Contact with the healthcare system by a sample of seropositive men who have sex with men (MSM) prior to their HIV diagnosis are analysed, and missed opportunities (MO) for an earlier HIV diagnosis are identified.
MethodologyBetween 2012 and 2013, an online survey was conducted among HIV-positive MSM, mainly recruited from gay websites. Those who were diagnosed with HIV between 2010 and 2013 were analysed. MO were defined as episodes prior to the HIV diagnosis in which the healthcare system was contacted due to an indicator condition of HIV infection and the test was not suggested. The proportion of missed opportunities was compared according to the type of indicator condition, the department consulted and the healthcare professional's knowledge that the patient was MSM.
ResultsOverall, 639 participants (66% of 966) reported 1145 episodes with some indicator condition, the majority of these being identified in primary care (n=527; 46%). The highest percentage of MOs is also observed in primary care (63%). Although the indicator condition with the highest number of MOs was STIs (n=124), the highest percentage of MOs was observed in consultations due to diarrhoea with no known cause (69.8%). The percentage of MOs when the doctor knew that the patient was MSM was 40 vs. 70% when the doctor did not know.
ConclusionThe majority of HIV-positive MSM analysed in this study went to healthcare services for HIV-infection indicator conditions prior to their HIV diagnosis. Primary care was the most-frequently-visited department and is also where the most opportunities were missed to perform an HIV test, even when it was known that the patient was a MSM.
Analizar los contactos con el sistema sanitario de una muestra de hombres seropositivos que tienen relaciones sexuales con otros hombres (HSH) sucedidos con anterioridad a su diagnóstico de infección por VIH e identificar posibles oportunidades perdidas (OP) de haber adelantado su diagnóstico.
MétodosEntre 2012–2013 se realizó una encuesta online a HSH infectados por el VIH que fueron seleccionados, fundamentalmente, en páginas de contacto gays. Se analizaron los diagnosticados de infección por VIH en el periodo 2010-2013. Se consideró OP a los episodios previos al diagnóstico en los que se contactó con el sistema sanitario por alguna condición indicadora de infección por VIH y no se propuso la prueba. Se compararon las proporciones de OP según el tipo de condición indicadora, el servicio consultado y el conocimiento del profesional de que el paciente atendido era HSH.
ResultadosEn total, 639 participantes (66% de 966) refirieron 1.145 episodios con alguna condición indicadora, identificándose la mayoría en atención primaria (n=527; 46%). También es en este servicio donde se observó la mayor proporción de OP (63%). Aunque las ITS fue la condición indicadora con mayor número de OP (n=124), el mayor porcentaje de OP se observó en las consultas por diarreas sin causa clara (69,8%). El porcentaje de OP cuando el médico conocía que el paciente era HSH se elevó al 40% frente al 70% cuando lo desconocía.
ConclusiónLa mayoría de los HSH positivos para el VIH acudió a los servicios sanitarios antes de su diagnóstico por condiciones indicadoras de infección por VIH. Atención primaria fue el servicio más visitado y también donde se estarían perdiendo más oportunidades para indicar la prueba de VIH, incluso sabiendo que el paciente es HSH.
In Spain, HIV transmission between men who have sex with men (MSM) accounts for 53.6% of new diagnoses.1 This means that sex between men is the most common route of transmission of the virus. Although MSM comprise the most commonly tested group,2,3 38.4% of MSM diagnosed with HIV in 2015 had a late diagnosis (i.e. had a CD4 count below 350cells/μl at the time of HIV diagnosis). In countries with an epidemic similar to the one in Spain, it has been estimated that between 20%4 and 44%5 of MSM are undiagnosed.
Lack of diagnosis and late diagnosis of HIV are associated with greater morbidity and mortality, increased healthcare expenditure and a higher risk of HIV transmission.6,7 Hence, reducing the undiagnosed proportion of the epidemic and therefore late diagnosis is a priority in the fight against HIV. To this end, MSM are advised to undergo HIV testing at least once per year.8,9 Every missed opportunity for HIV testing could amount to an unacceptable contribution to the spread and persistence of the infection.
To improve coverage and reduce time to diagnosis, many countries, including Spain,7 have implemented various strategies.8,9 One such strategy is indicator condition-based testing grounded in the recommendations issued by the HIV in Europe (HIE) platform in 2012.10 This initiative proposes systematic HIV testing in patients who are assessed for a number of indicator conditions, which have a prevalence of HIV infection estimated at, or which can be expected to exceed, 0.1%,8,11,12 therefore rendering HIV infection screening cost-effective.13–15
Some studies have shown that missed opportunities in the healthcare system to advance the diagnosis of HIV are occurring.16,17 In Spain there are few studies on this subject. A population study conducted in Catalonia reported that HIV testing is not being performed in nearly 80% of diagnoses related to indicator conditions.6 However, this study focused on a single healthcare context (primary care) and did not offer disaggregated data for the MSM group. Another study, conducted in a hospital setting, reported a much lower percentage of missed opportunities (14.5%). However, it too did not offer figures for missed opportunities for the MSM group.7
Even though most new diagnoses are made in MSM,1 the relationship between awareness on the part of the healthcare professional that the patient is an MSM and suitable application of the recommendations for HIV prevention has scarcely been studied.18
The aim of this study was to offer an overview to better understand the types of healthcare department and the conditions in which missed opportunities are occurring in a substantial sample of MSM diagnosed with HIV infection in Spain. To this end, the percentage of contacts with the healthcare system related to HIV infection indicator conditions in which the healthcare professional did not propose HIV testing was estimated. Differences were analysed based on type of indicator condition, department visited and whether the professional responsible for offering HIV testing knew that the patient was an MSM.
