypical, and we believe that preventive measures should be insisted upon such as hand washing and eradicating ectoparasites in pets.10
Please cite this article as: Hernández-Porto M, Sánchez Burgos R, Martínez de las Heras B, Rodriguez Luis JC. Conjuntivitis palpebral y adenopatía preauricular: síndrome oculoglandular de Parinaud. Enferm Infecc Microbiol Clin. 2017;35:122–124.