Non-invasive fungal rhinosinusitis is a clinical condition with a variable inflammatory response which usually affects immunocompetent patients. This condition typically involves the occupation of multiple sinuses by mucoid material containing fungal hyphae. The main aetiological agents are dematiaceous fungi and Aspergillus spp., particularly A. flavus.1
We describe the case of a 46-year-old immunocompetent woman whose only relevant medical history was endoscopic sinus surgery two and a half years previously for central facial pain, in which mucoid material occupying the left sphenoid sinus was aspirated. Some 22 months after the procedure, the patient reported persistence of the pain, in addition to hyposmia and difficulty breathing through her nose. A CT scan showed complete expansive occupation of the left sphenoid sinus with posterior wall bone erosion and complete occupation of the maxillary sinus, ethmoid cells and frontal sinus on the left side, with underlying polyp. Six months later the patient had repeat endoscopic nasal-sinus surgery, with removal of purulent material from the left maxillary, sphenoid and ethmoid sinuses, which was sent to pathology and microbiology for testing.
Pathology reported mucoid material rich in eosinophils and the presence of septate hyphae.
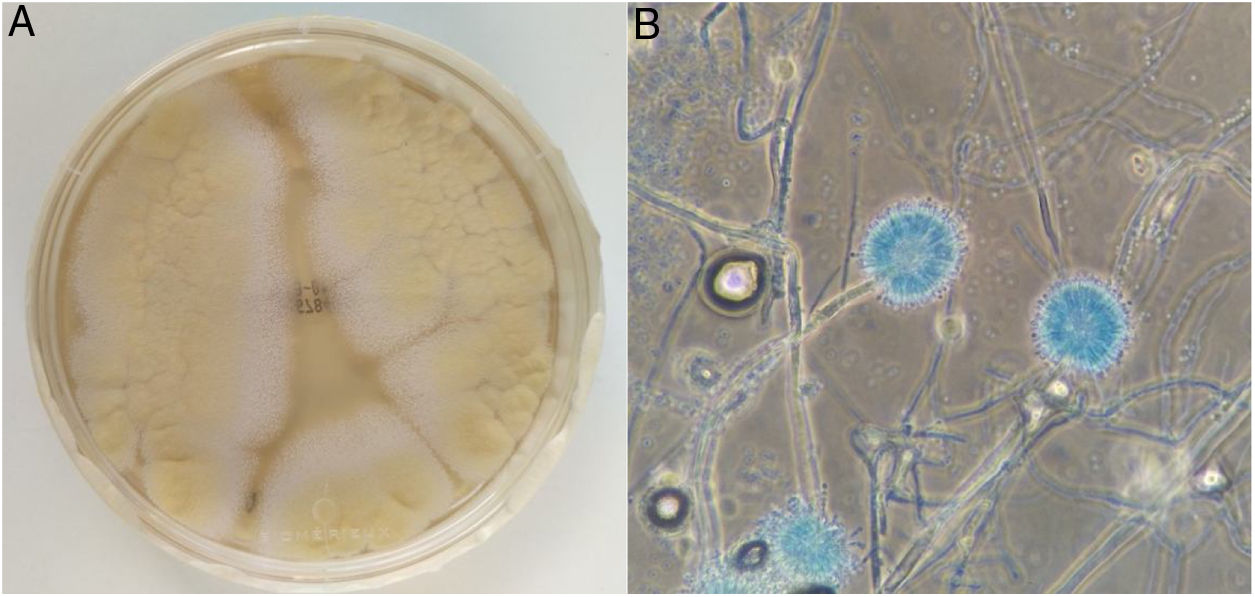
Microbiology received three samples of pus drained from the left maxillary, sphenoid and ethmoid sinuses, which were seeded in Sabouraud-chloramphenicol agar (bioMerièux) culture media and incubated at 37°C and 30°C. After 72h of incubation, several 4-cm colonies with a yellowish centre and white periphery had grown in the three cultures incubated at 30°C (Fig. 1A). Microscopic examination revealed radiate, biseriate conidial heads (Fig. 1B).
Initially, the identification was carried out using MALDI-TOF mass spectrometry (Bruker Daltonics), obtaining a score of 1.8 for Aspergillus ochraceus. To confirm this result, the β-tubulin gene was amplified with conventional PCR, which can discriminate between species of Aspergillus,2,3 and with its subsequent sequencing Aspergillus melleus was definitively identified with 100 % similarity to the sequence deposited in GeneBank® (FJ491523.1).
The patient was discharged home after surgery. She was prescribed antibiotic treatment (amoxicillin-clavulanic acid 875mg/125mg every 8h for 7 days) and nasal lavage with normal saline followed by inhalations of mometasone furoate in each nostril. Four months later, she had made a good recovery.
Aspergillus melleus belongs to the subgenus Circumdati, section Circumdati and the group Aspergillus ochraceus.2,4 It is a fungus of ubiquitous distribution, found in soil, plantations or food,5 and has the ability to produce proteolytic enzymes6 and insecticidal compounds.7 Like other species in the group, it can also produce ochratoxin, although in small quantities.4 To our knowledge, A. melleus has only been described as a human pathogen in certain cases of onychomycosis,8,9 so the case we describe would be the first case of fungal rhinosinusitis due to A. melleus and the first infection other than an onychomycosis caused by this microorganism.
In terms of therapeutic management, the fact that it was a non-invasive condition in an immunocompetent patient meant that the use of systemic antifungals was not necessary10; the main treatment being the drainage of the mucous material occupying the sinus cavities. Despite this being an immunocompetent patient with no risk factors for an Aspergillus spp. infection, the anatomical alteration of her nasal sinuses in conjunction with the previous surgery may have played a significant role in the infection and proliferation of the fungus.
By way of conclusion, we would like to emphasise on the one hand the importance of nucleic acid amplification techniques to precisely identify the species of the Aspergillus genus, and on the other, to raise the possibility that A. melleus cases are underdiagnosed. This is primarily due to their low severity, which means that very often only empirical treatment is considered necessary and microbiological diagnosis is not requested. Another reason is the difficulty in establishing a definitive diagnosis with techniques other than nucleic acid amplification, such as microscopy or MALDI-TOF, which are much more widely available in microbiology laboratories.
To Carmen Vera González and Rosaura Pérez Muñoz.
Please cite this article as: Carretero-Vicario O, Fradejas I, Meana I, Perez-Ayala A. Primer caso de rinosinusitis fúngica no invasiva por Aspergillus melleus. Enferm Infecc Microbiol Clin. 2020;38:92–93.