MethodologyProcess and participants in the studyAn online cross-sectional study that enrolled HIV-infected MSM was conducted between September 2012 and April 2013. For the purposes of the study, the main commercial websites in Spain for gay contact; lesbian, gay, bisexual and transgender (LGBT) defence; and the fight against HIV, as well as other websites with information specific to this group or related to HIV infection, were identified. Participants were recruited through banners appearing on websites and emails delivered to the distribution lists of the cooperating sites. The set fee for each commercial website had to be paid in order to reach more potential study participants. Participation in the study was not remunerated.
When an individual clicked on the banner or the link included in the emails, he accessed a screen presenting the study which contained the informed consent form for voluntary participation. This form assured the individual of the anonymity and confidentiality of the information.
The subjects included in this analysis were men ≥18 years of age who were residents of Spain and reported having sex with other men and having been diagnosed with HIV infection in Spain between 2010 and 2013. The study was approved by the Instituto de Salud Carlos III Ethics Committee (CEI PI 70_2015).
Data collection toolThe questionnaire included several blocks of questions about sociodemographic characteristics, sexual behaviour and aspects concerning the time of HIV diagnosis.
To assess missed opportunities before HIV diagnosis, the participants were asked whether they visited a physician for any of the following HIV infection indicator conditions:
- •
Sexually transmitted infection (STI).
- •
Tuberculosis.
- •
Candidiasis.
- •
Herpes zoster.
- •
Inflamed painful lymph nodes in different parts of the body.
- •
Weight loss exceeding 10%.
- •
Frequent repeated bouts of diarrhoea or diarrhoea for more than one month with no clear cause.
- •
Fever for more than one month with no clear cause.
These indicator conditions were included based on the recommendations for early HIV diagnosis both in Spain and in Europe8–10,19 and taking into account in the preparation and drafting phases that this was a self-administered questionnaire with a limited length and that most participants were unfamiliar with medical terminology.
Those who reported having been assessed for any of these conditions were asked the following questions for each condition assessed: (1) the department in which the diagnosis was made, (2) whether the physician had proposed HIV testing and (3) whether the physician knew that they were an MSM.
Participants who had no testing prior to diagnosis, as well as participants who did have such testing but reported that more than five years had elapsed between their diagnosis and their previous test, were asked to only consider contacts with the healthcare system that occurred in the five years prior to diagnosis. All other participants were asked to consider the period between their last negative test and their diagnostic test.
