Mainly due to the high percentage of infection and the ineffectiveness of treatments, Helicobacter pylori is a global health problem. Knowing the age at acquisition is key to preventing the infection.
PatientsSixty-seven mothers and their respective children participated. To evaluate the presence of H. pylori, the faeces of the mother and her child were analysed using the HpSA antigen test.
Results71.6% (48/67) of pregnant mothers were positive for H. pylori at the term of their pregnancy. In newborns, 8.96% (6/67) of them showed H. pylori colonisation/persistent infection. During the first month of life, a prevalence and incidence of infection of 23.9% and 13%, respectively, was observed.
ConclusionOverall, the results suggest that there is a high risk of H. pylori infection during the first month of life, even of the persistent type.
Helicobacter pylori constituye un problema de salud mundial principalmente por el elevado porcentaje de infección y la ineficacia en los tratamientos. Para prevenir la infección resulta clave conocer la edad de adquisición.
PacientesParticiparon 67 madres y sus respectivos hijos. Para evaluar la presencia de H. pylori, las deposiciones de la madre y de su hijo fueron analizadas mediante test HpSA.
ResultadosEl 71,6% (48/67) de las embarazadas a término fueron H. pylori positivas. En los recién nacidos, el 8,96% (6/67) de ellos presentaron colonización/infección persistente para H. pylori. Durante el primer mes de vida se observó una prevalencia e incidencia de infección del 23,9 y 13%, respectivamente.
ConclusiónLos resultados, en conjunto, sugieren que durante el primer mes de vida existe un alto riesgo de infección por H. pylori, pudiendo ser esta incluso de tipo persistente.
Helicobacter pylori is a gram-negative, microaerophilic bacterium that colonises and infects the human gastric epithelium.1 The most accepted route of transmission is from person to person through oral–oral and faecal–oral contact.2 It is acquired mainly during childhood.3 It is a pathogen which is highly adapted to live in the human gastric environment, colonising around 50% of the world population.4 In all infected individuals without treatment, it causes active chronic gastritis, progressing in 10% of them to peptic ulcer, in 1–3% to gastric cancer and in 0.1% to mucosa-associated lymphoid tissue lymphoma (MALT lymphoma).5 The high rates of antibiotic resistance that it presents6 have made this pathogen a high priority for the development of new antibiotics,7 denoting the difficulty of establishing effective treatments. In order to treat the infection in a timely manner, an accurate diagnosis that is appropriate to the type of patient is necessary. In this sense, the diagnosis of H. pylori infection can be performed by methods such as serology (IgG and IgA), measurement of urease activity in exhaled air and detection of H. pylori antigens in stools (HpSA),8 but only the latter is appropriate in infants.
The objective of this paper is to determine the dynamics of colonisation/infection by H. pylori presented by infants during the first six months of life. To do this, the infection was evaluated in both the full-term mother and her newborn child.
MethodologyTarget populationA total of 67 mothers and their respective children participated in the study. Mothers interested in participating were given the survey and informed consent. The survey considered: sex of the newborn, type of delivery, type of lactation and access to drinking water. Infants of both sexes, who were healthy and delivered between October 2008 and January 2009 in the Hospital Higueras de Talcahuano, Biobío Region, Chile, were included.
This study was approved by the Ethics Committee of the Faculty of Medicine of the Universidad de Concepción and by the Ethics Committee of the Los Cerros Family Health Centre (CESFAM), Talcahuano commune, Biobío Region, Chile.
Inclusion criteria: healthy and full-term pregnancy, healthy newborn and signing of informed consent by the mother.
Exclusion criteria for mothers: psychiatric disorder, illiteracy and treatment with antibiotics during the last three months of pregnancy.
Exclusion criteria for newborns: preterm pregnancy, hospitalised newborn and treatment with antibiotics.
Helicobacter pylori stool antigen (HpSA) testThe HpSA ELISA test (Premier Platinum Helicobacter pylori stool antigen, Meridian Diagnostics, Ohio, USA) was performed according to the manufacturer's instructions. The test was carried out in duplicate in the stool sample prior to delivery in the mothers, and in their children at seven days, one month and six months of age. The results were measured spectrophotometrically; the value to consider a sample positive was ≥0.140 (450nm) and a 450/630nm ratio ≥0.100 optical density. The HpSA ELISA test has a sensitivity and specificity of 94% in both cases.8
Criterion of prevalence and incidenceThe prevalence and incidence calculation was performed according to the criteria of the Pan American Health Organisation.9
Criterion of colonisation/transient and persistent infection due to Helicobacter pyloriThe HpSA test does not differentiate between colonisation and infection, so the term “colonisation/infection” was used, as defined by O’Ryan et al. (2013).10 It was defined as transient if one or two samples were positive; as persistent if three consecutive samples were positive, and as indeterminate if one sample was positive only in the last sample.