A “missed opportunity” was defined as an episode in which care was sought for any of the above-mentioned HIV infection indicator conditions and the physician did not propose HIV testing.
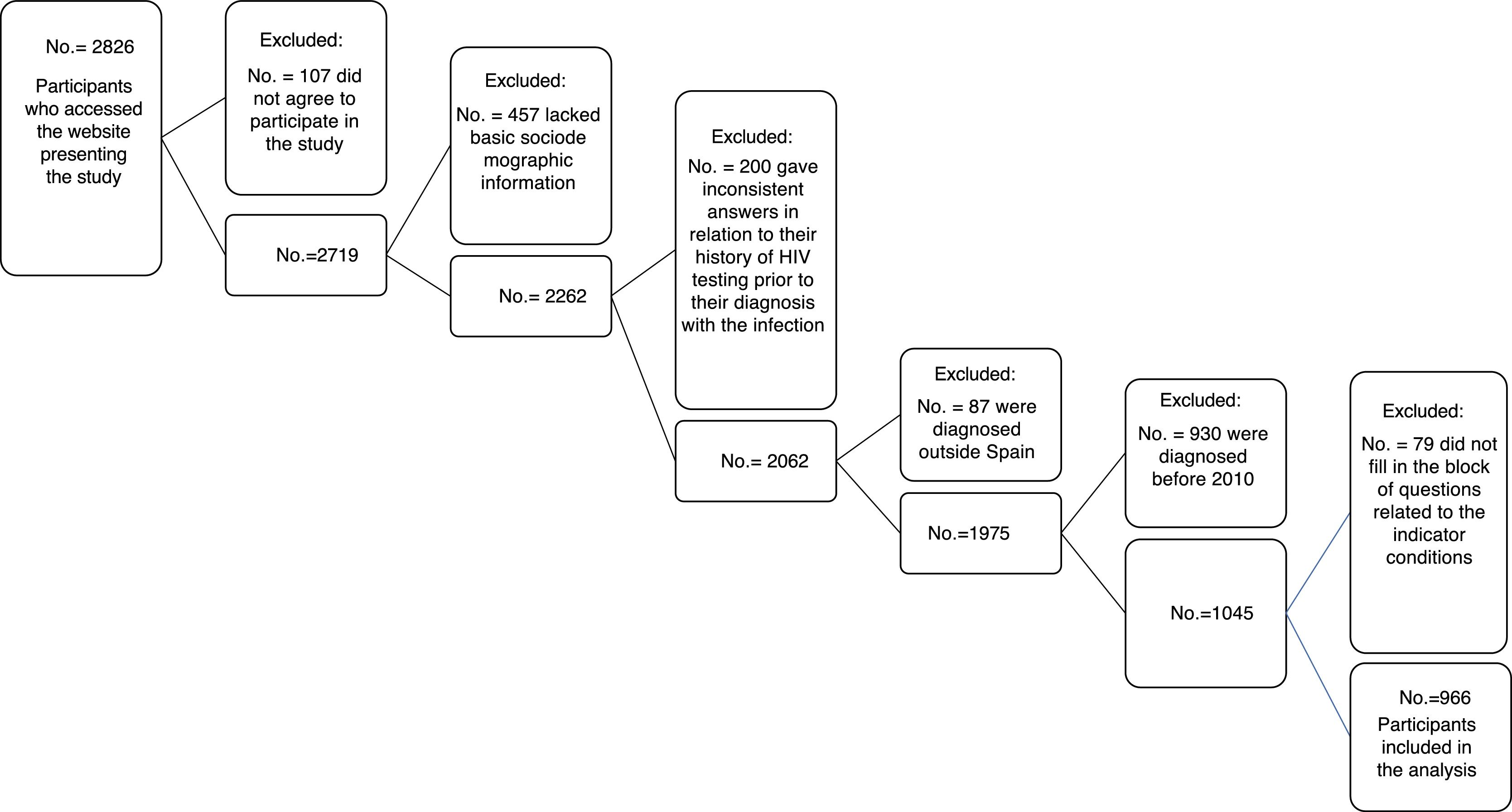
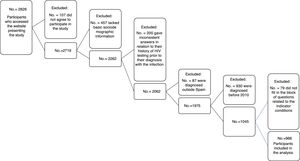
Data analysisOf the total of 2826 participants with positive serology for HIV who accessed the first screen presenting the study, 96.2% agreed to participate (n=2719). Of these, three questionnaires were excluded because the respondents said that they were women, one was excluded because the respondent had never had sex and 453 were excluded because they were virtually devoid of information — that is to say, they lacked basic information for analysis, such as age, place of birth, gender, type of sexual relations throughout life, history of HIV testing and time elapsed since last HIV test. Of the remaining 2262 questionnaires, 200 were eliminated because they had inconsistent information in relation to HIV testing prior to diagnosis. Of the 2062 MSM, those who were selected for this analysis were those who in addition had been diagnosed in Spain (n=1975) between 2010 and 2013 (n=1045) and those who had answered all questions in relation to whether they had sought care due to any HIV infection indicator condition and the associated questions (n=966) (Fig. 1).
A two-level analysis was performed. First, the main sociodemographic, behavioural and HIV diagnosis-related characteristics of these participants were reported, and the percentage of participants who were diagnosed or who sought care due to any HIV indicator condition and its corresponding 95% confidence interval (95% CI) were calculated.
As participants could specify more than one indicator condition, an analysis of episodes was then performed. The distribution of episodes was analysed based on type of healthcare department visited and type of indicator condition. Subsequently, the proportion of missed opportunities was calculated for each condition and type of healthcare department. Finally, the percentage of episodes in which healthcare professionals knew that the patient was an MSM was calculated, and missed opportunities were estimated based on this variable. Differences in proportions were analysed using the χ2 test for comparing proportions.
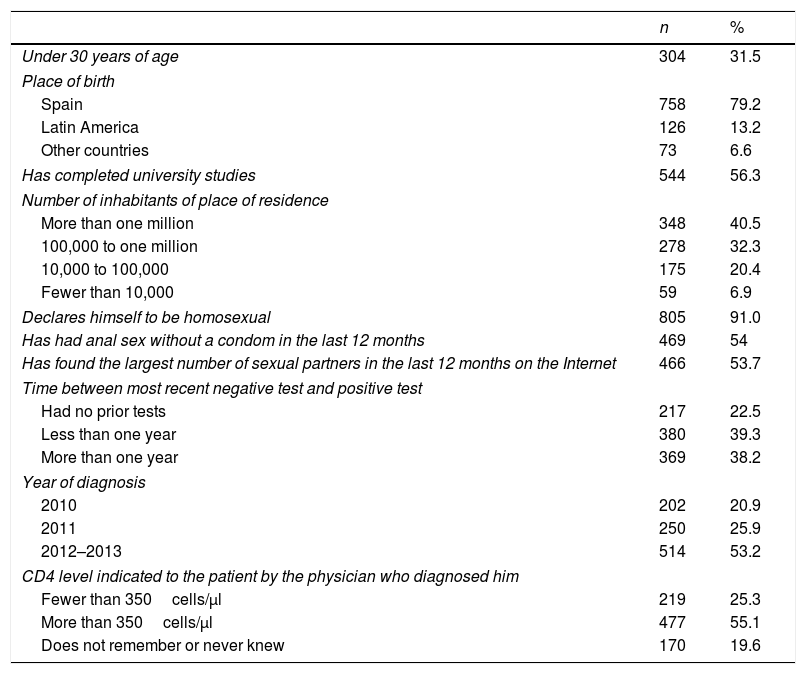
ResultsOf the 966 participants, 81.1% were recruited on gay contact websites, 31.5% were under 30 years of age, 79% were Spanish and 56.3% reported undertaking university studies. Residence in a city of more than one million inhabitants was reported by 40.5% whereas residence in a town or city with less than 10,000 inhabitants was reported by 7%. A total of 91% declared themselves to be homosexual.
Regarding sexual behaviour in the last 12 months, 54% reported having had anal sex without a condom, and 54% specified that they had found the largest number of sexual partners on the Internet.
Regarding questions referring to time of diagnosis, 22.5% knew that they were infected with the first HIV test that was done, and for 39.3% less than one year had elapsed from the last negative test to the diagnostic test. In total, 53% were diagnosed between 2012 and 2013, and one in four (25.3%) reported having a CD4 level below 350cells/mm3 (Table 1).
Sociodemographic, behavioural and diagnosis-related characteristics of survey respondents (No.=966).
| n | % | |
|---|---|---|
| Under 30 years of age | 304 | 31.5 |
| Place of birth | ||
| Spain | 758 | 79.2 |
| Latin America | 126 | 13.2 |
| Other countries | 73 | 6.6 |
| Has completed university studies | 544 | 56.3 |
| Number of inhabitants of place of residence | ||
| More than one million | 348 | 40.5 |
| 100,000 to one million | 278 | 32.3 |
| 10,000 to 100,000 | 175 | 20.4 |
| Fewer than 10,000 | 59 | 6.9 |
| Declares himself to be homosexual | 805 | 91.0 |
| Has had anal sex without a condom in the last 12 months | 469 | 54 |
| Has found the largest number of sexual partners in the last 12 months on the Internet | 466 | 53.7 |
| Time between most recent negative test and positive test | ||
| Had no prior tests | 217 | 22.5 |
| Less than one year | 380 | 39.3 |
| More than one year | 369 | 38.2 |
| Year of diagnosis | ||
| 2010 | 202 | 20.9 |
| 2011 | 250 | 25.9 |
| 2012–2013 | 514 | 53.2 |
| CD4 level indicated to the patient by the physician who diagnosed him | ||
| Fewer than 350cells/μl | 219 | 25.3 |
| More than 350cells/μl | 477 | 55.1 |