ResultsDetection of Helicobacter pylori in pregnant mothers at full termOf the total of 67 pregnant mothers at full term, 48 were positive for H. pylori and 19 were negative for the pathogen, which corresponds to 71.6 and 28.4%, respectively (data not shown).
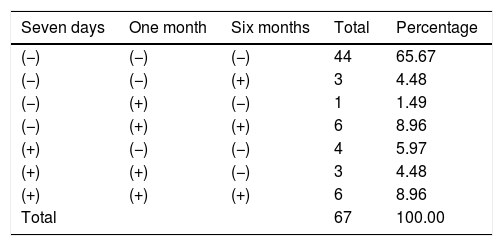
Follow-up of Helicobacter pylori in infantsEpidemiological follow-up of H. pylori infection in newborns is shown in Table 1. These results were ordered according to the number and time of negativity or positivity for H. pylori, i.e. children negative to the pathogen, those positive in one, two and three samples (persistent infection). The results show that the presence of H. pylori was not detected in 65.67% of children. Regarding infected children, 20.89% were positive in one or two samples (transient infection) and 4.47% were positive only at the last sampling (indeterminate infection). 8.96% of children were found to be positive for the three samples, which is a persistent infection (Table 1).
Monitoring the infective status of Helicobacter pylori in newborns using the HpSA test.
| Seven days | One month | Six months | Total | Percentage |
|---|---|---|---|---|
| (−) | (−) | (−) | 44 | 65.67 |
| (−) | (−) | (+) | 3 | 4.48 |
| (−) | (+) | (−) | 1 | 1.49 |
| (−) | (+) | (+) | 6 | 8.96 |
| (+) | (−) | (−) | 4 | 5.97 |
| (+) | (+) | (−) | 3 | 4.48 |
| (+) | (+) | (+) | 6 | 8.96 |
| Total | 67 | 100.00 |
(−): negative sample; (+): positive sample.
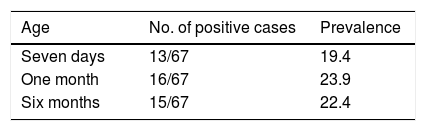
At seven days from birth, 13 out of 67 children were positive for H. pylori, which corresponds to an initial prevalence of 19.4%, increasing to 23.9% after one month and finally falling to 22.4% at the sixth month of life (Table 2). From the initial prevalence of infection, the number of new cases during two periods was counted. Between seven days and the first month of life, seven new cases of infection were observed, which corresponds to an incidence of 13%. On the other hand, between the first and sixth months of life, three new cases were registered, which corresponds to an incidence of 6.4% (data not shown).
DiscussionThe diagnostic method to detect H. pylori both in mothers and their children is a non-invasive, low-cost technique with acceptable diagnostic accuracy. However, care must be taken to keep the samples at refrigeration or freezing temperatures, and accuracy may decrease when the sample is not uniform or is very diluted.8
In this research, an infection prevalence of 71.6% was observed in pregnant women at full term, a percentage higher than the overall rate of infection reported for this group, which varies from 46 to 56.7%.4 It has been established that the main risk factor for infection and/or acquisition of H. pylori in children is the mother.11 However, this statement is controversial, because several studies establish that the infection of the mother does not represent a preponderant risk factor to acquire the infection.10,12 In this sense, infected parents and siblings seem to play an important role in the contagion of children.11,13
O’Ryan et al. in 201310 and 20153 reported cases of persistent infection in about 20% of the cohort of newborns, which was acquired between 9 and 24 months, indicating this period as that in which the infection was acquired. However, our results suggest that this type of infection could be acquired before seven days of age, since 9% of children who had this condition did so almost from birth. Persistent H. pylori infection in children has been associated with high bacterial load, virulent genotype and non-secretory phenotype, characterised by increased adherence of H. pylori.3
The fact that children younger than six months investigated in this study have high levels of H. pylori infection is a matter for concern, since infection in infants has been linked to serious pathologies such as bronchial asthma, growth retardation,14 and even sudden infant death syndrome.15 The lack of detection and eradication in the infected family members of the infant, added to the impossibility of treatment in them except strict indications, make it difficult to break the chain of infection. However, the use of individual toothbrushes for each person, not placing materials belonging to infants in the mouth, the frequent washing of hands and the prophylactic use of probiotic strains have proven to be effective measures to prevent H. pylori infection.14
In this study, high levels of infection were observed in both mothers and their newborns. In the latter, the highest prevalence and incidence of colonisation/infection were observed during the first month of life, and this type may be persistent. The results as a whole suggest that during the first month of life there is a high risk of contracting H. pylori. These results can be considered to promote public policies about diagnosis, surveillance and preventive measures of H. pylori infection, both in the pregnant mother and her newborn and in their family environment.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: Merino JS, Araneda L, Lincoñir-Campos P, Parra C, Sáez K, García A. Dinámica de la infección por Helicobacter pylori en lactantes durante los primeros 6 meses de vida. Enferm Infecc Microbiol Clin. 2019;37:109–111.