| Does not remember or never knew | 170 | 19.6 |
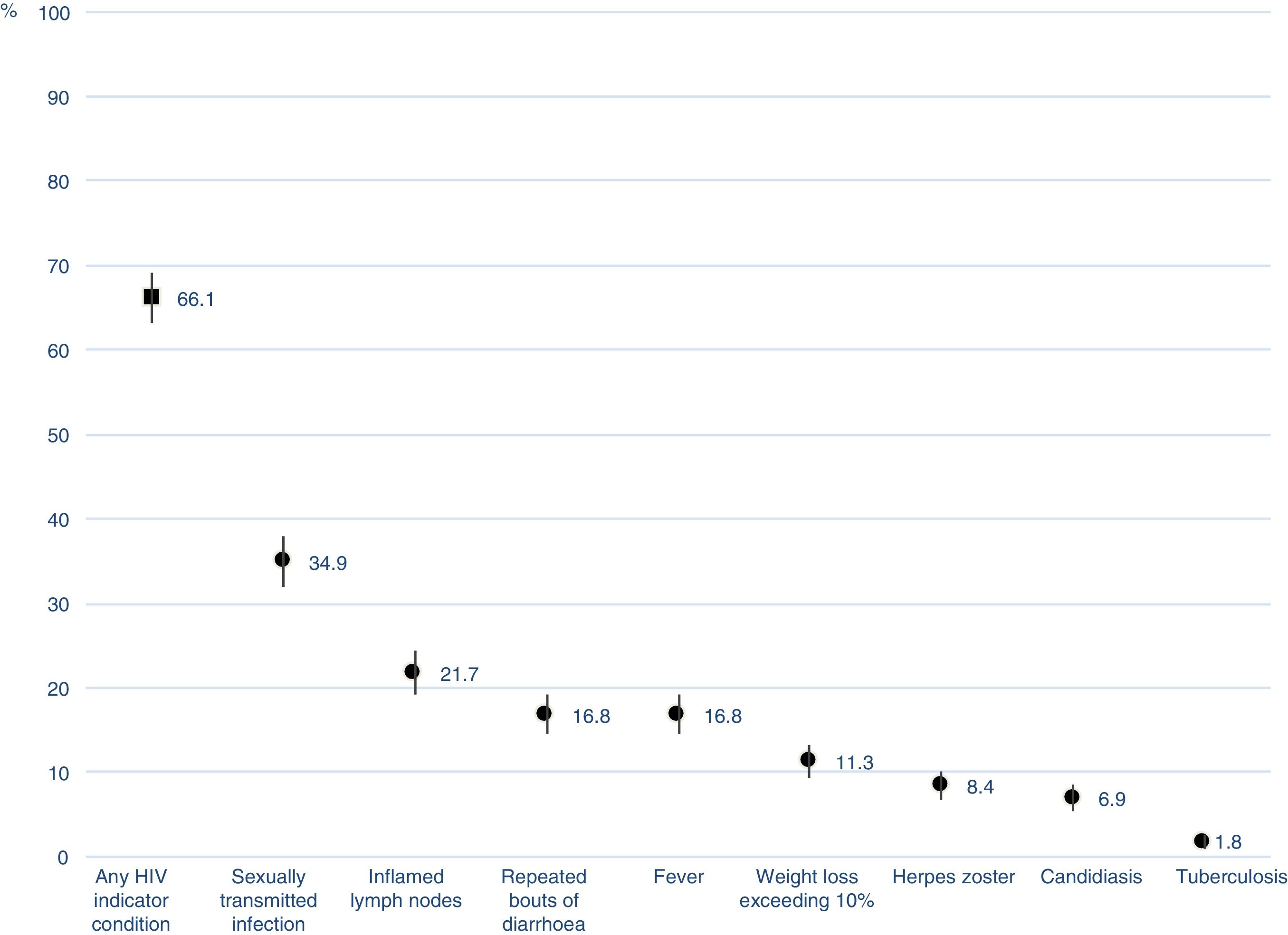
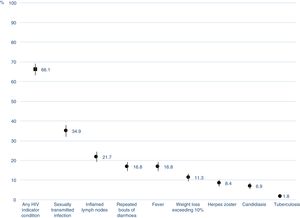
Of the individuals analysed, 66% (95% CI 63.0–69.1) reported that, before they knew that they were infected with HIV, they sought care due to symptoms or were diagnosed with an HIV indicator condition.
Indicator conditions included diagnoses of an STI, with 34.9% (95% CI 31.9–37.9), followed by inflamed painful lymph nodes in different parts of the body (21.7%; 95% CI 19.1–24.3), repeated or chronic bouts of diarrhoea (16.8%; 95% CI 14.4–19.1), fever of unknown origin (16.8%; 95% CI 14.4–19.1), herpes zoster (8.4%; 95% CI 6.6–10.1), candidiasis (6.9%; 95% CI 5.3–8.5) and tuberculosis (1.8%; 95% CI 0.9–2.6) (Fig. 2Fig. 2).
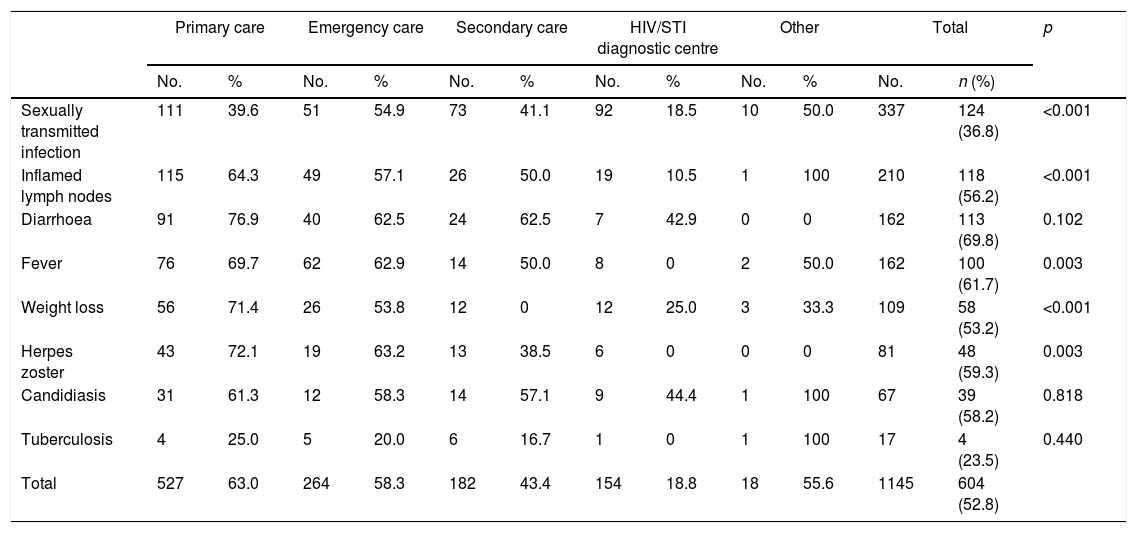
A single episode was reported by 50.7% (n=324) of participants, two conditions were reported by 28.6% (n=183), three conditions were reported by 13.6% (n=87) and more than three were reported by 7.0% (n=45). Therefore, a total of 1145 episodes were counted among the 639 participants who specified any of the conditions. As Table 2 shows, of these 1145 episodes, 604 (52.8%) represented a missed opportunity as HIV testing was not offered or performed by the healthcare professional who provided care. The three conditions that generated the largest numbers of missed opportunities were STIs (n=124), inflamed lymph nodes (n=118) and diarrhoea for more than 30 days (n=113). However, in proportion to the number of episodes, the conditions with the highest percentages of missed opportunities were diarrhoea, with 69.8% (n=113); fever, with 61.7% (n=100); and herpes zoster, with 59.3% (n=48).
Percentage of missed opportunities for HIV testing by type of healthcare department visited.
| Primary care | Emergency care | Secondary care | HIV/STI diagnostic centre | Other | Total | p | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No. | % | No. | % | No. | % | No. | % | No. | % | No. | n (%) | ||
| Sexually transmitted infection | 111 | 39.6 | 51 | 54.9 | 73 | 41.1 | 92 | 18.5 | 10 | 50.0 | 337 | 124 (36.8) | <0.001 |
| Inflamed lymph nodes | 115 | 64.3 | 49 | 57.1 | 26 | 50.0 | 19 | 10.5 | 1 | 100 | 210 | 118 (56.2) | <0.001 |
| Diarrhoea | 91 | 76.9 | 40 | 62.5 | 24 | 62.5 | 7 | 42.9 | 0 | 0 | 162 | 113 (69.8) | 0.102 |
| Fever | 76 | 69.7 | 62 | 62.9 | 14 | 50.0 | 8 | 0 | 2 | 50.0 | 162 | 100 (61.7) | 0.003 |
| Weight loss | 56 | 71.4 | 26 | 53.8 | 12 | 0 | 12 | 25.0 | 3 | 33.3 | 109 | 58 (53.2) | <0.001 |
| Herpes zoster | 43 | 72.1 | 19 | 63.2 | 13 | 38.5 | 6 | 0 | 0 | 0 | 81 | 48 (59.3) | 0.003 |
| Candidiasis | 31 | 61.3 | 12 | 58.3 | 14 | 57.1 | 9 | 44.4 | 1 | 100 | 67 | 39 (58.2) | 0.818 |
| Tuberculosis | 4 | 25.0 | 5 | 20.0 | 6 | 16.7 | 1 | 0 | 1 | 100 | 17 | 4 (23.5) | 0.440 |
| Total | 527 | 63.0 | 264 | 58.3 | 182 | 43.4 | 154 | 18.8 | 18 | 55.6 | 1145 | 604 (52.8) | |
No.: number of episodes of HIV indicator conditions; n: number of missed opportunities for HIV testing.
Table 2 also shows that primary care and emergency care were the departments that assessed the most HIV indicator conditions, accounting for 46.0% (n=527) and 23.1% (n=264), respectively, of all episodes with any HIV indicator condition. Primary care and emergency care were the departments in which the most opportunities for HIV testing were missed (63% and 58.3%, respectively), followed by secondary care (43.4%) and HIV/STI diagnostic centres (18.8%). This same order was repeated for most of the HIV indicator conditions included in the questionnaire, except for STI, where the emergency department was the department in which most opportunities for HIV testing were missed, followed by primary and secondary care to practically the same degree. This difference between departments was statistically significant (p<0.05) for most HIV indicator conditions, with the exception of diarrhoea, candidiasis and tuberculosis.
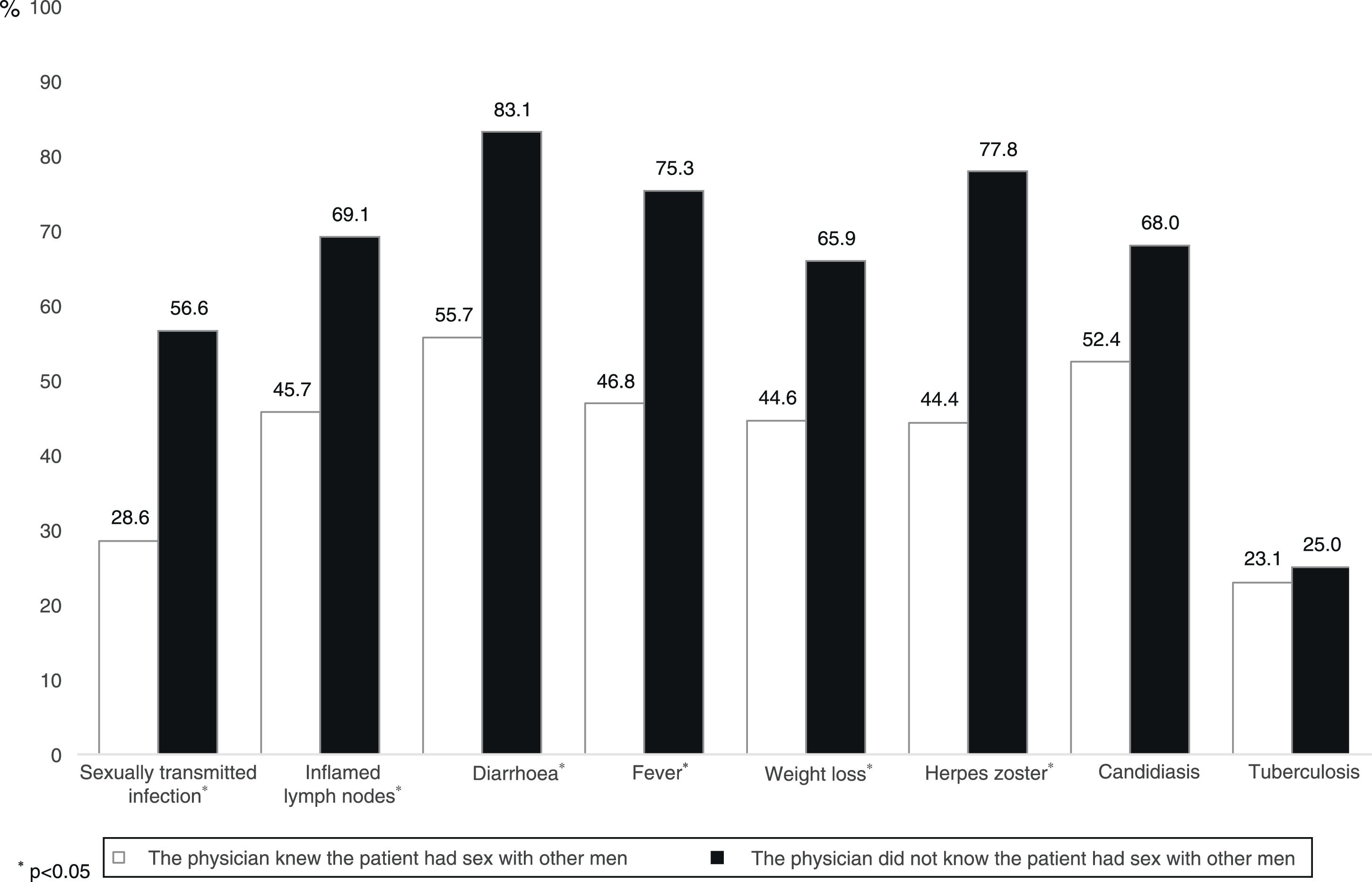
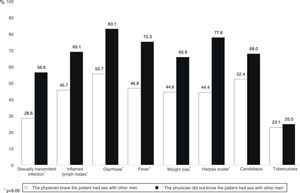
Out of all episodes with any HIV indicator condition, in 675 (58.9%) the physician knew that the patient was an MSM and in 40% of these cases did not recommend HIV testing. In episodes in which the physician did not know that the patient had homosexual relations, the proportion of missed opportunities was 70% (p<0.05). As Fig. 3 shows, this pattern was repeated in all indicator conditions, except candidiasis (p=0.21) and tuberculosis (p=0.94).
DiscussionMost HIV-positive MSM analysed in this study had contact with the healthcare system before their diagnosis due to an HIV indicator condition. However, a large number of potentially missed opportunities to advance the diagnosis occurred, since in more than half of contacts the physician did not propose HIV testing. Most of these contacts occurred in general departments such as primary care and emergency care, which is also where the highest proportion of missed opportunities was recorded.
Even though indicator condition-based testing has been previously evaluated both in Spain6 and elsewhere in the world,20–22 this study was the first to analyse the extent of missed opportunities occurring in MSM, the population most affected by HIV and accounting for nearly half of new diagnoses made each year in Spain.1 Having a large enough sample size enabled us to identify the indicator conditions and healthcare departments in which the largest numbers of missed opportunities occurred. This represents an essential step towards guiding the future drafting of diagnostic policies.
The data presented in this study show that most seropositive MSM came into contact with the healthcare system with symptoms indicative of HIV before they were diagnosed. This finding is similar to that presented in the only other study that analysed contacts with the healthcare system in the same time frame of reference as our study (five years before HIV diagnosis).23 However, comparing the two studies is a complex endeavour since that study had a population that did not consist entirely of MSM and only analysed contacts with primary care. Other studies that have also analysed this aspect21,23 have found much lower levels of contact with the healthcare system due in part to their shorter time frames of reference.
Most of the contacts reported by MSM analysed in this study occurred with healthcare departments not specific to HIV. This is essential because it is precisely in these contexts where the proportion of missed opportunities is highest and it clearly points to the fact that there is enormous potential for advancing the diagnosis in a substantial proportion of MSM who repeatedly visit this type of department. Even though the highest percentage of missed opportunities has previously been reported to be in non-specific departments,7,21 this is the first time that estimates have been given in a population consisting entirely of MSM. With the exception of tuberculosis, there were always fewer missed opportunities whenever the physician knew that the patient was an MSM, even though it must be acknowledged that in candidiasis differences were not significant. The fact that in tuberculosis the percentage of missed opportunities was similar (and also the lowest among all the conditions analysed) was probably due to the fact that the association between tuberculosis and HIV is strongly internalised in healthcare professionals and goes beyond risk groups. However, it was striking that the percentage of missed opportunities remained so high even when the healthcare professional knew that the patient had sex with other men. This could point to barriers to discussing topics related to the sexuality of MSM.18,24,25 This barrier, together with others such as a lack of awareness of diagnostic recommendations, a lack of time or uncertainty when dealing with topics related to HIV, have a particular impact on general healthcare departments, where HIV is not a highly prevalent condition.6,16,24 As a matter of fact, one of the main arguments for implementing and generalising testing due to indicator conditions is that it eliminates many of these barriers and makes it easier for healthcare professionals to offer the test in a standardised, efficient and ethical fashion.10
By indicator condition, we found that diarrhoea and non-specific fever for more than one month accounted for the highest percentages of missed opportunities. Both symptoms had a percentage of missed opportunities above 60%. Other symptoms, such as inflamed lymph nodes and weight loss exceeding 10%, had a percentage above 50%. The multiple causes underlying these symptoms may partly explain such high percentages. However, it should be noted that these symptoms may indicate acute infection, which must be detected to manage the epidemic, especially in groups with large numbers of sexual partners.26 Some experiences, such as the introduction of computerised warnings appearing on screen when the physician diagnoses and enters the code for any indicator condition, have shown promising results, tripling the proportion of patients with any indicator condition for whom HIV serology was ordered.27 This strategy could be considered particularly useful when the patient visits with non-specific symptoms that healthcare staff do not readily associate with HIV, especially those who work in low-prevalence contexts such as primary care and emergency care.27,28
Even though in relative terms STI had a lower percentage of missed opportunities among the conditions analysed, in absolute terms it accounted for the largest number of missed opportunities. This is particularly alarming since the link between STI and HIV has been known for many years. First, they share a route of transmission, and second, some ulcerative STIs exponentially increase the likelihood of transmitting HIV.29,30 It has already been reported that, of all the indicator conditions agreed upon by experts, STIs have by far the highest prevalence of HIV.20 In fact, the indication for HIV testing following diagnosis of an STI was the first recommendation issued 30 years ago (1987) .31 However, as other authors have also reported,6,32 the proportion of physicians who seem not to follow this recommendation still has plenty of room for improvement.
An important strength of our study is the fact that our survey respondents (966) represent approximately 15% of the target population, since it is estimated that between 2010 and mid-2013, 62731 new cases of HIV were diagnosed in MSM. Moreover, the use of an online survey made it possible to reach anybody, any time, anywhere, and its self-reporting nature protected the privacy and anonymity of the survey respondents. However, although Internet use is now very widespread in Spain, the survey necessarily excluded MSM with no Internet access and those who did not visit the websites used in the selection of the sample.
Our study also had several limitations. First, a memory bias may have affected the precision of the estimates. Some participants may have struggled to remember visits having occurred in the five years prior to diagnosis in detail or may not have clearly remembered whether or not they were offered HIV testing. Moreover, in some cases, visits due to indicator conditions may have given rise to subsequent visits in interdisciplinary settings and it is unknown whether HIV testing or even diagnosis occurred in the course of these referrals. In addition, the possibility that HIV testing was included in routine laboratory blood testing without the patient being certain of this could not be ruled out. However, we believe that these situations were anecdotal. Finally, it should be noted that most participants reported having been diagnosed before or during 2014, the year of publication of the Spanish guidelines recommending that HIV testing be offered if there is an indication or clinical suspicion of infection8; therefore, our study did not enable the degree of compliance to be evaluated. That being said, two years earlier, the recommendations agreed upon throughout Europe had already been disseminated among different scientific associations10 and translated into Spanish.33
Our study did enable assessment of the enormous potential of implementing HIV testing guided by indicator conditions for improving early detection of HIV in a healthcare setting. It also showed an urgent need to find solutions that make it possible to eliminate some of the barriers existing among healthcare professionals to promotion of testing as well as rigorous application of existing recommendations. Finally, promotion of HIV testing should be a priority in general healthcare departments such as primary care and emergency care, where the largest number of HIV indicator conditions are evaluated and, in turn, where the greatest proportion of missed opportunities for HIV testing occur.
FundingThe study was funded by the Ministerio de Sanidad, Servicios Sociales e Igualdad [Spanish Ministry of Health, Social Services and Equality] (MSSSI EC11-279) and the Consumers, Health, Agriculture and Food Executive Agency (2013 11 01).
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: Espinel M, Belza MJ, Cabeza-de-Vaca C, Arranz B, Guerras JM, Garcia-Soltero J, et al. La prueba del VIH orientada por condiciones indicadoras: oportunidades perdidas para adelantar el diagnóstico de la infección en hombres que tienen sexo con hombres. Enferm Infecc Microbiol Clin. 2018;36:465–471.